Cardiovascular System: The Blood
advertisement

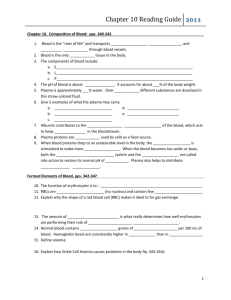
Cardiovascular System: The Blood Dr. Michael P. Gillespie Constituents Of Blood Blood is a connective tissue composed of a liquid matrix called plasma that dissolves and suspends various cells and fragments. Interstitial fluid is the fluid that bathes body cells. Functions of Blood Transportation – oxygen, carbon dioxide, nutrients, hormones, heat, & waste products. Regulation – maintains homeostasis (ph, heat, osmotic pressure). Protection – clotting, WBCs, & antibodies. Physical Characteristics Of Blood Blood is denser and more viscous than water. The temperature is 38 degrees C (100.4 degrees F). Slightly alkaline ph ranging from 7.35 to 7.45. 20% of the extracellular fluid (about 8% of total body mass). The blood volume is 5 to 6 liters (1.5 gal) in an average adult male and 4 to 5 liters (1.2 gal) in an average adult female. Withdrawing Blood Blood samples for laboratory testing are obtained in various ways. Venipuncture (the most common method). A finger or heel stick is utilized for children and people who must monitor their blood daily (I.E. Diabetics). An arterial stick is utilized when the level of O2 must be determined. Components Of Blood Whole blood has two components: Blood plasma, a watery liquid matrix that contains dissolved substances. Formed elements (cells and cell fragments). 45% formed elements and 55% plasma. Blood Plasma A straw-colored liquid which is about 91.5% water and 8.5% solutes. Plasma proteins – maintain osmotic pressure. Albumins, globulins, and fibrinogen (synthesized by hepatocytes). Gamma globulins (antibodies 0r immunoglobulins). Electrolytes, nutrients, regulatory substances (i.E. Enzymes and hormones), gases, & waste products (urea, uric acid, creatinine, ammonia, and bilirubin). Formed Elements RBCs. WBCs – perform many functions. Formed Elements Platelets – cell fragments. Formed Elements Hematocrit – the percentage of total blood occupied by RBCs. Males have a higher hematocrit than females because testosterone stimulates the production of erythropoeitin (EPO). Menstruation leads to lower values for females during their reproductive years. Anemia is a significant drop in the hematocrit. Polycythemia is an. Abnormally high percentage of RBCs. Causes of Polycythemia Abnormal increase in RBC production. Tissue hypoxia. Dehydration. Blood doping or use of Epoetin alfa (Procrit or Epogen) by athletes. This increases the work load of the heart. The increased #s of RBCs raise the viscosity of the blood, which increases the resistance to blood flow. This can cause high blood pressure and stroke. Formation of Blood Cells Hemopoiesis (hematopoiesis) – the process by which the formed elements of blood develop. Blood cells, macrophages, reticular cells, mast cells, and adipocytes arise from the red bone marrow. Pluripotent stem cells in the bone marrow reproduce themselves, proliferate and differentiate into mature blood cells. Two Types of Pluripotent Stem Cells Myeloid stem cells. Give rise to red blood cells, platelets, monocytes, neutrophils, eosinophils, and basophils. Lymphoid stem cells. Give rise to lymphocytes. Generations Of Cell Lines In The Development Of Blood Cells Pluripotent stem cells – mesenchymal cells which have the capacity to develop into many different types of cells. They can reproduce themselves. Progenitor cells – cannot reproduce themselves. Precursor cells (blasts) – they develop into the actual formed elements of the blood. Hormones That Regulate Blood Cell Development Hemopoietic growth factors – regulates differentiation and growth of progenitor cells. Erythropoietin (EPO) from the kidneys – increases the # of RBC precursors. Thrombopoietin (TPO) from the liver – stimulates the formation of platelets. Colony-stimulating factors (CSFs) or interleukins stimulate WBC formation. Medical Uses of Hemopoietic Growth Factors EPO is utilized in end stage kidney disease to increase RBC formation. CSFs are utilized to stimulate WBC formation in cancer patients undergoing chemotherapy. Thrombopoietin helps induce platelet formation in chemotherapy patients. Red Blood Cells Red blood cells (RBCs) or erythrocytes: Contain hemoglobin – oxygen-carrying protein which gives the cell its color. Approximately 5 million RBCs are present per microliter of blood. Approximately 2 million RBCs are created and destroyed per second. RBC Anatomy Biconcave discs with a diameter of 7-8 micrometers. The plasma membrane is flexible, which allows them to deform without rupturing as they squeeze through capillaries. RBCs lack a nucleus and other organelles. RBCs cannot reproduce or carry on extensive metabolic activities. RBC Physiology With no nucleus, RBCs have more space available for oxygen transport. RBCs lack mitochondria and generate ATP anaerobically; Consequently, they do not use up the oxygen they are transporting. RBC Physiology The biconcave disc has a greater surface area allowing greater diffusion of gas molecules. Hemoglobin binds to oxygen, carbon dioxide, and nitric oxide (NO). NO causes vasodilation which enhances oxygen delivery to cells. RBC Life Cycle Red blood cells live only about 120 days. Macrophages in the spleen and liver remove dead RBCs through phagocytosis. Hemoglobin is broken down into its globin and heme portions. Globin is broken down into amino acids, which are reused for proteins. Heme is converted into the yellow-orange pigment bilirubin. Reticulocyte Count The rate of eryhtropoiesis is measured by a reticulocyte count. Low “retic” count – could indicate a shortage of erythropoietin due to a nutritional deficiency or leukemia. High “retic” count – could indicate a good response to previous blood loss, iron therapy, or illegal use of Epoetin by an athlete. White Blood Cells White blood cells (WBCs) or leukocytes have a nucleus and do not contain hemoglobin. Classified as either granular or agranular. Types Of White Blood Cells Eosinophil Basophil Neutrophil Small lymphocyte Monocyte Numbers Of WBCs RBCs outnumber WBCs by about 700:1. There are approximately 5000 – 10,000 cells per microliter of blood. Leukocytosis – an increase in the number of WBCs due to stresses such as microbes, strenuous exercise, anesthesia, or surgery. Leukopenia – a decrease in the number of WBCs due to radiation, shock, or chemotherapy. Functions Of WBCs The WBCs combat pathogens by phagocytosis and other immune responses. WBCs leave the bloodstream by emigration. Functions Of WBCs Neutrophils and macrophages are active in phagocytosis. Phagocytes are attracted to inflamed tissues through a process called chemotaxis. Phagocytes release the enzyme lysozyme, which destroys certain bacteria. Functions Of WBCs Eosinophil – release histamines. Respond to allergic responses and parasitic infection. Basophil – liberate heparin, histamine, and serotonin. They intensify the inflammatory reaction and are involved in hypersensitivity (allergic) reactions. Functions Of WBCs Neutrophil – active in phagocytosis and ingest bacteria and dead matter. They respond to bacteria and fungi. Lymphocyte – “soldiers” of the immune system. Monocyte – turn into macrophages and clean up cellular debris after an infection. Differential WBC Count Utilized to detect infection, inflammation, poisoning, blood disorders, effects of chemotherapy, allergic reactions, and parasitic infections. Significance Of High & Low WBC Counts WBC Type High Count Low Count Neutrophils Bacterial infection, burns, stress, inflammation Viral infection, leukemia Radiation, drug toxicity, B12 deficiency, SLE Lymphocytes Prolonged illness, immunosuppress ion, cortisol tx. Significance Of High & Low WBC Counts Monocytes Eosinophils Basophils Viral or fungal infection, chronic diseases Allergic rx., parasites, autoimmune dis. Allergic rx., cancers, hypothyroidism Bone marrow suppression, cortisol tx. Drug toxicity, stress Pregnancy, ovulation, stress, hyperthyroidism Platelets The hormone thrombopoietin influences the production of platelets (thrombocytes). Platelets help stop blood loss by forming a platelet plug. Complete Blood Count (CBC) A test that screens for anemia and various infections. Counts of RBCs, WBCs, platelets, hematocrit, and a differential white blood cell count are included. Blood Clotting Serum is a straw colored liquid and the gel is called a clot. The process of gel formation is called clotting or coagulation. Clotting factors are involved in the coagulation cascade. Blood Clotting Normal clotting requires vitamin K, which is produced by bacteria in the intestines. Dissolution of a clot is called fibrinolysis. Anticoagulants (heparin & Warfaring a.K.A. Coumadin) are utilized for patients at risk of forming a blood clot. Intravascular Clotting Thrombosis – clotting in an unbroken blood vessel. Thrombus – the clot itself. Embolus – a blood clot, bubble of air, fat from broken bones, or a piece of debris transported by the bloodstream. Pulmonary embolism – when an embolus lodges in the lungs. ABO Blood Group Type A blood - RBCs display only antigen A. Type B blood – RBCs display only antigen B. Type AB blood – RBCs display both antigens A & B. Type O blood – RBCs display neither antigen A or B. ABO Blood Group The blood plasma contains isoantibodies or agglutinins that react with A or B antigens if mixed. You do not have the antibodies that react with the antigens of your own RBC type, but you most likely have the antibodies for antigens your own blood lacks. Rh Blood Group People with Rh antigens in their blood are Rh positive and people without the Rh antigen are Rh negative. Normally, plasma does not contain anti-Rh antibodies. Rh Blood Group If an Rh- person receives Rh+ blood transfusion, he or she will start to make antibodies that will remain in the blood. The next time he or she receives Rh+ blood, the antibodies will cause hemolysis of the donated blood. Hemolytic Disease Of The Newborn ABO Blood Group Interactions Characteristics A B AB O Antibody Anti-B in plasma Antigen on A RBCs Anti-A Neither Both B A&B Neither Donors B, O A, B, AB, O None O A, O Hemolysis B, AB A, AB A, B, AB