Policy Procedure Manual
advertisement
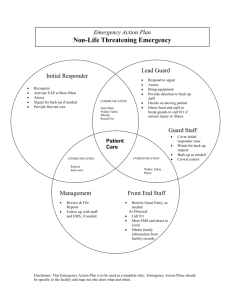
d/b/a SOS Technologies, Inc. A WBE-Certified Company TRAUMA-READY™ SELF-ASSISTMENT FOR CORPORATIONS. Approximately 150 million Americans go to work every day where they spend more than half of their waking hours. Yet, few companies are prepared to deal with sudden cardiac arrest (SCA). Every minute without CPR and defibrillation decreases the chance of survival by 7% -10% PER MINUTE! OSHA now recommends automated external defibrillators in the workplace. Employees should have the proper equipment, know how to use it, and know how to respond to an emergency including getting advanced medical help. We hope this complimentary assessment helps make your Hospitality area a safe environment. LifeSafe Services does offer an on-site analysis of your facility if desired. Call for details Safety Equipment Policy & Placement Guidelines This self-survey is broken into 6 parts. A. Equipping for a Trauma-Emergency. B. Placing equipment effectively. C. Policies and Maintenance. D. Emergency Response. E. Transfer of Care. F. Post-Event Procedures. A. Equipping for a Trauma-Emergency: OSHA’s Best Practices guidebooks states that first aid supplies “must be adequate, should reflect the kinds of injuries that occur, and must be stored in an area where they are readily available for emergency access. An automated external defibrillator (AED) should be considered when selecting first-aid supplies and equipment.” LifeSafe suggests the following, with portability being a key point for the Hospitality Industries: Personal Protection Equipment. AED (automated external defibrillator) Emergency Oxygen. First Aid Supplies. o Absorbent compress dressings (5 x 9 inches) o Adhesive bandages (assorted sizes) o Adhesive cloth tape (10 yards x 1 inch) o Antibiotic ointment packets (approximately 1 gram) o Antiseptic wipe packets o Packets of aspirin (81 mg each) o Blanket (space blanket) o Breathing barrier (with one-way valve) o Instant cold compress o Pair of non latex gloves (size: large) o Hydrocortisone ointment packets (approximately 1 gram each) o Scissors o Roller bandage (3 inches wide) o Roller bandage (4 inches wide) o Sterile gauze pads (3 x 3 inches) o Sterile gauze pads (4 x 4 inches) o Oral thermometer (non-mercury/non-glass) o Triangular bandages o Tweezers o First aid instruction booklet Clean-up Supplies. Blood borne Pathogens Kit. B. Placing Equipment Effectively. Based on the American Heart Association Guidelines of 3-5 minutes from “Drop to Shock” Implement the following procedures for best placement. Budgetary restraints often do not allow for the perfect environment, using the steps below should help evaluate the best locations to have a proactive emergency preparedness plan. Use a written floor plan, and mark the most critical areas for AED, O2 and safety supplies. This overview of the concept should help you to answer the following questions. Critical areas: Simple Rules: Calculations: Place responder equipment: In areas where the largest number of people are present, lobbies, large meeting rooms, cafeterias, etc. Medical equipment needs to be highly visible and accessible. Using the 3 to 4 minutes goal of the American Heart Association do one of the following. Near people with a history of heart disease. Areas that are difficult for EMS to reach. IE: Floors that must be reached by elevators, confined spaces, possibly restrooms. Hazardous areas such as high electric voltage or machine maintenance shops. Large geographical areas should have portable equipment. Near expected responders such as security guards, rangers, lifeguards, CPR /FA responders. Equipment must be easily accessible during all hours. Balance the best practice with financial responsibility. If you must walk to the equipment and then return to the victim with it: Use a stopwatch and walk for 1½ minutes. If you will radio for the equipment, a 3-minute direct walk if efficient. OR The average person walks 300 feet per minute; measure out 450 feet from each first aid station location. If they radio for help, measure out 900 feet. Questionnaire How will an employee get help for a victim? Cell Phone, landline, run to find an employee? If landline, do they first need to get an outside line? If cell phone, after calling 911 who do they call? Are there 2 way radios? How long will EMS take to arrive? Who will meet the EMS team? Where should the EMS team be met? How will the EMS team get to remote locations? Who should be contacted after an emergency? What is the furthest distance on the property? How long will it take to reach a victim in different areas? Is an elevator required? Is the stairwell accessible? Are there areas where people are isolated? Is the emergency equipment portable? Is it centrally located? Who has access to the AEDs? Who can use the AED’s? Are the AED’s allowed to be used off property, for example is your business by a road, are there other businesses in the building? Where is the highest concentration of People? Is there a responder kit located there? What equipment is in the kit? If not how far is the closest location in minutes? Is there heavy equipment used? Is there a responder kit located there? If yes, what equipment is in the kit? If not, how far is the closest responder kit in minutes? Are there meeting rooms? Is there a lobby? Is there a cafeteria? Is there a responder kit located there? If yes, what equipment is in the kit? If not, how far is the closest responder kit in minutes? Who is trained to use the AED? CPR? FA? When do the certifications expire? Are there any people with known heart disease? If so we are they located? Is there equipment near them? C. Policies and Maintenance. Does your state require medical direction? If yes, who provides your medical direction? Written emergency policies and procedures should be reviewed and practiced regularly. Facility staff members should be well-trained in AED use. Maintenance and record keeping need to be maintained. Facilities should coordinate their AED program with local EMS. Emergency drills should be practiced. AED programs must comply with local or regional regulations and legislation. D. Emergency Response. Detail the following questions: 1. What are the possible ways 911 will be called? Cell phone, radio, landline? 2. Is there an access number for landlines? 3. How will the Trauma-Response equipment be activated? 4. How will the First Aid Team be activated? 5. Who will bring the equipment? 6. Where is the equipment located? 7. Who will meet the EMS Team? 8. Where will the EMS Team be met? 9. How will the EMS Team get to a remote location? E. Transfer of Care: Transfer of Care: Once EMS arrives transfer care to the EMS entity. Give the EMS agency a complete oral report of the event and any significant findings. If requested by EMS, assist in patient care. Complete the Early Defibrillation Incident Report. The Early Defibrillation Incident Report is a part of the patient care record and is confidential to both the patient and the facility. This report is not to be copied or altered once it is completed. Discussion of all aspects of the event is to be limited. F. Post-Event procedure: Who should be contacted? Who is a back-up contact? Contact LifeSafe Services, 888-767-0050 to perform data collection and inspection from the AED; this must be completed before returning the units to service. Loaner equipment available at no charge if necessary. Once the data is downloaded, it can be transferred via file format or printed in a hard copy format. Clean the area in accordance with OSHA guidelines. Conduct a debriefing to evaluate the responder’s actions and procedures. There may be a potential need for emotional support of the responders involved. Perhaps informally with the team or with the assistance of professional counselors. Evaluate all aspects of the emergency response plan, both the positives and negatives.