Glycogen Metabolism Storage and Mobilization of Glucose
advertisement

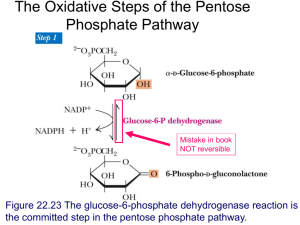
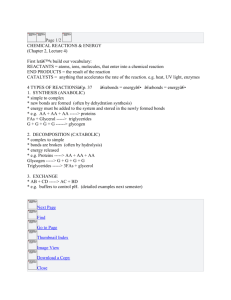
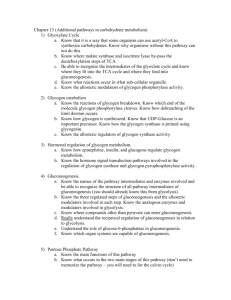
Glycogen Metabolism Storage and Mobilization of Glucose NUTR 543 – Advanced Nutritional Biochemistry David L. Gee, PhD Professor of Food Science and Nutrition Department of Health, Human Performance, and Nutrition Central Washington University Glycogen Functions Liver – Buffer for regulating blood glucose levels Muscle – Store of glucose as a fuel for exercise • high intensity exercise dependent on anaerobic glycolysis Glycogen Synthesis Figure 12-2 Regulation of Glycogen Synthase Figure 12-4 Active/Inactive Forms – Active • dephosphorylated – Inactive • phosphorylated Regulation of Glycogen Synthase Fasting Figure 12-4 Glucagon or epinephrine – G-protein linked receptors – increased [cAMP] Regulation of Glycogen Synthase Fasting Figure 12-4 cAMP activates Protein Kinase A Protein kinase A phosphorylates and inactivates glycogen synthase Little glycogen synthesis during fasting Regulation of Glycogen Synthase Feeding Figure 12-4 Insulin – Reduces [cAMP] • Stimulates phosphodiesterase – Induces and activates protein phosphatase-1 • Activates GS Feeding results in glycogen synthesis Glycogen Degradation Glycogen Phosphorylase – Hydrolyzes glucose units from glycogen – Produces glucose-1-P Removal of branch points – Debranching enzyme complex • Glucan transferase • Alpha-1,6-glucosidase Regulation of Glycogen Phosphorylase Fasting Figure 12-7 Glucagon or epinephrine – Increase [cAMP] – Activates Protein Kinase A – Phosphorylates and activates glycogen phosphorylase Fasting results in increased glycogenolysis Regulation of Glycogen Phosphorylase Feeding Figure 12-7 Insulin – Reduces [cAMP] – Induces and activates Protein Phosphatase-1 – Inactivates Glycogen Phosphorylase Feeding results in decreased glycogenolysis Allosteric Regulation of Glycogen Phosphorylase Table 12-1 Regulation of Glycogen Degradation during Exercise Figure 12-8 Coordinated Regulation of Glycogen Metabolism (Table 12-2) Application: Pharmacological Agents for Diabetics Insulin – Mandatory for Type 1 diabetics – Used in Type 2 diabetics as oral medications become less effective Oral medications – Mechanisms • • • • Increase insulin production Improve insulin receptor sensitivity Inhibit gluconeogenesis Inhibit carbohydrate absorption Sulfonylureas First widely used diabetic drug Stimulates endogenous release of insulin from pancreas – Direct action on ATP-K channel protein on beta-cells Short and longer acting forms – Glipizide (Glucotrol), glyburide (Diabeta), tolazamide (Tolinase) Side Effects – Hypoglycemia – Weight gain Meglitinides Like sulfonylureas, stimulate pancreatic secretion of insulin – Short-acting: taken with meals Replaglinide (Prandin) Side Effects – Hypoglycemia – Weight gain Biguanides Mechanism of action – Reduces gluconeogenesis (stimulates (?) Protein kinase A) – Decrease absorption of dietary CHO – Increase insulin sensitivity Metformin (Glucophage) (most widely used anti-diabetic drug) Side effects (not hypoglycemia) – Lactic acidosis • Contraindicated in heart failure, liver and kidney disorders – Diarrhea Other facts – Only drug shown to reduced risk diabetes related heart disease – Derived from French lilac (known as useful for treating symptoms of diabetes) Thiazolidinediones (TZDs) Mechanism of action – Binds to nuclear receptors that increase transcription of certain genes • Decreased insulin resistance • Leptin levels decreased (increased appetite) Rosiglitazone (Avandia) Side effects: edema, risk of hepatitis, increased heart disease risk (5/07 – FDA safety alert) Incretin mimetic Incretins are GI hormones that increase insulin production Exenatide (39aa peptide from saliva of gila monster (lizard spit), synthesized) – 50% homology with Glugacon-Like Peptide (GLP), an incretin that stimulates insulin production and inhibits glucagon production – Self-regulating: active only when during hyperglycemia – Appetite suppresent effect: gradual weight loss Side effects: – may increase hypoglycemic risk with sulfonylureas – must be injected 2x per day