The “Top 10” - Heart Disease Prevention Program
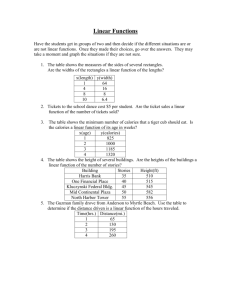
advertisement

Obesity
A Weighty Problem
The “Top 10”
The Associated Press
The “Top 10” alternative reasons for
obesity:
1. Inadequate sleep. (Average sleep amounts
have fallen, and many studies tie sleep
deprivation to weight gain.)
The “Top 10” alternative reasons for
obesity:
2. Endocrine disruptors, which are substances
in some foods that might alter fats in the
body.
The “Top 10” alternative reasons for
obesity:
3. Nice temperatures. (Air conditioning and
heating limit calories burned from
sweating and shivering.)
The “Top 10” alternative reasons for
obesity:
4. Fewer people smoking. (Less appetite
suppression.)
The “Top 10” alternative reasons for
obesity:
5. Medicines that cause weight gains
The “Top 10” alternative reasons for
obesity:
6. Population changes. (More middle-agers
and Hispanics, who have higher obesity
rates.)
The “Top 10” alternative reasons for
obesity:
7. Older birth moms. (That correlates with
heavier children.)
The “Top 10” alternative reasons for
obesity:
8. Genetic influences during pregnancy
The “Top 10” alternative reasons for
obesity:
9. Darwinian natural selection. (Fat people out
survive skinny ones).
The “Top 10” alternative reasons for
obesity
10. Assortative mating, or like mating with
like,” Allison puts it. Translation: fat people
procreating with others of the same body
type, gradually skewing the population
toward the heavy end.
Obesity Related Morbidity
• The estimated number of deaths attributable to
obesity among US adults is approximately
280,000.
Obesity Related Morbidity
• The estimated number of deaths attributable to
obesity for nonsmokers is approximately 325,000
Obesity
• AHA and NIH have recognized obesity as a major modifiable risk
factor for CHD
• Obesity is a risk factor for development of hypertension, diabetes,
and dyslipidemia
• Obesity also linked to insulin resistance, particular intraabdominal fat
estimated by waist circumference
The Theories of Obesity Fall Into
Three Categories
Genetic Influence of Human Variation
in Body Fat
Defining Obesity
• Body Mass Index (BMI)= Weight divided
by Height squared (kg/m 2).
• Normal Weight: 18.5 to 24.9
• Overweight: 25.0 to 29.9
• Obese I: 30.0 to 34.9
• Obese II: 35.0 to 39.9
• Obese III: > 40
Relationship Between Cardiovascular Disease
and Their Risk Factors
Disease Risk Associated with
Overweight and Obesity
• “Disease risk in early life is associated with
respiratory conditions and several risk factors for
coronary heart disease and is predictive of
hypertension, diabetes, coronary heart disease and
all-cause mortality.”
• Other risk factors include certain types of cancers,
high blood cholesterol level, gall bladder disease,
and osteoarthritis.
Prevalence and Risk of Obesity
• NHANES III shows approximately 60% of men and 50%
of women are obese or overweight, with 20% of men and
25% of women having a BMI of 30 or greater
• BMI 27-29 associated with a RR of total mortality of 1.6,
BMI 29-32 RR 2.1, and BMI >=32 RR 2.2 vs. BMI <19
from Nurses’ Health Study.
Increasing Prevalence of Overweight
and Obesity
• Obesity has increased in every state, in both sexes,
across all age groups, educational levels, and
smoking statuses.
• Over the last 3 decades there has been a 25%
increase in the number of people who qualify as
overweight.
Percentage of Overweight and
Obesity in the United States
• For adults 25 years and older the percentage
of people who qualify as overweight is 63%
for men and 55% for women.
• Specifically, 42% of men and 28% of
women are overweight. While 21% of men
and 27% of women are obese.
Prevalence of Obesity among US Adults From
Years 1991, 1993, 1995, and 1998
Prevalence of Obesity among US Adults From
Years 1991, 1993, 1995, and 1998
Increasing Prevalence of Overweight in
U.S. Adults and
of Obesity
Age-Adjusted Standardized Prevalence of Overweight
(BMI 25–29.9) and Obesity (BMI >30)
24
.9
16
.3
16
.1
15
.1
12
.2
10
.4
20
11
.8
19
.9
24
.7
24
.3
23
.6
39
.4
39
.1
30
23
.6
Percent
40
37
.8
50
41
.1
NHES I NHANES I NHANES II NHANES III
10
0
Men
Women
BMI 25–29.9
CDC/NCHS, United States, 1960-94, ages 20-74
years
Men
BMI > 30
Women
NHANES III Age-Adjusted Prevalence of
Hypertension* According to BMI
BMI <25 BMI 25-26 BMI 27-29 BMI >30
50
38.4
Percent
40
32.2
30
22.5
20
25.2
18.2
21.9
24.0
16.5
10
0
Men
Women
*Defined as mean systolic blood pressure 140 mm Hg, as mean diastolic
90 mm Hg, or currently taking antihypertensive medication .
Brown C et al. Body Mass Index and the prevalence of
Risk Factors for Cardiovascular Disease (in preparation).
NHANES III Age-Adjusted Prevalence of
High Blood Cholesterol* According to BMI
BMI <25
BMI 25-26
BMI 27-29
BMI >30
50
Percent
40
27.9
30
20
14.7
17.5
20.4
28.2
20.2
15.7
10
0
Men
*Defined as > 240
mg/dL.
Brown C et al. Body Mass Index and the
Prevalence of Risk Factors for Cardiovascular
Disease (in preparation).
Women
24.7
NHANES III Age-Adjusted Prevalence of
Low HDL-Cholesterol* According to BMI
BMI <25 BMI 25-26 BMI 27-29 BMI >30
60
Percent
50
41.5
40
31.4
30
23.1
17.2
20
10
27.0
27.2
16.5
9.1
0
Men
*Defined as <35 mg/dL in men and <45 mg/dL in
women.
Brown C et al. Body Mass Index and the
Prevalence of Risk Factors for Cardiovascular
Disease (in preparation).
Women
Carbo-Lipo-Terrorism in the U.S.
A Report To:
Orange County
On: 2/18/04
Percent Overweight (>95% weight/height)
Percent Overweight Children
U.S. & Orange County
16
14
U.S. 6-11 yo
12
10
U.S.12-19 yo
8
6
Orange County
2-12 yo
4
2
0
1963-70 1971-74 1976-80 1988-94
Year
19992000
Data from the CDC & Prevention, NCHS, NHANES, HHNES, NHES, Report on
the Conditions of Children in Orange County, 2002
Obesity (> 120%tile
ideal body weight)
in U.S. Adults
1992
Diabetes in U.S Adults
1992
No Data
<4%
4%-6%
6%-8%
8%-10%
>10%
Obesity
1994
Diabetes
1994
No Data
<4%
4%-6%
6%-8%
8%-10%
>10%
Obesity
1996
Diabetes
1996
No Data
<4%
4%-6%
6%-8%
8%-10%
>10%
Obesity
1998
Diabetes
1998
No Data
<4%
4%-6%
6%-8%
8%-10%
>10%
Obesity
1999
Diabetes
1999
No Data
<4%
4%-6%
6%-8%
8%-10%
>10%
Obesity
2000
Diabetes
2000
No Data
<4%
4%-6%
6%-8%
8%-10%
>10%
Tracking BMI-for-Age from Birth to 18 Years with
% of Overweight Children who Are Obese at Age 25
100
BMI < 85th
BMI >=85th
BMI >=95th
% obese as adults
83
80
69
60
77
75
67
55
52
36
40
26
20
16 17
15
19
12
11
10
9
10 to 15
15 to 18
0
Birth
Whitaker et al. NEJM:
1997;337:869-873
1 to 3
3 to 6
6 to 10
Age of child (years)
BMI-for-Age Cutoffs
> 95th percentile
Overweight
85th to < 95th
percentile
Risk of overweight
< 5th percentile
Underweight
National Longitudinal Survey of Youth
Prospective Cohort Study of
8270 Children (4-12 years old) - 1999
Risk of Overweight Overweight
> 85th %ile BMI
> 95th %ile
BMI
African American
Hispanics
Caucasian
38.4%
37.9%
25.8%
21.5%
21.8%
12.3%
Secular Increases in Relative Weight and
Adiposity in Children (5-14 years old)
- Bogalusa Heart Study Weight (kg)
Height
(cm)
BMI
(kg/m2)
1973-1974
35.9
140
17.6
1992-1994
41.0
142
19.5
+1.6
+1.5
Study years
* Change
adjusted for height, age, +3.4
race, and sex
Change*
Source: Pediatrics 99:420-426, 1997
Prevalence of Overweight and Obesity
Among US Children (6-19 years old)
1999-2002
1999-2000
2001-2002
85th percentile BMI
29.9%
31.5%
95th percentile BMI
15.0%
16.5%
Source: Hedley et al., JAMA 291:2847-2850, 2004
Overweight in Children*
(> 95th percentile BMI)
1971-1974
1988-1994
1999-2002
2-5 years
5.0
7.2
10.4
6-11 years
4.0
11.3
15.3
12-19 years
6.1
10.5
15.5**
* 4722 children from NHANES; overweight > 95th adjusted for age
** > 23% of African American and Mexican American adolescents
Source: Ogden et al., JAMA 288:1728-1732, 2002
Correlations of Weight and BMI
at 7.7 and 23.6 Years
r=0.605
r=0.612
Source: Minneapolis Children’s BP Study, Circulation 99:1471, 1999
For Children, BMI Changes with Age
BMI
BMI
Example: 95th
Percentile
Tracking
Boys: 2 to 20 years
BMI
BMI
Age
BMI
2 yrs
4 yrs
9 yrs
13 yrs
19.3
17.8
21.0
25.1
BMI Changes with age
BMI
BMI
Boys: 2 to 20 years
BMI = 18
Age 4 years: >95th
Age 8 years: 85th
Age 13 years: <50th
BMI
BMI
Can you see risk?
• This boy is 3 years, 3 weeks
old.
• Is his BMI-for-age
- >85th to <95th percentile:
at risk for overweight?
Photo from UC Berkeley Longitudinal Study,
1973
Plotted BMI-for-Age
BMI
BMI
Boys: 2 to 20 years
Measurements:
Age=3 y 3 wks
Height=
100.8 cm (39.7 in)
Weight=
18.6 kg (41 lb)
BMI = 18.3
BMI
BMI
BMI-for-age=
>95th percentile
overweight
Can you see risk?
• This girl is 4 years old.
• Is her BMI-for-age
- >85th to <95th percentile:
at risk for overweight?
Photo from UC Berkeley Longitudinal Study,
1973
Plotted BMI-for-Age
BMI
BMI
Girls: 2 to 20
years
Measurements:
Age=4 y
Height=
99.2 cm (39.2 in)
Weight=
17.55 kg (38.6 lb)
BMI=17.8
BMI
BMI
BMI-for-age=
between 90th –95th
percentile
At risk for overweight
Accurate Measurements are Critical
BMI
BMI
Boys: 2 to 20 years
5 1/2 year old boy
Weight: 41.5 lb
Height: 43 in
BMI= 15.8
BMI-for-age=50th %tile
Inaccurate height
measurement: 42.25
BMI=16.3
BMI-for-age=75th %tile
BMI
BMI
Childhood Overweight 2003
BMI (Body Mass Index) is Now Defining Tool
•
•
•
•
•
BMI Calculated as
Weight / Height Squared
Used to judge appropriateness
of weight for height
Replaces weight for height
charts and % ideal body wt
For a child, BMI > 95% is obese
BMI 85-95% is “at risk”
BMI data from retrospective analysis:
1. Reflect increasing fatness
2. Predict adult risk
Prevalence of Overweight, U.S. Adults, 1988 to 1991
Overweight Adults 20-74 Years of
Age, 1988-1994
Overweight Prevalence by
Race/Ethnicity for Adolescent Boys
and Girls
Targeted History & Physical for
the Obese Child
The Identification, Management &
Treatment of the Obese Child
History
• Birth
– Weight: LGA & SGA
• Risk factor for Diabetes Mellitus
– Decreased tone, poor feeding
• Concern regarding Prader Willi
• Family History (below are RF for DM & dysmetabolic syndrome)
–
–
–
–
–
Diabetes (1 vs 2, gestational)
Obesity (calculate parents BMI)
Hypertension
Dyslipidemia
Premature cardiovascular disease
Male < 55 yo
Female < 65 yo
Medical history/Review of Systems
Possible Underlying Endogenous Cause of
Obesity
• Decreased growth velocity or abnormal height
• Abnormal pubertal development
• Abnormal Developmental history
– Prader Willi, Bardet Biedl, Sotos
• Dysmorphic Features
• Hypothyroidism: cold, fatigue, dry skin, hair loss, constipation
Medical History/Review of Systems for
the Obese Child
• Sleep
– snoring, stops breathing, daytime sleepiness
• Menstrual History
– Amenorrhea, Irregular Menses
• Leg pain
•
•
•
•
– Hip, knee, tibial (SCFE, Blounts)
Blood pressure
Lipid Levels
Recurrent yeast infections
Polyuria, Polydipsia
Directed Exam for Obese Youth
•Ht____cm
Wt_____Kg
BMI (kg/m2)____
(>85%Dietician) (BMI>40 or > 95%Endo)
•BP_____ (HTN: Y/N)
•Dyspnea at rest vs exertion
•Tanner stage____
•Normal Pubertal development: Y/N
•Skin: Acanthosis: Y/N Hirsutism: Y/N
•Ext: Hip, knee, valgus or varus deformity
The A, B, C Intervention
•
•
•
Activity
1.
2.
Minimum of 60 min/day of minimum intensity of a brisk walk.
Limit screen time (not associated with school work) < 1 hour
Beverages
1.
2.
3.
No regular soda or sugar/corn syrup sports drinks/punch
< 6 ounces juice/day
Increase water & non-or low fat milk (or other calcium containing food)
consumption
Change=Goal
1.
2.
3.
Family changes eating & activity habits
Reasonable, achievable, step wise goals
Minimum nursing visits every 3-4 months: check progress & reinforce
goals. Phone follow-up
Who to Test for IGT & Diabetes
• Obese: BMI>85%
• Age: Earliest of the following, > 10 years of age or onset of
puberty
• And 2 of the following:
– Family history of T2DM in 1st or 2nd degree relative
– Ethnicity: Native American; African-American; Latino; Asian; Pacific
Islander
– Conditions assoc. with or signs of insulin resistance: acanthosis
nigricans; hypertension, dyslipidemia, PCOs
Based on ADA Recs: Diabetes Care 2003
Impaired Glucose Tolerance & Diabetes
Normal
IFG or IGT
FPG <100 mg/dl
FPG= 100 - 125 mg/dl
(IFG)
2-h PG <140 mg/dl
Diabetes
FPG > 126 mg/dl
2-h PG=140- 199mg/dl 2-h PG > 200 mg/dl
(IGT)
Symptoms of diabetes &
casual plasma glucose
concentration 200 mg/dl
In the absence of unequivocal hyperglycemia, a diagnosis of diabetes must be
confirmed, on a subsequent day, by measurement of FPG, 2-h PG, or random plasma
glucose (if symptoms are present). The FPG test is greatly preferred because of ease of
administration, convenience, acceptability to patients, and lower cost. Fasting is defined
as no caloric intake for at least 8 h.
This test requires the use of a glucose load containing the equivalent of 75 g anhydrous
glucose dissolved in water. 2-h PG, 2-h postload glucose
Based on ADA Recs: Diabetes Care 2004
Do You Know How Food Portions Have
Changed in 20 Years?
National Heart, Lung, and Blood Institute
Obesity Education Initiative
BAGEL
20 Years Ago
140 calories
3-inch diameter
Today
How many calories
are in this bagel?
BAGEL
20 Years Ago
140 calories
3-inch diameter
Today
350 calories
6-inch diameter
Calorie Difference: 210 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to rake leaves in order to
burn the extra 210 calories?*
*Based on 130-pound person
Calories In = Calories Out
If you rake the leaves for 50 minutes you will
burn the extra 210 calories.*
*Based on 130-pound person
CHEESEBURGER
20 Years Ago
333 calories
Today
How many calories are
in today’s cheeseburger?
CHEESEBURGER
20 Years Ago
Today
333 calories
590 calories
Calorie Difference: 257 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to lift weights
in order to burn the extra 257 calories?*
*Based on 130-pound person
Calories In = Calories Out
If you lift weights for 1 hour and 30 minutes,
you will burn approximately 257 calories.*
*Based on 130-pound person
SPAGHETTI AND MEATBALLS
20 Years Ago
500 calories
1 cup spaghetti with sauce
and 3 small meatballs
Today
How many calories do
you think are in today's
portion of spaghetti and
meatballs?
SPAGHETTI AND MEATBALLS
20 Years Ago
500 calories
1 cup spaghetti with sauce
and 3 small meatballs
Today
1,025 calories
2 cups of pasta with sauce
and 3 large meatballs
Calorie Difference: 525 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to houseclean in order
to burn the extra 525 calories?*
*Based on 130-pound person
Calories In = Calories Out
If you houseclean for 2 hours and 35 minutes,
you will burn approximately 525 calories.*
*Based on 130-pound person
FRENCH FRIES
20 Years Ago
Today
210 Calories
2.4 ounces
How many calories are in
today’s portion of fries?
FRENCH FRIES
20 Years Ago
210 Calories
2.4 ounces
Calorie Difference: 400 Calories
Today
610 Calories
6.9 ounces
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to walk leisurely in
order to burn those extra 400 calories?*
*Based on 160-pound person
Calories In = Calories Out
If you walk leisurely for 1 hour and 10 minutes
you will burn approximately 400 calories.*
*Based on 160-pound person
SODA
20 Years Ago
85 Calories
6.5 ounces
Today
How many calories are
in today’s portion?
SODA
20 Years Ago
85 Calories
6.5 ounces
Today
250 Calories
20 ounces
Calorie Difference: 165 Calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to work in the garden to
burn those extra calories?*
*Based on 160-pound person
Calories In = Calories Out
If you work in the garden for 35 minutes,
you will burn approximately 165 calories.*
*Based on 160-pound person
TURKEY SANDWICH
20 Years Ago
320 calories
Today
How many calories are in
today’s turkey sandwich?
TURKEY SANDWICH
20 Years Ago
320 calories
Today
820 calories
Calorie Difference: 500 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to ride a bike in order to
burn those extra calories?*
*Based on 160-pound person
Calories In = Calories Out
If you ride a bike for 1 hour and 25 minutes,
you will burn approximately 500 calories.*
*Based on 160-pound person
Thank you for participating in
Portion Distortion!
For more information about Maintaining a Healthy Weight
visit www.nhlbi.nih.gov
TOO MUCH SODA
Coke glass bottle (8 fl. oz.) = 100
kcals.
Coke can (12 fl. oz) = 150 kcals.
Coke plastic bottle (20 fl. oz. ) = 250
kcals.
Super Big Gulp (44 fl. oz.) = 550
kcals.
***1 big gulp a day = 57
pounds /year!!!!
What does the future hold??
Do You Know How Food Portions Have
Changed in 20 Years?
National Heart, Lung, and Blood Institute
Obesity Education Initiative
COFFEE
20 Years Ago
Today
Coffee
(with whole milk and sugar)
Mocha Coffee
(with steamed whole milk and
mocha syrup)
45 calories
8 ounces
350 calories
16 ounces
Calorie Difference: 305 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to walk in order
to burn those extra 305 calories?*
*Based on 130-pound person
Calories In = Calories Out
If you walk 1 hour and 20 minutes, you
will burn approximately 305 calories.*
*Based on 130-pound person
MUFFIN
20 Years Ago
210 calories
1.5 ounces
Today
How many calories are
in today’s muffin?
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to vacuum in
order to burn those extra 290 calories?*
*Based on 130-pound person
Calories In = Calories Out
If you vacuum for 1 hour and 30 minutes you
will burn approximately 290 calories.*
*Based on 130-pound person
PEPPERONI PIZZA
20 Years Ago
500 calories
Today
How many calories are in
two large slices of today’s
pizza?
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to play golf (while
walking and carrying your clubs) in order
to burn those extra 350 calories?*
*Based on 160-pound person
Calories In = Calories Out
If you play golf (while walking and carrying your
clubs) for 1 hour you will burn approximately 350
calories.*
*Based on 160-pound person
CHICKEN CAESAR SALAD
20 Years Ago
390 calories
1 ½ cups
Today
How many calories are in
today’s chicken Caesar
salad?
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to walk the dog in
order to burn those extra 400 calories?*
*Based on 160-pound person
Calories In = Calories Out
If you walk the dog for 1 hour and 20 minutes,
you will burn approximately 400 calories.*
*Based on 160-pound person
POPCORN
20 Years Ago
270 calories
5 cups
Today
How many calories
are in today’s large
popcorn?
POPCORN
20 Years Ago
Today
270 calories
5 cups
630 calories
11 cups
Calorie Difference: 360 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to do water
aerobics in order to burn the extra 360
calories?*
*Based on 160-pound person
Calories In = Calories Out
If you do water aerobics for 1 hour and 15
minutes you will burn approximately 360 calories.*
*Based on 160-pound person
CHEESECAKE
20 Years Ago
Today
260 calories
3 ounces
640 calories
7 ounces
Calorie Difference: 380 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to play tennis in
order to burn those extra 380 calories?*
*Based on 130-pound person
Calories In = Calories Out
If you play tennis for 55 minutes you
will burn approximately 380 calories.*
*Based on 130-pound person
CHOCOLATE CHIP COOKIE
20 Years Ago
55 calories
1.5 inch diameter
Today
How many calories are
in today’s large cookie?
CHOCOLATE CHIP COOKIE
20 Years Ago
55 calories
1.5 inch diameter
Today
275 calories
3.5 inch diameter
Calorie Difference: 220 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to wash the car to
burn those extra 220 calories?*
*Based on 130-pound person
Calories In = Calories Out
If you wash the car for 1 hour and 15 minutes you
will burn approximately 220 calories.*
*Based on 130-pound person
CHICKEN STIR FRY
20 Years Ago
435 calories
2 cups
Today
How many calories are in
today’s chicken stir fry?
CHICKEN STIR FRY
20 Years Ago
435 calories
2 cups
Today
865 calories
4 ½ cups
Calorie Difference: 430 calories
Maintaining a Healthy Weight is a Balancing Act
Calories In = Calories Out
How long will you have to do aerobic
dance to burn those extra 430 calories?*
*Based on 130-pound person
Calories In = Calories Out
If you do aerobic dance for 1 hour and 5 minutes
you will burn approximately 430 calories.*
*Based on 130-pound person
Thank you for participating in
Portion Distortion II!
For more information about Maintaining a Healthy Weight
visit www.nhlbi.nih.gov
KID FRIENDLY SNACKS?
Super Pretzel and
16 fl. oz. Snapple Fruit
Punch = 630 kcals.
24 fl. oz. Banana Berry
Jamba Juice = 470 kcals.
Venti Vanilla Creme
Frappacchino = 870
kcals.
WHAT ABOUT SCHOOL?
PRACTICAL SUGGESTIONS
Encourage parents to limit contribution of calories
from beverages (only milk required).
Encourage 5 a day program.
Suggest Stoplight Diet (Epstein)
Stress Family Commitment- entire family needs to
follow new eating habits.
FAST FOOD MAKEOVERS
Big Mac Value Meal = 1250 kcals.
If you super size….. Add 360 kcals!
Hamburger Happy Meal with regular
coke = 640 kcals.
If you switch to diet or water
subtract 150 kcals.
FAST FOOD MAKEOVERS
Del Taco Combo
Burrito Meal =
1090 kcals.
2 Del taco soft
chicken tacos = 320
kcals.
SERVING SIZES
GRAIN = 1 slice of
bread, ½ cup
cooked rice or
pasta.
FRUIT = 1 piece of
fruit, ¾ cup juice.
VEGETABLE = ½
cup cooked or 1 cup
raw.
MILK = 1 cup milk
MEAT = 2-3 oz.
cooked lean meat or
fish.
FATS and
SWEETS: use
sparingly.
Cardiovascular Complications of
Obesity
The Identification, Management and
Treatment of the Obese Child
Jody Kranz M.D.
Div. Endocrinology & Diabetes
CHOC
Stan Bassin Ed.D
Div. Cardiology
UCI
Cardiovascular Complications of
Obesity
• Cardiovascular Disease (CVD)
–
–
–
–
Atherosclerosis
Obesity
Hypertension
Lipids
• Inflammatory Factors
• Homocysteine & Other Risk Factors
• Guidance for Practitioners
– Guidelines/Schedule for cardiovascular health
– Proper blood pressure measurement
– Charts for determining hypertension
Cardiovascular Disease
• Leading cause of death in the United States
– Half a million deaths year
• Atherosclerosis: disease of large & medium
sized vessels that leads to decrease blood
flow to the myocardium, brain and
extremities.
• Atherosclerosis begins in childhood
– Same risk factors as in adults
Atherosclerosis Begins in
Childhood
PDAY-Pathologic Determinants of Atherosclerosis in Youth
Autopsy Evaluations of CVD Risk Factors
Progression of atherosclerosis from fatty streaks to raised
lesions in persons > 15 years of age
10-20% of 15-19 year olds have intermediate lesions
Risk factors:
High non-HDL cholesterol
Smoking
HbA1C > 8%
Low HDL cholesterol
Hypertension
Obesity (BMI > 30 kg/m2)
Atherosclerosis Risk
Factors
– Increasing
Blood Pressure
– Dyslipidemia
– Inflammatory
factors
– Homocysteine
– Diabetes
– Tobacco
exposure
– Family History
– Male gender
– Obesity
– Sedentary
Lifestyle
Obesity & Hypertension
Clinical Presentation of Hypertension
• High blood pressure = BP > 90th percentile for age
gender and height.
• Hypertension= BP > 95th percentile for age, gender and
height.
• Primary Hypertension
– most common cause of Hypertension in Children over 6 years of
age
<6 years of age
• Secondary Hypertension
– Renal disease
– Aortic Coarctation
• Primary isolated systolic
– Isolated systolic hypertension is an independent risk factor for
cardiovascular disease
– 50% prevalence in obese
Percent with Hypertension (%)
Prevalence of Hypertension in Children
vs Distribution of BMI (%)
50
40
34
30
23
20
10
6
5
6
<5
10
25
11
12
50
75
0
BMI centile
90
>95
Blood Pressure & CVD
• Blood pressure is positively correlated with cardiovascular
risk across the entire BP range
– Evidence from autopsy studies
– Increase in carotid intima media thickness in adolescents with
hypertension
• Increase in Left Ventricular Mass/ Mass index indicating
hypertrophy
• There is a synergistic effect on CVD with lipids
• Increases the risk for renal disease which in turn increases
the risk for CVD
Treatment of Hypertension
• Weight loss
– Demonstrated in observational & interventional
studies
– Decrease of 8/7 to16/9 mmHg for children with
3.9kg weight loss vs 10% weight loss
respectively
• Exercise
– May have additive effect
– Decrease of 10mm Hg with regular exercise
• Medication
Obesity & Dyslipidemia
Increased Risk of Abnormal Lipid
Levels in Overweight vs. Normal
Weight Teens
12
Increased Risk
10
8
TC>200
TG>130
LDL>130
HDL<35
6
4
2
0
7 to 8
9 to 10
11 to 12
Age (years)
13 to 14
15 to 17
Atherosclerosis & Dyslipidemia
• Evidence from adult studies
• Evidence in Children & Adolescents
– PDAY
– In vivo studies
• decreased compliance of arteries
• increased IMT in adolescents with dyslipidemia
Treatment of Dyslipidemia
• Weight loss
• Exercise
• Nutrition
–
–
–
–
Saturated fat <10% of calories
Total fat < 20-30% of calories
< 300mg cholesterol/day
Increase fiber intake
• Medication
Obesity & Inflammatory
Factors
Prevalence of Elevated CRP
(>0.22mg/dL) by BMI centile
Elevated CRP (%)
25
20
15
Boys
Girls
10
5
0
<25%
25-50%
50-75%
BMI centiles
75-85%
>85%
Level of TNF-alpha (ng/mL)
TNF-alpha Levels in Obese &
Non-obese Adolescents
20
18.15
15
10
5.88
5
0
Obese
Non-Obese
Moon et al. NASO, Oct. 2003
Homocysteine & other CVD
Risk Factors in Youth
• Homocysteine
–
–
–
–
An independent risk factor for CVD
> 10-12 umol/L increases CVD risk 2-4 fold
Not increased with obesity
Treatment: Folate 0.4 mg/day; B12 400-1000
ug/day; Vit. B6 400 mg/day
• Tobacco exposure: 1st & 2nd Hand
Preventing Cardiovascular
Disease
• Regular exercise (4-5 times/week)
–
–
–
–
Decreases weight gain
Increases HDL
Decreases blood pressure
Decreases inflammatory factors
• Healthy eating patterns
– Minimize saturated fat
• Cigarette Smoking Prevention
Adolescent Obesity
and its Effects into Adulthood
Obesity and CVD Risk
• In Nurses’ Health Study, 14-year CHD risk increased about 3.5-fold
for BMI >29 vs. <21, weight gain of >20 kg associated with 2.5-fold
increased risk.
• NHANES I follow-up showed a 1.5-fold greater risk of CVD in those
women with a BMI >29 vs. <21.
• A waist circumference of >35 inches in women, and >40 inches in men
is also associated with greater CHD risk.
Weight Related Risks for CHD and
Stroke
Obesity and Hypertension
• For every 1 kg/m2 increase in BMI, increased risk of hypertension
in Nurses’ Health Study was 12%
• Those with a BMI >31 RR=6.3 for developing HTN compared with
BMI <19.
• Study showed each 10 kg weight to be associated with an increase
of 3mmHg SBP and 2.2mHg DBP.
• Increased insulin levels may explain relation of obesity with HTN,
as compensatory increases in insulin are required to maintain
glucose homeostasis, and insulin may elevate BP by affecting renal
sodium retention, raising peripheral resistance.
Obesity and Diabetes
• Obesity worsens insulin sensitivity, eventually exhausting
pancreatic production of insulin, causing hyperglycemia and
diabetes.
Obesity and Diabetes
• In Pima Indians (approx 50% of adults diabetic), incidence
(per 1000 person-years) was 0.8 if BMI <20, but 72 if BMI
>40.
• In Nurses’ Health Study, BMI 23-23.9 showed a RR=3.6
for diabetes compared with BMI <22. Weight again was
very important, with weight again of 20-35kg associated
with an 11-fold greater risk of diabetes, >35kg 17-fold.
• In Health Professionals Study among men, BMI >35
associated with RR=42 for developing diabetes.
Obesity and Dyslipidemia
• Rates of cholesterol synthesis correlate with
excess body mass
• Data suggest a 10kg/m2 increment in BMI
is associated with a 3.2 mg/dl (women) to
10 mg/dl (men) lower HDL-C and about a
10 mg/dl greater LDL-C
Obesity and Dyslipidemia
• Obesity is associated with higher LDL-C and
triglycerides, and lower HDL-C.
Obesity and Dyslipidemia
• Weight loss reduces triglycerides, increases
HDL-C, and lowers LDL-C
Absolute Fat and Lean Changes per
Decade as a Function of Age in Men
Absolute Fat and Lean Changes per
Decade as a Function of Age in Women
Definitions
Body Mass Index (BMI) describes relative
weight for height: weight (kg)/height (m2)
• Overweight = 25–29.9 BMI
• Obesity = > 30 BMI
Age-Adjusted Standardized Prevalence of Overweight
(BMI 25–29.9) and Obesity (BMI >30)
24
.9
16
.3
16
.1
15
.1
12
.2
10
.4
20
11
.8
19
.9
24
.7
24
.3
23
.6
39
.4
39
.1
30
23
.6
Percent
40
37
.8
50
41
.1
NHES I NHANES I NHANES II NHANES III
10
0
Men
Women
BMI 25–29.9
CDC/NCHS, United States, 1960-94, ages 20-74
years
Men
BMI > 30
Women
NHANES III Age-Adjusted Prevalence of
Hypertension* According to BMI
BMI <25
BMI 25-26
BMI 27-29
BMI >30
50
38.4
Percent
40
32.2
30
20
22.5
25.2
18.2
21.9
24.0
16.5
10
0
Men
*Defined as mean systolic blood pressure 140 mm Hg, as mean diastolic
90 mm Hg, or currently taking antihypertensive medication .
Brown C et al. Body Mass Index and the prevalence of
Risk Factors for Cardiovascular Disease (in preparation).
Women
NHANES III Age-Adjusted Prevalence of
High Blood Cholesterol* According to BMI
BMI <25
BMI 25-26
BMI 27-29
BMI >30
50
Percent
40
27.9
30
20
14.7
17.5
20.4
28.2
20.2
15.7
10
0
Men
*Defined as > 240
mg/dL.
Brown C et al. Body Mass Index and the
Prevalence of Risk Factors for Cardiovascular
Disease (in preparation).
Women
24.7
NHANES III Age-Adjusted Prevalence of
Low HDL-Cholesterol* According to BMI
BMI <25 BMI 25-26 BMI 27-29 BMI >30
60
Percent
50
41.5
40
31.4
30
23.1
17.2
20
10
27.0
27.2
16.5
9.1
0
Men
*Defined as <35 mg/dL in men and <45 mg/dL in
women.
Brown C et al. Body Mass Index and the
Prevalence of Risk Factors for Cardiovascular
Disease (in preparation).
Women
Care of Overweight/Obese
Patients
Requires two steps:
•
Assessment
•
Management
Assessment of Overweight and
Obesity
• Body Mass Index
– Weight (kg)/height (m2)
– Weight (lb)/height (in2) x 703
– Table
• Waist Circumference
– High risk:
• Men >102 cm (40 in.)
• Women >88 cm (35 in.)
Classification of Overweight and Obesity by
BMI
Obesity Class
2
BMI kg/m
Underweight
<18.5
Normal
18.5–24.9
Overweight
25–29.9
Obesity
Extreme Obesity
I
30.0–34.9
II
35.0–39.9
III
40.0
Determine Absolute Risk Status
Evaluate:
• Disease conditions (e.g., CHD, type 2 diabetes, sleep apnea)
(+ = very high risk)
• Other obesity-associated diseases (e.g., gynecological
abnormalities, osteoarthritis)
• Cardiovascular risk factors: smoking, hypertension,
high LDL, low HDL, IGT, family hx (>3 = high risk)
• Other risk factors:
– Physical inactivity
– High serum triglycerides (>200 mg/dL)
Adolescent and Adult
Interventions
•
•
•
•
Decrease Television viewing
Decrease consumption of high fat foods
Increase fruit and vegetable intake
Increase moderate and vigorous physical activity
Weight Control and Risk Reduction
• Weight loss improves BP, dyslipidemia, and diabetes.
• Clinical trials show normotensive overweight persons on a hypocaloric diet
had a lowering of blood pressure and reduced incidence of hypertension.
DASH diet high in vegetables and fruits showed significant lowering of
SBP and DBP both in persons with and without HTN.
• Weight control also lessens hyperglycemia and has been shown to be
related to reduced diabetes-related mortality and improvements in glucose
and insulin levels.
• Among Indian coronary patients, those randomized to low saturated fat,
high fruit and vegetable diet plus weight-loss advice, compared to usual
care, showed a 50% reduction in cardiac events and 45% lower mortality in
those who lost more than 5kg.
Weight Control and Risk Reduction
• Meta-analysis of 70 randomized controlled trials shows
correlation between fall in LDL-C and amount of weight
loss (Dattilo et al., 1992)
• Combined programs of weight loss and exercise are
associated with greater increases in HDL-C and more
significant loss of weight and fat.
• Findings are less consistent in women, however, and often
LDL-C/HDL-C ratio worsens. While HDL-C is inversely
related to CHD risk in populations, low rates of CHD are
seen in populations with low-fat diets who have lower
levels of both LDL-C and HDL-C.
Fat vs. Caloric Restriction
• While fat from calories has been reduced from 40-42% to
34% over the past 30 years, recent data show we consume
more calories
• Message of caloric restriction needs to be coupled with
dietary fat reduction, with greater emphasis on fruit and
vegetable consumption
• Greater availability of low-fat and fat-free foods allows for
substitution away from traditional higher-fat alternatives.
Fat and calorie restriction needs to be individualized to
patient need and risk-factor profile.
Hypocaloric Diets
• Such diets allow for 1000-1200 kcal/day, with
very low-calorie diets providing only 400-500
kcal/day.
• Initial weight loss may be more rapid with the
very low-calorie diet, but amount of weight loss
over one year is similar with either plan and
adherence better with the moderate diet.
• Combination of low calorie diet plus exercise is
more successful than either strategy alone.
Health Benefits of Weight Loss
•
•
•
•
•
•
•
Decreased cardiovascular risk
Decreased glucose and insulin levels
Decreased blood pressure
Decreased LDL and triglycerides, increased
HDL
Decrease in severity of sleep apnea
Reduced symptoms of degenerative joint
disease
Improved gynecological conditions
1
Patient
Encounter
2
Treatment Algorithm
Hx of 25 BMI?
No
3
BMI
measured in
past
2 years?
Yes
4
BMI
6
• Measure weight,
height, and waist
circumference
• Calculate BMI
BMI 25 OR
waist circumference Yes
> 88 cm (F)
> 102 cm (M)
5
30 OR
7
Assess risk
factors
{[BMI 25 to 29.9
Yes
OR waist circumference
>88 cm (F) >102 cm (M)]
AND 2 risk
factors}
No
14
Hx BMI 25?
15
Clinician and patient
devise goals and
treatment strategy
for weight loss and
risk factor control
No
12
Yes
Does
patient want to
lose weight?
Yes
Yes
No
8
9
No
13
Brief reinforcement/ Advise to maintain
educate on weight weight/address
management
other risk factors
Examination
Treatment
Progress
being made/goal
achieved?
No
11
16
Periodic weight
check
:
10
Maintenance counseling:
Assess reasons for
failure to lose
Dietary therapy
weight
Behavior therapy
Physical activity
Treatment Algorithm
(Part 1 of 3)
1
Patient Encounter
2
Examination
Treatment
Hx of 25
BMI?
No
3
BMI
measured in
past
2 years?
Yes
4
• Measure
weight, height,
and waist
circumference
6
5
BMI 25 OR Yes
Assess risk
waist > 88 cm (F)
factors
> 102 cm (M)
• Calculate BMI
BMI
30 OR
{[BMI 25 to 29.9 Yes
OR waist >88 cm (F)
>102 cm (M)]
AND 2 risk
factors}
7
No
No
BMI
30 OR
7 {[BMI 25 to 29.9
OR waist >88 cm (F)
>102 cm (M)]
AND 2 risk
factors}
Examination
Treatment
No
Treatment Algorithm
(Part 2 of 3)
Yes
8
Devise goals and
treatment strategy for
weight loss and risk
factor control
No
12
Desire to
lose weight?
Yes
Yes
9
13
• Advise to maintain
weight
• Address other risk
factors
16
Periodic weight
check
Progress
made?
No
11
10
Maintenance
counseling
Assess reasons for
failure to lose weight
Treatment
5
BMI 25 OR
waist > 88 cm (F)
> 102 cm (M)
Algorithm
(Part 3 of 3)
Yes
Examination
Treatment
No
14
15
Yes
Hx BMI 25?
No
13
• Brief reinforcement
• Educate on weight
management
* This algorithm applies only to
the assessment for overweight and
obesity and subsequent decisions
based on that assessment. It does
not include any initial overall
assessment for cardiovascular risk
factors or diseases that are
indicated.
16
Periodic weight
check
• Advise to maintain
weight
• Address other risk
factors
Goals of Weight
Management/Treatment
• Prevent further weight gain
(minimum goal).
• Reduce body weight.
• Maintain a lower body weight
over long term.
Target Weight: Realistic Goals
• Substitute “healthier weight” for ideal or
•
landmark weight.
Accept slow, incremental progress to goal.
— Short-term goal: 5 to 10 percent loss,
1 to 2 lb per week.
— Interim goal: Maintenance.
— Long-term goal: Additional weight
loss,
if desired, and long-term weight
maintenance.
Weight Loss Goals
Goal: Decrease body weight by 10 percent from
baseline.
• If goal is achieved, further weight loss can be
attempted if indicated.
• Reasonable timeline: 6 months of therapy.
– Moderate caloric deficits
– Weight loss 1 to 2 lb/week
Weight Loss Goals
• Start weight maintenance efforts after
6 months.
– May need to be continued
indefinitely.
• If unable to lose weight, prevent
further weight gain.
Strategies for Weight Loss and
Maintenance
•
•
•
•
•
•
Dietary therapy
Physical activity
Behavior therapy
“Combined” therapy
Pharmacotherapy
Weight loss surgery
Weight Loss Therapy
Whenever possible, weight loss
therapy should employ the
combination of
• Low-calorie/low-fat diets
• Increased physical activity
• Behavior modification
Dietary Therapy (1 of 5)
Low-calorie diets (LCD) are recommended for
weight loss in overweight and obese persons.
Evidence Category A.
Reducing fat as part of an LCD is a practical
way to reduce calories. Evidence Category A.
Dietary Therapy (2 of 5)
Low-calorie diets can reduce total body
weight by an average of 8 percent and help
reduce abdominal fat content over a period of
6 months. Evidence Category A.
Dietary Therapy (3 of 5)
Although lower fat diets without targeted calorie
reduction help promote weight loss by producing
a reduced calorie intake, lower fat diets coupled
with total calorie reduction produce greater
weight loss than lower fat diets alone.
Evidence Category A.
Dietary Therapy (4 of 5)
Very low-calorie diets produce greater initial
weight loss than low-calorie diets. However,
long-term (>1 year) weight loss is not different
from an LCD. Evidence Category A.
Dietary Therapy (5 of 5)
Very Low-Calorie Diets (less than 800
kcal/day):
•
•
•
•
•
•
Rapid weight loss
Deficits are too great
Nutritional inadequacies
Greater weight regain
No change in behavior
Greater risk of gallstones
Low-Calorie Step I Diet
Nutrient
Recommended Intake
Calories
500 to 1,000 kcal/day reduction
Total Fat
30 percent or less of total calories
SFA
8 to 10 percent of total calories
MUFA
Up to 15 percent of total calories
PUFA
Up to 10 percent of total calories
Cholesterol
<300 mg/day
Low-Calorie Step I Diet (continued)
Nutrient
Recommended Intake
Protein
~ 15 percent of total calories
Carbohydrate
55 percent or more of total calories
Sodium Chloride
No more than 100 mmol/day (~ 2.4 g
of sodium or ~ 6 g of sodium
chloride)
Calcium
1,000 to 1,500 mg
Fiber
20 to 30 g
Percent of the Population by Race/Ethnicity
1990, 2000, 2025 and 2050
75.7
71.8
62.4
52.8
1990
2000
2025
2050
24.5
14.2
15.4
12.9
12.3
0.8
White, not
Hispanic
Africa n
American
0.9 1 1.1
3
6.6
4.1
8.7
Nativ e
Asian and
American,
Pacific
Eskimo,
Islander
Aleut
17.6
11.4
9
Hispanic
Origin (of
any ra ce)
Source: U.S. Bureau of the Census, decennial census and population projections
California’s Population by
Race and Ethnicity
• California leads the nation
in diversity.
• The state is challenged with
a substantial leadership
role in assuring a diverse
workforce and designing
and maintaining quality
care for all populations.
Source: Johnson, California’s Demographic Future, Public Policy Institute of California, 2003
Challenges for the Nation’s Workforce
• Insufficient numbers of staff;
• Unsatisfactory skill and proficiency levels;
• Inappropriate training to deal with a changed delivery
environment;
• Racial and ethnic diversity;
• Racial and ethnic disparities in access to and quality of
care.
Winds that are blowing...
• A national crisis is looming for health workforce but
it has as much to do with lack of innovation, as it
does with shortages of workers
Four Challenges
• Enhancing Public Participation in Clinical
Research
• Developing Information Systems
• An Adequately Trained Diverse Workforce
• Funding
New paradigms in clinical
research and research training
1.
What is the benefit of increasing representation of women and minorities
in the clinical research workforce?
2.
Will increased diversity improve translation
of the results of clinical research in minority communities?
3.
What are the needs of the private and public sector?
4.
Are the current approaches to training clinical investigators meeting the
needs of academia, industry, and public health?
Source: IOM: Opportunities to Address Clinical Research Workforce Diversity Needs for 2010 , 2006
New paradigms in clinical research
and research training
5.
Where is demand exceeding supply?
6.
What training programs and career tracks appear to foster
the development and retention of women and minorities in
the clinical research workforce?
7.
What research related to evaluation of existing training
efforts needs to be funded?
8.
What are the key outcome measures?
Source: IOM: Opportunities to Address Clinical Research Workforce Diversity Needs for 2010 , 2006
QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture.