Blood Chapter 17
advertisement

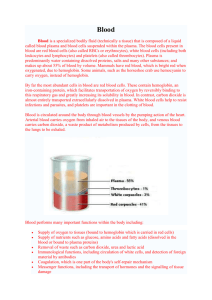
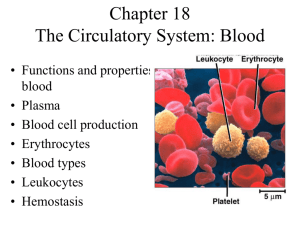
Blood Chapter 17 Composition of Blood • Body’s only fluid tissue • It is composed of liquid plasma (54%) and formed elements (Cells) (46%) • Erythrocytes, or red blood cells (RBCs)- 45% • Leukocytes, or white blood cells (WBCs) and Platelets (1%) Physical Characteristics and Volume • The pH of blood is 7.35–7.45 • Temperature is 38C, slightly higher than “normal” body temperature • 5–6 L for males, and 4–5 L for females Color depends on its oxygen content. – Bright red when oxygenated (e.g., arterial blood) – Dark red when deoxygenated (e.g., venous blood). Without O2 With O2 Functions of Blood • Distribution – Gases, nutrients, signaling molecules, wastes, heat • Regulation – Body fluid volume – Body fluid pH – Body T° – Electrolyte levels • Protection from pathogens and fluid loss Body Temperature Regulation Notice how the distribution of blood varies with temperature. Under warm conditions, blood is shunted to the surface so that heat can radiate away. Under cold conditions, blood (and thus heat) are conserved within the core of the body. Plasma • 55% of blood • Mostly water • Dissolved Solutes Contains: – Proteins – Electrolytes – Gases – Nutrients – Wastes – Signaling molecules – Buffers Some of the Plasma Proteins – Albumin • 60% of plasma proteins. • Produced by the liver. • Primary function is to maintain the osmotic pressure of the plasma. Also involved in transport of certain substances (steroids, bilirubin). – Globulins • Some globulins are produced in the liver and are transport proteins for lipids, metal ions, and fat-soluble vitamins. • Other globulins are produced by plasma cells (a type of leukocyte) during the immune response. These globulins are also known as antibodies. – Clotting proteins • Most produced in the liver. • Two important examples are prothrombin and fibrinogen. Erythrocytes (RBCs) • • • • • • • Small Biconcave disks Anucleate No organelles Stuffed with hemoglobin Transport O2 4-6 million per μL of blood Figure 16.3 Hemoglobin • Note the 4 heme groups associated with the 4 polypeptide chains of the hemoglobin protein. Each has an iron in its center. How many O2 molecules could a single hemoglobin carry? Hemopoiesis • Blood cell formation = hemopoiesis • All blood cell production occurs in the red bone marrow, which is found in the: – Axial skeleton – Pelvic and pectoral girdles – Proximal epiphyses of the humerus and femurs. • What must happen as a hemocytoblast differentiates into an RBC? • - What must be lost? • - What must be made? • - What must change? RBC Production RBC Lifespan Born in the red marrow Circulate for 120d Swallowed by a macrophage (usually in the spleen) Hemoglobin Heme Globin Iron Bilirubin Carried by albumin to the liver Carried by transferrin to the liver Secreted into the small intestine as part of bile Stored in the liver as hemosiderin or ferritin Converted to stercobilin and urobilin and excreted in feces Amino acids Back into the plasma for reuse/recycling Red Blood Cells An important measurement involving RBCs is the hematocrit. The hematocrit is the % of whole blood occupied by RBCs. It’s reflective of the body’s O2 carrying capacity. What’s the hematocrit in the sample below? Homeostatic Imbalance Genetic Thalassemias • Missing a globin chain • RBC fragile and ruputre easy Homeostatic Imbalance Sickle-cell anemia -Results from a defective gene coding for an abnormal hemoglobin called hemoglobin S (HbS) - HbS has a single amino acid substitution (287) - This defect causes RBCs to become sickle-shaped in low-oxygen situations Leukocytes (WBCs) • Only blood components that are complete cells: – 4000 – 11,000 WBC’s /mm3 – Make up 1% of the total blood volume – Can leave capillaries via diapedesis – Move through tissue spaces – Most are found in lymphatic organs and loose connective tissues. Neutrophils • Most numerous. 60% of circulating WBCs. • A.k.a. polymorphonuclear leukocytes b/c of their multilobed nucleus. • Function primarily in killing bacteria. • Contain pale, lilac colored granules Eosinophils • • • • 3% of circulating WBCs. Function primarily in killing parasitic worms. Also help reduce the severity of allergy attacks. Contain reddish/orangish granules Basophils • Least numerous. <1% of circulating WBCs. • Involved in inflammation. • Contain purplish granules that contain: – Histamine – a vasodilator – Heparin – an anticoagulant Lymphocytes • 25% of circulating WBCs. • No granules. Large purple nucleus dominates most of the cell. • 2 main types: – T lymphocytes • Control/coordinate immune response • Kill virus-infected and cancerous cells – B lymphocytes • Secrete antibodies (immunoglobulins) Monocytes • • • • 6% of circulating WBCs. No granules. Large pale cells w/ U or kidney-shaped nucleus. Travel in the blood. Become macrophages w/in the tissue spaces. In this picture, find: RBCs, 2 neutrophils, an eosinophil, a basophil, a monocyte, a lymphocyte, and a platelet. What can you find here? Homeostatic Imbalance Leukemias • Cancerous bone marrow cell that send immature white blood cells into blood stream • Immune response lessen Platelets • Cell fragments of megakaryocytes (giant cells created from mitosis w/o cytokinesis) • Contain chemicals vital to coagulation. • A.k.a. thrombocytes. Hemostasis • Designed for healing the vasculature and providing a framework for tissue repair Three phases 1. Vascular spasms – immediate vasoconstriction in response to injury 2. Platelet plug formation 3. Coagulation (blood clotting) Mosquito saliva contains an enzyme called apyrase. Which of the following is it most likely to do? a. b. c. d. Inhibit fibrinolysis Promote thrombin production Inhibit platelet aggregation Promote fibrin production • • • • Antiprostaglandin Aspirin Low dose helps reduce risk of heart attack Reduces platelet aggregation and plug formation Reduces risks to embolism Heart attack and stroke Blood Groups • Humans have 30 varieties of naturally occurring RBC antigens • The antigens of the ABO and Rh blood groups cause vigorous transfusion reactions with agglutination (cell clumping) and severe consequences when they are improperly transfused • RBC membranes have glycoprotein antigens on their external surface • These antigens are: – Unique to the individual – Recognized as foreign if transfused into another individual • Presence/absence of these antigens are used to classify blood groups AB0 blood grouping system = red blood cell • Blood group A – A antigens on the surface of their red blood cells and B antibodies in their blood plasma. • Blood group B – B antigens on the surface of their RBCs and A antibodies • Blood group AB – A and B antigens on the surface of their RBCs and no A or B antibodies at all • Blood group 0 (null) – No antigens on the surface of their RBCs but both A and B antibodies http://nobelprize.org/medicine/educational/landsteiner/readmore.html ABO Blood Groups Universal donor Universal receiver - Table 16.4 Blood Typing http://nobelprize.org/medicine/educational/landsteiner/readmore.html • When serum containing anti-A or anti-B antibodies is added to blood, agglutination (cell clumping) will occur between the antibody and the corresponding antigens • Positive reactions indicate agglutination (cell clumping) Blood typ e being tested RBC agglutinog ens AB B A O A and B B A none Serum Reaction Anti -A Anti -B + + – + + – – – Rh factor blood grouping system Rh+ • Have Rh factor on RBCs • Do not make Rh antibodies Rh• Do not have Rh factor on RBCs • Do not make Rh antibodies unless exposed to Rh factor!!! What will occur??? http://nobelprize.org/medicine/educational/landsteiner/readmore.html Women and Pregnacy • Rh- women with Rh+ babies • Pregnancy okay, but mother builds Rh antibodies • If next pregnancy is Rh+ again mothers antibodies will kill fetus RBCs • RhoGAM blocks the Rh+ affect and does not allow mother to make antibodies