CLINICAL CHEMISTRY CHAPTER 14
advertisement

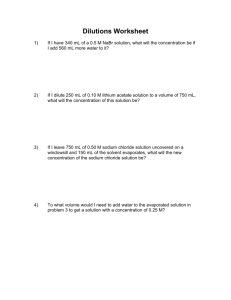
CLINICAL CHEMISTRY ELECTROLYTES 1 Introduction – This chapter is largely about the water and electrolytes ( salts )in your plasma and how the body manages to keep you from drying up and blowing away even if you are in the hot Texas sun and without liquid drink. 2 Chapter KEY TERMS • • • • • • • • • • • • • Anion Anion Gap Cation Active transport Diffusion Electrolyte Osmolality Osmolality Polydipsia Tetany ADH Hypothalamus Gland Renin - Angiotensin Aldosterone System • • • • • Hyper / Hypo … natremia , kalemia, calcemia Parathyroid Hormone ( PTH ) Acidosis / Alkalosis Calcitonin Ion Selective Electrode • • • • • • • Na = Sodium K = Potassium Cl = Chloride CO2 = Carbon Dioxide Ca = Calcium Mg = Magnesium PO4 = Phosphate 3 General Objectives • Define the key terms • Discuss the factors that regulate each of the electrolytes • Discuss the physiological functions and clinical significance of each of the electrolytes • Discuss ISE and Osmometers 4 Electrolytes • Electrolytes – Substances whose molecules dissociate into ions when they are placed in water. – CATIONS (+) ANIONS (-) • Medically significant / routinely ordered electrolytes include: – sodium (Na) – potassium (K) – chloride (Cl) – and CO2 (in its ion form = HCO3- ) 5 Electrolyte Functions • • • • • • • • Volume and osmotic regulation Myocardial rhythm and contractility Cofactors in enzyme activation Regulation of ATPase ion pumps Acid-base balance Blood coagulation Neuromuscular excitability Production of ATP from glucose 6 Electrolytes • General dietary requirements – Most need to be consumed only in small amounts as utilized – Excessive intake leads to increased excretion via kidneys – Excessive loss may result in need for corrective therapy • loss due to vomiting / diarrhea; therapy required - IV replacement, Pedilyte, etc. 7 Electrolytes • Water (the diluent for all electrolytes) constitutes 4070% of total body and is distributed: – Intracellular – inside cells • 2/3 of body water (ICW) – Extracellular – outside cells • 1/3 of body water – Intravascular – plasma 93% water » Intrastitial -surrounds the cells in tissue (ISF) 8 Electrolytes 9 Electrolytes • Ions exist in all of these fluids, but the concentration varies depending on individual ion and compartment • The body uses active and passive transport principles to keep water and ion concentration in place 10 Electrolytes • Sodium has a pulling effect on water – Na affects extracellular fluids (plasma & interstitial) equally. – However, because there is considerably more Na outside cells than inside, the water is pulled out of cells into the extracellular fluid. – Na determines osmotic pressure of extracellular fluid. 11 Electrolytes • Proteins (especially albumin) inside the capillaries strongly pulls/keeps water inside the vascular system – Albumin provides oncotic pressure. – By keeping Na & albumin in their place, the body is able to regulate its hydration. • When there is a disturbance in osmolality, – the body responds by regulating water intake, – not by changing electrolyte balance 12 Electrolytes • Laboratory assessment of body hydration is often by determination of osmolality and specific gravity of urine 13 Electrolytes Osmolality • Physical property of a solution based on solute concentration – Water concentration is regulated by thirst and urine output – Thirst and urine production are regulated by plasma osmolality 14 Electrolytes Osmolality • osmolality stimulates two responses that regulate water – Hypothalamus stimulates the sensation of thirst – Posterior pituitary secrets ADH • ( ADH increases H2O re-absorption by renal collection ducts ) • In both cases, plasma water increases 15 Electrolytes • Osmolality – concentration of solute / kg – reported as mOsm / kg • another term: – Osmolarity - mOsm / L - not often used 16 Electrolytes • Determination – 2 methods or principles to determine osmolality • Freezing point depression – (the preferred method) • Vapor pressure depression – Also called ‘dewpoint’ 17 Specimen Collection • Serum • Urine • Plasma not recommended due to osmotically active substances that can be introduced into sample • Samples should be free of particulate matter..no turbid samples, must centrifuge 18 Electrolytes • Calculated osmolality – uses glucose, BUN, & Na values – (Plasma Sodium accounts for 90 % of plasma osmolality) • Formula: – 1.86 (Na) + glucose∕18 + BUN∕2.8 = calculated osmolality • Osmolal gap = difference between calculated and determined osmolatity – Should be less than 10-15 units difference • (measured – calculated = 10 to 15) 19 Electrolytes • Increase in the difference between measured and calculated – would indicate presence of osmo active substances such as possibly alcohol - ethanol, methanol, or ethylene glycol or other substance. • Osmolality are concerns for – Infants – Unconscious patients – Elderly 20 Electrolytes • Decreased osmolality – Diabetes insipidus • ADH deficiency • Because they have little / no water reabsorption, produce 10 – 20 liters of urine per day 21 Electrolytes • Osmolality normal values – – – – Serum – 275-295 mOsm/Kgm 24 hour urine – 300-900 mOsm/Kgm urine/serum ratio – 1.0-3.0 Osmolal gap < 10-15 mOsm (depending on author) 22 Electrolytes • Classifications of ions - by their charge – Cations – have a positive charge - in an electrical field, (move toward the cathode) • Na+ = most abundant extracellular cation • K+ = most abundant intracellular cation 23 Electrolytes – Anions – have a negative charge - move toward the anode • Cl– (1st) most abundant extracellular anion • HCO–3 – (bicarbonate) second most abundant extracellular anion 24 Electrolytes • Phosphate is sometimes discussed as an electrolyte, sometimes as a mineral. – HPO-24 / H2PO-4 – when body pH is normal, HPO-24 is the usual form (@ 80 % of time) 25 Electrolyte Summary • cations (+) • • • • • Na 142 K 5 Ca 5 Mg 2 154 mEq/L • anions (-) • • • • • • Cl 105 HCO324 HPO4-2 2 SO4-2 1 organic acids 6 proteins 16 » 154 mEq/L 26 Routinely measured electrolytes • Sodium – – the major cation of extracellular fluid outside cells – Most abundant (90 %) extracellular cation – Functions - recall influence on regulation of body water • Osmotic activity - sodium determines osmotic activity (Main contributor to plasma osmolality) • Neuromuscular excitability - extremes in concentration can result in neuromuscular symptoms 27 Routinely measured electrolytes • Diet - sodium is easily absorbed • Na-K ATP-ase Pump – pumps Na out and K into cells • Without this active transport pump, the cells would fill with Na and subsequent osmotic pressure would rupture the cells 28 Regulation of Sodium • Concentration depends on: – intake of water in response to thirst – excretion of water due to blood volume or osmolality changes • Renal regulation of sodium – Kidneys can conserve or excrete Na+ depending on ECF and blood volume • by aldosterone • and the renin-angiotensin system – this system will stimulate the adrenal cortex to secrete aldosterone. 29 Sodium (Na) • Aldosterone – From the (adrenal cortex) – Functions • promote excretion of K • in exchange for reabsorption of Na 30 Sodium (Na) • Sodium normal values – Serum – 135-148 mEq/L – Urine (24 hour collection) – 40-220 mEq/L 31 Sodium (Na) • Urine testing & calculation: – 1st. Because levels are often increased, a dilution of the urine specimen is usually required. – Then the result from the instrument (mEq/L or mmol/L) X # L in 24 hr. 32 Clinical Features: Sodium • Hyponatremia: < 135 mmol/L – Increased Na+ loss • Aldosterone deficiency – Addison’s disease (hypo-adrenalism, result in ➷ aldosterone) • Diabetes mellitus – In acidosis of diabetes, Na is excreted with ketones • Potassium depletion – K normally excreted , if none, then Na • Loss of gastric contents 33 Hyponatremia • Increased water retention – Dilution of serum/plasma Na+ – excretion of > 20 mmol /mEq urine sodium) • Renal failure • Nephrotic syndrome • Water imbalance – Excess water intake – Chronic condition 34 Hypernatremia • Excess water loss resulting in dehydration (relative increase) – Sweating – Diarrhea – Burns – Dehydration from inadequate water intake, including thirst mechanism problems – Diabetes insipidus • (ADH deficiency … H2O loss ) 35 Hypernatremia • Excessive IV therapy • comatose diabetics following treatment with insulin. Some Na in the cells is kicked out as it is replaced with potassium. – Cushing's syndrome - opposite of Addison’s 36 Specimen Collection: Sodium (Na) • serum (sl hemolysis is OK, but not gross) • • • • heparinized plasma timed urine sweat GI fluids • liquid feces (would be only time of excessive loss) 37 Sodium (Na) Note: • Increased lipids or proteins may cause false decrease in results. artifactual/pseudo-hyponatremia 38 Sodium (Na) • Sodium determination – Ion-selective (specific) electrode • Membrane composition = lithium aluminum silicate glass • Semi-permeable membrane allows sodium ions to cross 300X faster than potassium and is insensitive to hydrogen ions. • direct measurement – where specimen is not diluted – gives the truest results – systems that dilute the sample give lower results (called dilutional effect) 39 Sodium (Na) – Flame emission spectrophotometry (flame photometer) • Na emits λ 589 nm (yellow) • Use internal standard of lithium or cesium • Possible for a dilutional error to occur in some flame photometer systems, but literature does not dwell on it. 40 Routinely measured electrolytes • Potassium (K) – the major cation of intracellular fluid • Only 2 % of potassium is in the plasma • Potassium concentration inside cells is 20 X greater than it is outside. • This is maintained by the Na pump, (exchanges 3 Na for 1 K) INSIDE 20 OUTSIDE 1 41 Potassium (K) • Function – critically important to the functions of neuromuscular cells – Critical for the control of heart muscle contraction! • ↑ potassium promotes muscular excitability • ↓ potassium decreases excitability (paralysis and arrhythmias) 42 Potassium (K) • Regulation – Diet • easily consumed (bananas etc.) – Kidneys • Kidneys - responsible for regulation. Potassium is readily excreted, but gets reabsorbed in the proximal tubule - under the control of ALDOSTERONE 43 Potassium (K) • Potassium normal values – Serum (adults) – 3.5 - 5.3 mEq/L – Newborns slightly higher – 3.7 - 5.9 mEq/L – Urine (24 hour collection) – 25 - 125 mEq/L 44 Hypokalemia • Decrease in K concentration • Effects • neuromuscular weakness & cardiac arrhythmia 45 Causes of hypokalemia – Excessive fluid loss ( diarrhea, vomiting, diuretics ) – ↑ Aldosterone promote Na reabsorption … K is excreted in its place (Cushing’s syndrome = hyper aldosterone) – Insulin IVs promote rapid cellular potassium uptake 46 Causes of hypokalemia • Increased plasma pH ( decreased Hydrogen ion ) RBC H+ K+ K+ moves into RBCs to preserve electrical balance, causing plasma potassium to decrease. ( Sodium also shows a slight decrease ) 47 Hyperkalemia • Increased K concentration • Causes – IV’S or other increased intake – Renal disease – impaired excretion – Acidosis (Diabetes mellitus ) • H+ competes with K+ to get into cells & to be excreted by kidneys • Decreased insulin promotes cellular K loss • Hyperosomolar plasma (from ↑ glucose) pulls H2O and potassium into the plasma 48 Hyperkalemia • Causes – Tissue breakdown ( RBC hemolysis ) – Addison’s - hypo- adrenal; hypoaldosterone 49 Specimen Collection:Potassium • Non-hemolyzed serum • heparinized plasma • 24 hr urine. 50 Potassium (K) • Determination – Ion-selective electrode (valinomycin membrane) • insensitive to H+, & prefers K+ 1000 X over Na+ – Flame photometry • - K λ 766 nm 51 Chloride ( Cl - ) • Chloride - the major anion of extracellular fluid – Chloride moves passively with Na+ or against HCO3- to maintain neutral electrical charge – Chloride usually follows Na (if one is abnormal, so is the other) – Function - not completely known • body hydration • osmotic pressure • electrical neutrality & other functions 52 Chloride ( Cl - ) • Regulation via diet and kidneys – In the kidney, Cl is reabsorbed in the renal proximal tubules, along with sodium. – Deficiencies of either one limits the reabsorption of the other. 53 Chloride ( Cl - ) • Normal values – Serum – 100 -110 mEq/L – 24 hour urine – 110-250 mEq/L • varies with intake – CSF – 120-132 mEq/L 54 Hypochloremia • Decreased serum Cl – loss of gastric HCl – salt loosing renal diseases – metabolic alkalosis; – increased HCO3- & decreased Cl- 55 Hyperchloremia • Increased serum Cl – dehydration (relative increase) – excessive intake (IV) – congestive heart failure – renal tubular disease – metabolic acidosis – decreased HCO3- & increased Cl- 56 Specimen Collection: Chloride • • • • Serum heparinized plasma 24 hr urine sweat 57 Chloride ( Cl - ) • Determination – Amperometric/Coulometric titration – involves titration with silver ions. 58 Chloride ( Cl - ) • Mercurimetric titration of Schales and Schales – Precipitate protein out - 1 st step – Titrate using solution of mercury • Hg +2 + 2 Cl- = HgCl2 – When all chloride is removed, next drop of mercury will complex with diphenylcarbazone indicator to produce violet color = endpoint • a calculation required to determine amt of Cl present by the amt of Hg used 59 Chloride ( Cl - ) • Colorimetric – Procedure suitable for automation – Chloride complexes with mercuric thiocyanate – forms a reddish color proportional to amt of Cl in the specimen. 60 Chloride ( Cl - ) • Sweat chloride – – Remember, need fresh sweat to accurately measure true Cl concentration. – Testing purpose - to ID cystic fibrosis patients by the increased salt concentration in their sweat. • Pilocarpine iontophoresis – Pilocarpine = the chemical used to stimulate the sweat production – Iontophoresis = mild electrical current that simulates sweat production 61 Chloride ( Cl - ) • CSF chloride – NV = 120 - 132 mEq/L (higher than serum) – Often CSF Cl is decreased when CSF protein is increased, as often occurs in bacterial meningitis. 62 bicarbonate ion (HCO3- ) • Carbon dioxide/bicarbonate – – * the major anion of intracellular fluid – 2nd most important anion (2nd to Cl) • Note: most abundant intra-cellular anion • 2nd most abundant extra-cellular anion 63 bicarbonate ion (HCO3- ) • Total plasma CO2 = HCO3- + H2CO3- + CO2 – HCO3- (carbonate ion) accounts for 90% of total plasma CO2 – H2CO3- carbonic acid (bicarbonate) 64 bicarbonate ion (HCO3- ) • Regulation: – Bicarbonate is regulated by secretion / reabsorption of the renal tubules – Acidosis : ↓ renal excretion – Alkalosis : ↑ renal excretion 65 bicarbonate ion (HCO3- ) • Kidney regulation requires the enzyme carbonic anhydrase - which is present in renal tubular cells & RBCs carbonic anhydrase carbonic anhydrase Reaction: CO2 + H2O ⇋ H2CO3 → H+ + HCO–3 66 bicarbonate ion (HCO3- ) CO2 Transport forms – 8% dissolved in plasma • dissolved CO2 – 27% carbamino compounds • C02 bound to hemoglobin – 65% bicarbonate ion • HCO3- - carbonate ion 67 bicarbonate ion (HCO3- ) • Normal values – Total Carbon dioxide (venous) – @ 2230 mmol/L • includes bicarb, dissolved & undissociated H2CO3 - carbonic acid (bicarbonate) – Bicarbonate ion (HCO3–) – 22-26 mEq/L 68 bicarbonate ion (HCO3- ) • Function – – CO2 is a waste product – continuously produced as a result of cell metabolism, – the ability of the bicarbonate ion to accept a hydrogen ion makes it an efficient and effective means of buffering body pH – dominant buffering system of plasma – makes up @ 95% of the buffering capacity of plasma 69 bicarbonate ion (HCO3- ) • Significance – The bicarbonate ion (HCO–3) is the body's major base substance – Determining its concentration provides information concerning metabolic acid/base 70 bicarbonate ion (HCO3- ) • CO2 /bicarb Determination – Specimen can be heparinized plasma, arterial whole blood or fresh serum. Anaerobic collection preferred. • methods • • • • Ion selective electrodes Colorimetric Calculated from pH and PCO2 values Measurement of liberated gas 71 Electrolyte balance • Anion gap – an estimate of the unmeasured anion concentrations such as sulfate, phosphate, and various organic acids. 72 Electrolyte balance • Calculations – 1. Na - (Cl + CO2 or HCO3-) = – NV 8-12 mEq/L – Or – 2. (Na + K) - (Cl + CO2 or HCO3-) NV 7-14 mEq/L • which one to use may depend on whether K value is available. Some authors feel that K value is so small and usually varies little, that it is not worth including into the formula. 73 Electrolyte balance • Causes in normal patients – what causes the anion gap? – 2/3 plasma proteins & 1/3 phosphate& sulfate ions, along with organic acids • Increased AG – – uncontrolled diabetes (due to lactic & keto acids) – severe renal disorders • Decreased AG – a decrease AG is rare, more often it occurs when one test/instrument error 74 Normal Ranges SODIUM POTASSIUM CHLORIDE CO2 135 – 145 3.5 – 5.0 100 – 110 20 – 30 ANION GAP 10 - 20 PLASMA OSMOALITY CALCIUM IONIZED Ca MAGNESIUM PHOSPHATE LACTATE mEq/L mEq/L mEq/L mEq/L meq / L 275 - 295 8.5 – 10.0 4.5 – 5.5 1.2 – 2.1 2.5 – 4.5 0.5 – 17.0 mOsmol / kg mg/dL mg/dL mEq/L mg/dL mgl/dl 75 ELECTROYTE TOP 10 • Osmolality is detected by the Hypothalamus Gland Thirst sensation and secretion of ADH by Posterior Pituitary Gland. ADH increases renal reabsorption of water • Blood Volume stimulates Renin - Angiotensin - Aldosterone system. Aldosterone secretion by the Adrenal Cortex stimulates increased renal absorption of sodium • Sodium is the main extracellular cation and contributor to plasma osmolality Potassium is the main intracellular cation Plasma “CO2” = Dissolved CO2 + H2 CO3 + HCO3Chloride is usually a passive follower of Sodium to maintain electrical charge Sodium and Potassium usually move opposite each other • • • • • Parathyroid Hormone ( PTH ) secretion increases plasma calcium , increases plasma magnesium and decreases phosphate • Acidosis is associated with Potassium ( Alkalosis with Potassium ) 76 Electrolyte Links http://www.nlm.nih.gov/medlineplus/ency/article/002350.htm http://www.thirdage.com/health/adam/ency/article/002350.htm 77