Cranial Nerves
advertisement

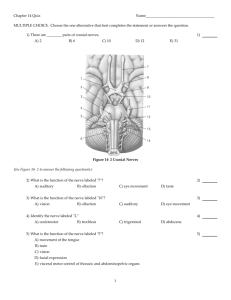
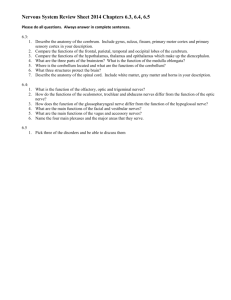
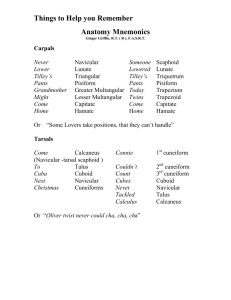
Cranial Nerves I Introduction • The head and neck are not innervated by spinal nerves; rather, they receive sensory information and send motor information via the 12 cranial nerves located in the brain. Although they are located within the skull, cranial nerves are considered part of the peripheral nervous system because they convey messages to and from the body's muscles and glands. Introduction • The cranial nerves function as modified spinal nerves. While all the spinal nerves convey both sensory and motor information, cranial nerves may carry solely sensory information, solely motor information, or both. Cranial nerves that have only a sensory or motor component can be called pure nerves ; nerves that have both components can be called mixed nerves . Introduction • The cranial nerve routes for sensory and motor circuits have different neuroanatomical connections. Sensory pathways are composed of 3 major neurons: the primary, the secondary, and the tertiary (see Figure 2). The cell bodies of primary neurons are usually located outside the CNS in sensory ganglia. They are homologous with the dorsal root ganglia of the spinal cord. The cell bodies of secondary neurons are in the dorsal gray matter of the brain stem, and their axons usually cross the midline and project to the thalamus. These are the actual sensory components of the cranial nerves. The cell bodies of the tertiary neurons are in the thalamus, and their axons project to the sensory cerebral cortex. There are two exceptions to this neuroanatomical scheme. Cranial nerves I and II (olfactory and optic) are special cases; the afferent fibers of their primary sensory neurons enter the brain stem and terminate on the secondary sensory neurons. Introduction • Motor pathways are composed of only two major neurons: the upper motor neuron and the lower motor neuron. The upper motor neuron is usually located in the cerebral cortex. It's axon projects caudally to contact the lower motor neuron. Most, but not all, of the motor pathways that terminate in the brain stem project bilaterally to contact lower motor neurons on both sides of the midline. The lower motor neuron is located in the brain stem. These are the actual motor components of the cranial nerves. Cranial Nerves • There are various mnemonics floating around to help students learn the cranial nerves. A few are shown below. Help for remembering the functions of each nerve are more mnemonics in the second table below. I Olfactory On Oh II Optic Old Oh III Oculomotor Olympus Oh IV Trochlear Towering To V Trigeminal Tops Touch VI Abducens A And VII Facial Frenchman Feel VIII Auditory &/or Vestibulococchlear And Very IX Glossopharyngeal German Green X Vagus Viewed Vegetables XI Spinal/Accessory Some Ah XII Hypoglossal Hops Heaven Cranial Nerves - S=Sensory; M=Motor; B=Both II III IV V VI VII VIII IX X XI XII Some Say Marry Money But My Brother Says Big Business Makes Money Some Say Marilyn Monroe But My Brother Says Bridget Bardoe Mmm Mmm I Cranial Nerve I: Olfactory Nerve • CN-I is a purely sensory nerve and serves the sense of smell. It originates in the olfactory cells of the nasal mucosa. Olfactory neurons are bipolar neurons that serve as the olfactory receptor. They are bathed by a layer of mucus where odorous substance dissolve into. Olfactory Nerve • Bundles of fibers collect information and pass it to the olfactory bulb, which continues in a caudal direction to the olfactory tract. The olfactory tract extends into the olfactory trigone, where olfactory tract splits into lateral olfactory stria and medial olfactory stria. Most of the olfactory tract pass into the lateral olfactory stria, which run into lateral olfactory area. Olfactory Nerve • Lateral olfactory area consists of the paleocortex of uncus, cortex of the entorhinal area (the anterior part of the parahippocampal gyrus) and the cortex in the region of the limen insulae. The uncus, cortex of the entorhinal area and cortex in the region of the limen insulae. The three parts are generally referred as pyriform cortex (pear shaped). Part of the amygdaloid body (amygdala) also is included in the lateral olfactory area. Lateral olfactory area is the principal region for the awareness of olfactory stimuli, so it is the primary olfactory area. • Because olfactory system shares entorhinal cortex with limbic system, which has extensive connections with the septal area and hypothalamus. The medial forebrain bundle contains fibers that connect septal area and hypothalamus with autonomic nuclei. Descending fibers from hypothalamus proceed to autonomic nuclei in the brain stem and spinal cord. So smell of food --> saliva secretion Olfactory Nerve • Fracture of the floor of anterior fossa could damage the olfactory nerves and causing anosmia (loss of smell), leakage of CSF from nose (cerebrospinal fluid rhinorrhea). Tumor can also block the olfactory pathway, likely to be unilateral. CN II: Optic Nerve • CN-II is also a purely sensory nerve serving the sense of vision. Photoreceptor, Rods, and cones receive light stimuli and transmitted as action potential to series layers of cells to ganglion cells. Rods is twenty times more than the number of cones. Rods is absent in the central fovea and gets more and more peripherally. It is more sensitive to dim light and responsible for peripheral vision. Cones is more sensitive to bright light and responsible for color vision. • Note that light and action potential travel at opposite directions. Action potentials generated from visual receptors pass via bipolar cells to ganglion cells, which axons bundle together to form the optic nerve. Optic Nerve • Optic nerve originates in the ganglion cells of the retina and travels to the optic chiasm , where the fibers from the medial half of each retina cross to the opposite side while those from the lateral half of the retina remain on the same side. Retinal projections • 1. Right half of two retinas terminate in the right lateral geniculate body and to right hemisphere. Left half of two retinas terminate in the left lateral geniculate body and to left hemisphere • 2. Upper quadrants peripheral to the macula (yellow spot) end in medial part of lateral geniculate, then project to anterior two thirds of visual cortex above calcrine sulcus • 3. lower quadrant peripheral to the macula end in lateral part of lateral geniculate, then project to anterior two thirds of visual cortex below calcrine sulcus. • 4. macula projects to a relatively large area on lateral geniculate body. Upper quadrant --> medial, lower quadrant --> lateral, posterior one third of the visual cortex Visual Field Projection • Visual field: • Retinal image in the visual field is inverted and reversed from right to left (can be trained the other way around) • 1. Left visual field is represented in the right lateral geniculate body and in the visual cortex of the right brain. • 2. Upper half of the visual field is represented in the lateral portion of the lateral geniculate body, below calcrine sulcus. • 3. lower half of the visual field is represented in the medial portion of the lateral geniculate body, above the calcrine sulcus Images projected from the visual field to the retina are inverted and reversed. Upper visual field goes to the lower retina, lower visual field goes to the upper retina Right visual field projects to the left hemiretina in each eye, left visual field projects to the right hemiretina Central fixation point for each eye falls on the fovea where highest visual acuity occurs Optic nerve • • surrounded by extension of meninges, so increased intracranial pressure can be presented by edema of optic disk (papilledema) Partial crossing: – determines binocular vision. Left visual field is represented in the right hemisphere Normal Papilledema Lateral geniculate • located in thalamus. Note that lateral geniculate body has six layers of cells and crossed and uncrossed optic tracts terminate into different layers of cells. Crossed fibers 1, 4, 6 and uncrossed fibers 2, 3, and 5. Geniculocalcarine tract • originate from lateral geniculate , two branches for upper visual field and lower visual field, terminate into visual cortex, which is located on the upper and lower lips of calcrine sulcus. There is a detailed point to point projection of the retina on the lateral geniculate body and on the visual cortex. Therefore, a right temporal lesion in the brain will affect the right lower quadrants of both eyes (retina or visual fields ?), and left upper visual fields will be affected. What about a right parietal lesion? Temporal lobe lesions can cause a contralateral homonymous superior quadrantopia visual field defect. Parietal lobe lesions can cause a contralateral homonymous inferior quadrantopia visual field defect Visual defect • Macular sparing – This is due to the fact that input from the center of the retina (the macula) is spread over a large portion of the optic radiation and primary visual cortex. Visual reflexes • Small bundle of fibers from optic nerve bypass lateral geniculate body and enter the superior brachium which connects with superior colliculus. Information can also be projected to pretectal area (group of small nuclei rostral to the superior colliculus. Pupillary light reflex • Information collected from retina could be relayed to olivary pretectal nucleus (one of those nuclei in the pretectal area) then to Edinger-Westphal, nucleus of oculomotor complex finally to the sphincter pupillae in the orbit and contracts pupils. Be aware that both eyes should reflex to light entering into one eye, that is because each retina sends fibers to both sides and pretectal area projects fibers cross to the contralateral side of the Edinger-Westphal nucleus. • Some retinal ganglion cells have axons enter the retinohypothalamic tract, the visual stimuli can synchronize the intrinsic circadian rhythm of the firing pattern of the neurons in suprachiasmatic nucleus. Then influence the antigonadotrophic activity of pineal gland. CN III, Oculomotor Nerve • CN-III is a purely motor nerve that serves to control all of the eye muscles except the lateral rectus and the superior oblique . It also contains parasympathetic fibers that control the ciliary muscle and pupillary constrictor muscles; when this part of the tract is damages, light shone in the affected eye does not cause constriction of the pupil. Somatic motor (general somatic efferent) Supplies four of the six extraocular muscles of the eye and the levator palpebrae superioris muscle of the upper eyelid. Visceral motor (general visceral efferent) Parasympathetic innervation of the constrictor pupillae and ciliary muscles. Eye Movements and Extraocular muscles Rectus Muscles Superior and Inferior Oblique Dual Actions of Superior Rectus Dual Actions of Superior Oblique Oculomotor nerve • Oculomotor nerve originates from oculomotor nucleus, which is located in the periaquductal gray matter of the midbrain (ventral to the aqueduct) at the level of superior colliculus. Oculomotor fibers are partially crossed and partially uncrossed. Current theory suggests that there are different nucleus groups to innervate different eye muscles. For instance, only uncrossed fibers innervate inferior rectus, inferior oblique, and medial rectus muscles. Superior rectus only innervated by crossed fibers Nerve Nuclei and Connections • There are two motor nuclei for the oculomotor nerve • The main motor nucleus is located in the anterior part of the grey matter surrounding the cerebral aqueduct of the midbrain at the level of the superior colliculus. All the extrinsic muscles of the eye except the superior oblique and the lateral rectus are supplied by this nucleus. The superior rectus muscle is supplied by the contralateral oculomotor nucleus, the remaining extraocular muscles are supplied ipsilaterally and the Lavator Palpebrae Superioris muscle of both sides are supplied by a single central group of cells called the central caudal nucleus. Nuclei and Connections • The accessory parasympathetic nucleus (EdingerWestphal nucleus) is located posteriorly to the main oculomotor nucleus • The preganglionic nerve cells from the Edinger-Westphal nucleus follow the same path as the other oculomotor fibres to the orbit where they synapse in the ciliary ganglion. The postganglionic fibres leave the ciliary ganglion and pass through the short ciliary nerves to the constrictor pupillae of the iris and the ciliary muscles. • The Edinger-Westphal nucleus receives fibres from the pretectal nucleus for the direct and consensual light reflex and corticonuclear fibres for the accommodation reflex. CN III • Oculomotor fibers are partially crossed and partially uncrossed. So damage to one side will not cause paralysis of all extraocular muscles. Interruption of the parasympathetic fibers from Edinger-Westphal nucleus, causes dilation of pupil. Light response and accommodation response will also be severed. The most common scenario is losing light reflex after head injury, because the oculomotor nerve is compressed over the tentorium cerebelli. Damage of CNIII • Ptosis or drooping of the upper eyelid • Dilation of the pupil. No reaction to light or accommodation • Overaction of the lateral rectus, superior oblique, inferior oblique • abnormal head posture Cranial Nerve IV: Trochlear Nerve • CN-IV is a small purely motor nerve which serves to control the superior oblique muscles of the eye. Paralysis of the superior oblique muscle results in extortion (outward rotation) of the affected eye, which is attributable to the unopposed action of the inferior oblique muscle. This gives rise to diplopia (double vision) and weakness of downward gaze; patients with trochlear nerve palsies often complain of visual difficulties when going down stairs Trochlear Nerve • The fourth cranial nerve innervates superior oblique muscle, which intorts, depresses, and abducts the globe • Trochlear Nerve Palsy – Patients often adopt a characteristic head tilt, away from affected side to reduce their diplopia. Interestingly, some patients develop head tilt toward side of lesion. This so-called paradoxic head tilt is used to create a wider separation of images, which allows the patient to suppress or ignore one image Cranial Nerve VI: Abducens Nerve • CN-IV is a purely motor nerve that serves to control the lateral rectus muscle of the eye. Paralysis of the lateral rectus muscle can result in strabismus , the inability to direct both eyes towards the same object. A patient with strabismus has diplopia, but can obtain normal binocular vision by moving the head so that the fixed, affected eye is brought into line with the object of interest. Common defects • Third cranial nerve palsy • 1. Drooping of the upper eyelid (ptosis) 2. Lateral strabismus: due to unopposed action from the lateral rectus muscle 3. Inability to direct the eye medially or vertically Common defects • Fourth Cranial Nerve palsy – diplopia going downstairs • Sixth cranial Nerve Palsy – 1. medial strabismus: – 2. inability to direct affected eye laterally • Positions of the eye in strabismus. A. Eyes are straight (orthophoria). B. Right eye turned in (right esotropia). C. Right eye turned up (right hypertropia). D. Right eye turned out (right exo-tropia). E. Right eye turned down (right hypotropia; however, convention calls for labeling up and down turns by the elevated eye, thus this would be properly termed left hypertropia). Cranial Nerve V: Trigeminal Nerve • CN-V is a large mixed nerve. The sensory component carries impulses from touch, pain, heat, and cold receptors of the facial area, the scalp, and the mucous membranes. The motor component innervates the muscles of mastication (chewing). Sensory components • Trigeminal nerve has three large branches, ophthalmic, maxillary and mandibular. They innervate the skin of face (no overlapping), scalp, mucus membrane of oral and nasal cavities, paranasal sinuses and teeth. • Primary sensory neurons are in the trigeminal ganglion, others are in the mesencephalic trigeminal nucleus. The peripheral processes of trigeminal ganglion cells constitute the ophthalmic and maxillary nerves (sensory only) and the sensory component of the mandibular nerve (mixed). Trigeminal nerve • Axons of the trigeminal ganglion cells enter the pons and terminate in the pontine and spinal trigeminal nuclei. • Pontine trigeminal nucleus: large sensory root for discriminative touch • Spinal trigeminal nuclei: light touch Spinal trigeminal tract and its nucleus • Spinal trigeminal tract: – Medium and fine fibers that carry touch, pain, and temperature info form the spinal trigeminal tract. Fibers from facial, glossopharyngeal, and vagus nerves are also joining the tract carrying in general somatic sensation from external ears, posterior part of the tongue, pharynx, and larynx. – Fibers of spinal trigeminal tract then terminate onto adjacent spinal trigeminal nucleus which is subdivided into pars caudalis (receives fibers for pain and temperature), pars interpolaris (light touch, pain maybe), and pars oralis (discrimitive touch) and reticular formation (source of cutaneous stimuli to maintain arousal and alertness) Projections from above nucleus • ventral trigeminothalamic tract: crossed – small number of fibers from pontine nucleus (both crossed and uncrossed) proceed to thalamus via dorsal trigeminothalamic tract • The combined ventral and dorsal trigeminal trigeminothalamic tracts form the trigemical lemniscus. These axons end in the medial division of Ventral Posterior Nucleus of Thalamus, then project to primary somatosensory region • Some efferent fibers from sensory trigeminal nuclei terminate into motor nuclei of other cranial nerves, like facial, and hypoglossal nerves. They are responsible for reflexes, i.e. corneal reflex: touch on cornea transmits info via opthamic nerve of trigeminal, the efferent fiber, however, is in facial nerve. Mesencephalic trigeminal nucleus • Extending from the potine trigeminal nucleus into the midbrain. The axons from these nucleus form the mesencephalic root. Each axon splits into peripheral and central branch. The peripheral branch runs with mandibular nerve collecting proprioceptive info and ending in muscle spindles. Central branch terminates in the motor nuclei of the trigeminal nerve. The connection controls the force of mastication. Motor component of trigeminal nerve • Generate from trigeminal motor nucleus, joins mandibular branch, supplies muscles of mastication (masseter, temporalis, lateral and medial pterygoid muscles) and smaller muscles like tensor tympani, digastric anterior, and mylohoid. Descending fibers come from corticobulbar tract. Most of the fibers are crossed for the contralateral control, however, significant number of fibers do not cross. Therefore, damage of one side of the corticobulbar tract will only cause contralateral weakness of chewing, but not completely paralyzed n. Clinical significance • Trigeminal neuralgia (tic douloureux) – Tic douloureux or trigeminal neuralgia is a severe, stabbing pain to one side of the face. It stems from one or more branches of the nerve that supplies sensation to the face, the trigeminal nerve. It is considered one of the most painful conditions to affect people. – Pain is usually triggered by a light touch of the face or mouth on the same side as the pain Trigeminal neuralgia (tic douloureux) • Cause unknown – compression of the trigeminal nerve – Tumors and bony abnormalities of the skull – Trauma, infections, and multiple sclerosis can also cause damage to the trigeminal nerve • Treatment – Pain management – Surgery Shingles (Herpes Zoster) • Shingles – The ophthalmic division of the trigeminal nerve is affected – Caused by varicella-zoster virus, the same virus that causes chickenpox. After an attack of chickenpox, the virus lies dormant in the nerve tissue. As we get older, it is possible for the virus to reappear in the form of shingles