Energy and Weight control 2007
advertisement
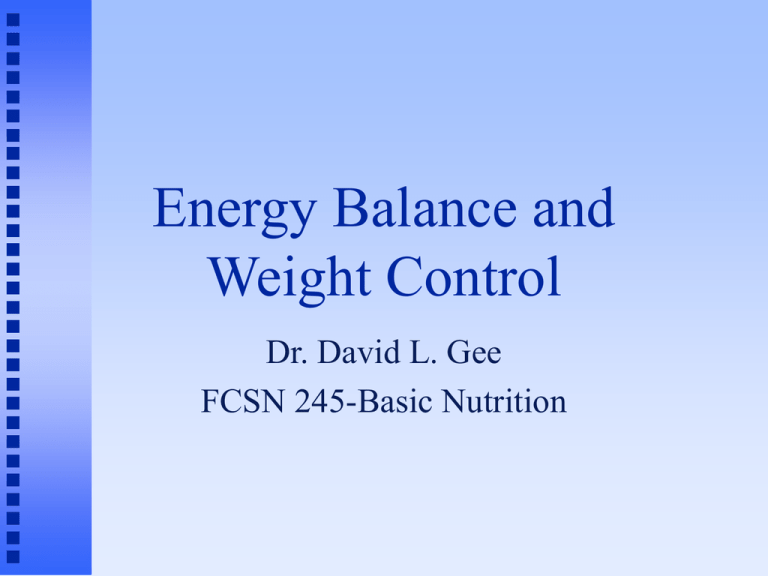
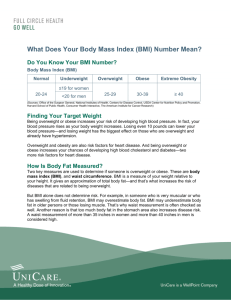
Energy Balance and Weight Control Dr. David L. Gee FCSN 245-Basic Nutrition Energy Balance EB = E(in) - E(out) E(in) = dietary intake of energy E(out) = energy expenditure Energy Balance: The Key to Weight Change When E(in) < E(out) Negative energy balance weight loss When E(in) > E(out) Positive energy balance weight gain When E(in) = E(out) Zero energy balance no weight change How do you measure: Energy (in) Calories = energy required to heat 1 kg water by 1 degree C. Bomb Calorimeter ©2001 Brooks/Cole, a division of Thomson Learning, Inc. Thomson Learning ™ is a trademark used herein under license. How do you measure: E(out) Direct Calorimetry measures heat directly bomb calorimeter (for food) room calorimeter Indirect Calorimetry measures oxygen consumed or carbon dioxide produced The effects of energy imbalance are cumulative!! If: +EB of 100 Cal/day Eat an additional cookie/day = +EB of 36,500 Cal/year If 1 lb fat = 3500 Cal Then see wt gain of 10 lbs per year !!! 36,500Cal/year / 3500 Cal/lb fat Therefore, knowing what affects energy balance is important Small consistent daily changes can accumulate to cause large weight changes Energy Out Components of E(out): Basal Metabolic Rate (BMR) Activity (Act) Thermic Effect of Food (TEF) E(out) = BMR + Act + TEF Basal Metabolic Rate Energy essential for life support Circulation Respiration Temperature Maintenance Nerve Transmission Kidney Function, etc Basal Metabolic Rate Estimation of BMR: BMR = 0.9 - 1 Cal / kg BW / hr Example: 120 lbs / 2.2 lbs/kg = 55 kg BMR = 55 x 1 x 24hr/d BMR = 1320 Cal / day Basal Metabolic Rate Factors affecting BMR Age BMR declines 2% per decade Height BMR related to body surface area Growth BMR highest during periods of growth Body Lean Composition tissue has higher metabolic rate than fat tissue Basal Metabolic Rate Factors affecting BMR Fever Increases by 7% per degree F. Stress Increases with physical stress (disease/trauma) Undernutrition Decreases with low calorie intake Energy for Activity Sedentary (adds 25-35% of BMR) Light (35-50%) Moderate (50-70%) Heavy (>70%) Example: Light Activity = 40% x 1320 = 530 Cal Moderate Activity = 60%x1320= 790 Cal Sedentary = 30%x1320= 396 Cal Change from Moderate to Sedentary Activity = gain 41 pounds of fat per year!! Thermic Effect of Food Increased energy expenditure after a meal. 5-10% Cost of BMR of digestion, absorption, & assimilation of nutrients Ex: 5% x 1320 = 60 Cal Estimation of E(out) E(out) = BMR + Act + TEF Example: E(out) = 1320 + 530 + 60 = 1910 Cal BMR = 69% of E(out) Act = 28% of E(out) TEF = 3% of E(out) Healthy Weight and the Non-Diet Approach David L. Gee, PhD Professor of Food Science and Nutrition Central Washington University Prevalence of Overweight in the US 1990: 56% of Americans were overweight 2000: 64% of Americans were overweight 30% were obese At this rate 23% were obese In 2010: 73% overweight In 2020: 84% overweight In 2030: 96% overweight Increases in overweight/obesity were seen in: Both males and females All age groups All ethnic groups The increase in prevalence in people with BMI > 25 was almost Entirely due to increased prevalence of obese!!! Overweight may be a transitional state for most Americans !!! Ethnicity and Overweight (BMI>27.5) Prevalence 70 66 63 60 50 45 42 40 % 30 24 27 31 40 34 26 20 10 0 White Black Hispanic Native Am Hawaiian Male Female Epidemic Increase in Childhood Overweight, 1986-1998 JAMA 286:2845-2848 (2001) National Longitudinal Survey of Youth 1986-1998 8,270 children, aged 4-12 yrs Prior studies show it took 30 years for overweight prevalence to double. Current study show doubling time to be less than 12 years. Rate of increase particularly high in African American and Hispanic children Prevalence of Overweight Children in the US Epidemic Increase in Childhood Overweight, 1986-1998 JAMA 286:2845-2848 (2001) Prevalence of overweight in children. CDC (2004) = above the 95th percentile for BMI based on NHANES II data from 1970’s For adolescents 12-19 yrs: Overweight 1974 = 7.4% 2002 = 15.6% Recent UW report (2007) that up to 25% of WA children are overweight. Genes/Biology vs Environment Overweight is a result of both Adoption studies (biology) Adopted adults have BMI that are more similar to biological parents than to adoptive parents. Animal studies (biology) genetically Genes obese rats and mice identified & biology explained Genes/Biology vs Environment (cont.) Migration studies (environment) Japanese Hawaiian Japanese Californian Japanese Dietary Change Studies (biology and environment) SW Native Americans Pima Indians Mexican Pima Indians subsistence farming & ranching 20% fat diet, 40 hrs/wk physical work Arizona Pima Indians mechanized agriculture, sedentary lifestyle 40% fat diet Pima Indians Arizona 1 Pima Indians are: inch taller 57 pounds heavier 70% obese 50% with diabetes by age 35 Genes vs Environment: Conclusions Genes for weight gain predisposes some individuals towards weight gain. Environment determines which of those individuals actually gain weight. Why lose weight? Obesity is associated with greater risk of: Diabetes Hypertension & stroke Coronary heart disease Most cancers (except lung cancer) Sleep apnea, arthritis, gall stones, …. Overfat vs Underfit ???? Good In question! reality: Vast majority of overfat are underfit Obesity and Causes of Death in the US The Cost of Obesity Health Affairs, Aug 2006 Year % of Medicare % of Medicare Patients with spending on obesity obese patients 1987 11.7% 9.4% 2002 22.5% 24.8% $336 billion 2005 total Medicare expenses What is a “Healthy Weight”? A broad range of weight which allows for minimal risks for chronic diseases. Goes beyond using only body weight as a criteria for good health. Determination of your "healthy weight". Step 1. Body Mass Index BMI = BW(kg)/Ht2(m2) Dr. Phil from Nutrition Action Health Letter, Jan. 2004 6‘4" = 78" x 0.0254(m/in)= 1.93m 240lbs / 2.2(lb/kg) = 109kg BMI = 109/(1.932)=109/3.72 = 29.3 BMI Classifications BMI = 19 - 25 => Desirable BMI = 25 - 30 => Overweight BMI = 30 - 35 => Obese, category 1 BMI = 35 - 40 => Obese, category 2 BMI > 40 => Severe obesity “Healthy weight is a broad range of weight…” For 5’10”, BMI 19-25 = 132 – 174 lbs Is BMI a good screening tool for weight problems? BMI measures degree of overWEIGHT BMI does not directly measure overFATNESS But…. Strong population-based relationship between high BMI and morbidity and mortality BMI a good predictor of overfatness in middleaged and older Americans BMI and Mortality Risk BMI and Prevalence of Low HDL NHANES III BMI and Prevalence of Hypertension Healthy Weight (cont.) If your BMI > 25, then consider presence of other health risk factors. Healthy Weight (cont.) Body Fat Distribution upper body fatness associated with higher health risks Waist Circumference (1998 NIH) > 35” for females, > 40” for males Healthy Weight (cont.): Know your blood lipids! Hyperlipidemia/dyslipidemia TC > 240 mg/dl LDL-C > 160 mg/dl HDL-C < 40 mg/dl TG > 200 mg/dl Healthy Weight (cont.): Know your blood pressure! High Blood Pressure Systolic BP > 140 mm Hg or Diastolic BP > 90 mm Hg or Borderline >130/85 or Pre-hypertensive Healthy Weight (cont.): Know your blood sugar and history Hyperglycemia (Diabetes) Fasting Blood Glucose > 126 mg/dl Impaired Glucose Tolerance Pre-diabetic >110 mg/dl Gestational Diabetes Family History of Diabetes Healthy Weight Summary If your BMI is 19-25, you are at a Healthy Weight. Health problems are not weight related If your BMI is > 25 and you have no other risk factors, you are at a Healthy Weight. If your BMI is > 25 and you have one or more risk factors, you are NOT at a Healthy Weight. Weight loss is likely to improve your health Should everybody who is overweight try to lose weight? Will weight loss improve your quality of life? A Prospective Study of Weight Change and Health-Related Quality of Life in Women JAMA Dec. 1999 Nurse’s Health Study 40,098 women, 4 yr longitudinal study Weight changes Quality of life questionnaire Physical function Vitality Freedom from bodily pain Mental health The effect of weight gain/loss on: Vitality Score Weight gain: associated with declines in vitality scores in all BMI categories Weight loss associated with improved vitality scores only in women with BMI>25 The effect of weight gain/loss on: Mental Health Score Weight gain associated with a decline in mental health scores in all weight categories Weight loss associated with improved mental health scores only in obese class I women and declined in normal weight women. A Prospective Study of Weight Change and Health-Related Quality of Life in Women. Conclusions: For women at all BMI categories: Don’t gain weight Reduced quality of life For overweight and obese women: Weight loss is generally associated with improved quality of life For normal weight women Weight loss does not improve quality of life May actually reduce quality of life The Obesity Epidemic in America: Who’s responsible? Personal responsibility Environmental influences Do we need a “Food Police”? http://www.nytimes.com/2005/06/12/business/yourmon ey/12food.html?pagewanted=1 Bottom Line on Weight Loss Lose weight for the right reasons Improve health and your quality of life Losing weight to attain the ‘perfect body’ May lead to frustration And, May ironically, weight gain lead to eating disorders Dietary Means to a Healthy Weight Weight loss occurs when in negative energy balance Weight loss is only half the battle Maintenance problem of weight loss is the critical Dietary Means to a Healthy Weight Balanced Reduced Calorie Diet Characteristics Calories reduced by 500-1000 Cal/day CHO:PRO:FAT = 50-60%: 10-15%: 20-30% Examples Weight Watchers, Jenny Craig, Slim Fast What the research shows: Short-term Modest weight loss, improved health Long-term outcomes outcomes Success rate not great Dietary Means to a Healthy Weight Low Carbohydrate Diets Characteristics Very low in CHO Restricted intakes of fruit, cereals, pasta, bread, potatoes, rice Caloric intake not specified Examples Atkins diet What the research shows: Short-term 6 month studies, good weight loss, no substantial change in heart disease risk factor, drop-out rate significant Long-term outcomes outcomes No long term studies, health risks?, 1 yr studies show more weight regain compared to low-fat diets Dietary Means to a Healthy Weight The Carbohydrate ‘Restrained’ Diets Characteristics Lower in CHO than Dietary Guidelines but higher than Low Carb diets (~40% CHO, 30%FAT, 30%PRO) Low glycemic index foods encouraged Monounsaturated fats encouraged Examples Zone Diet, South Beach Diet What the research shows: Little research available on these diets Dietary Means to a Healthy Weight Healthy Diet/Non-Diet Approach Characteristics Focus on quality of the diet, not quantity Attaining good health is primary goal, not weight loss Examples DASH diet, Dietary Guidelines, Food Guide Pyramid What the research shows: Short-term outcomes Slow, limited weight loss, health benefits Long-term outcomes U. Colorado’s Weight Loss Registry Diet most adopt in order to maintain weight loss Exercise and Weight Loss U. Colorado’s Weight Loss Registry Exercised used by nearly 100% Walking the most common form of exercise Benefits of Exercise Rate of weight loss greater Caloric restriction not as great Quality of weight loss better Proactive choice vs dieting Health benefits independent of weight loss Rates of physical inactivity in the US Exercise and Weight Loss Structured Exercise Aerobic Exercise Burns more calories, more fat Stress duration initially Strength Training Builds more lean tissue Increases basal metabolic rate Exercise for Weight Loss: Walking vs Running Going 4 miles Calories burned Walking @ 15min/mile 400 Cal Jogging @ 8 min/mile 400 Cal Fuels burned: CHO:FAT Calories CHO 50:50 75:25 200 Cal 300 Cal Calories FAT 200 Cal 100 Cal Exercise for Weight Loss: Walking vs Running Going 1 hour Distance covered Walking @ 15min/mile 4 miles Jogging @ 8 min/mile 7.5 miles Calories burned 400 Calories 750 Calories Fuels burned: CHO:FAT Calories CHO 50:50 75:25 200 Calories 560 Calories Calories FAT 200 Calories 190 Calories Exercise for Weight Loss: Walking vs Running Conclusions Walking and running burn the same number of calories over the same distance Walking burns more fat than running over the same distance Running burns calories at a faster rate and improves cardiovascular fitness more. Bottom line: Just do it! Either type of exercise is beneficial Exercise and Weight Loss Structured Exercise Characteristics of Successful Programs: Convenient Enjoyable Safe affordable Subject realizes net benefit over costs Exercise and Weight Loss Lifestyle Activity 24 hr day Sleep/rest = 10 hrs Structured exercise = 1 hr What you do the remaining 13 hrs of the day? Burn extra 25 Cal/hr = 325 Cal/day = 33 pounds of fat loss per year Develop a new attitude about being active Pedometers and 10,000 step programs Health benefits significant Weight Loss/Weight Maintenance Behavior/Attitude Changes Pay attention to what you eat Success Examine: Triggers for eating Emotional eating Risky of weight loss programs situations Behavior Modification Programs Track/record eating behaviors Identifies problems Sets goals and establishes rewards Continual reassessment/problem solving For more severe weight loss: Prescription Drugs For those with BMI > 30 or For those with BMI >27 and risk factors Meridia (Sibutramine, Abbott Lab) Suppresses appetite Xenical (Orlistat, Roche) Inhibits fat absorption Increases brain serotonin & norepinephrine levels – signal for satiety Reduces calories from fat containing foods Results in “adverse reactions” if eating high fat foods Long term success and risks Meridia – hypertension Xenical – steatorrhea (fatty diarrhea) For those with Severe Obesity Surgical Methods For those with BMI >40 Carnie Wilson Al Roker For those with Severe Obesity Gastroplasty Reduces size of stomach by banding or stapling Gastric Bypass Surgery Reduces size of stomach Bypasses much of the small intestine Outcomes Rapid and substantial weight loss Side effects Dangers Advice for the ‘typical’ CWU student: If you are at a healthy weight: Keep a close eye on your weight Preventing weight gain is far easier than trying to lose weight. If you are at an unhealthy weight: Don’t gain any more weight! If you try to lose weight Set reasonable goals (10% in 6 months) • Weight, diet, exercise Permanently change your lifestyle