Febrile Neutropenia...Where Do We Stand
advertisement

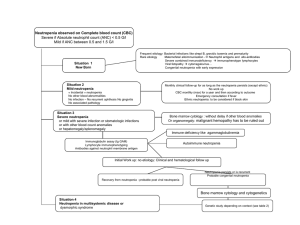
FEBRILE NEUTROPENIA WHERE DO WE STAND? Dr. / Khaled Abulkhair, PhD Medical Oncology SCE, Royal College Assistant Professor of clinical Oncology Mansoura University • Gary H. Lyman and Kenneth V. I. Rolston: How We Treat Febrile Neutropenia in Patients Receiving Cancer Chemotherapy. jop.ascopubs.org , May, 2010. • Management of febrile neutropenia: ESMO Clinical Practice Guidelines, Annals of Oncology 21 (Supplement 5): v252–v256, 2013 • NCCN guidelines, supportive care, infection in cancer patients, 2014. • Guidelines for the Management of Febrile Neutropenia in Oncology Patients, Nottingham Antibiotic Guidelines Committee, http://nuhnet/diagnostics_clinical_support /antibiotics , Dec 2009 • IDSA guidelines 2010 WHAT IS YOUR JOB? If your patient is a 65 y.o known metastatic NSCLC with the following co-morbidities; COPD, hypertensive, and cirrhotic liver with maintained LFT presented post his first cycle of Docetaxel + Carboplatin with severe oral mucositis and fever. CBC showed Neutropenia. - What would be his risk dying of his infection? Fever in the setting of neutropenia is considered a medical emergency requiring immediate evaluation and administration of empiric broad-spectrum antibiotics.1 Early studies demonstrated that patients with febrile neutropenia not promptly treated often experience a rapidly fatal outcome, most notably because of Gram negative bacteremia.2 Recent studies of unselected patients with cancer with febrile neutropenia have reported rates of mortality of 5% to 20%, increasing in direct proportion to the number of major infectious complications and comorbid medical conditions (Fig 1)3. SIMPLE MESSAGES Always remember infection can kill. Febrile Neutropenia is a medical Emergency. Be prepared and updated. How to improve our practice? NEUTROPENIA Can vary depending on institution: • Usually defined as absolute neutrophil count (ANC) <1000-1500 cells/microliter…How to Calculate • ANC = WBC (cells/microliter) x %(PMNs + bands) /100 Further categorized as: • Severe (ANC <500) • Moderate (ANC between 500-1000), variable hospitalization requirement • Mild (ANC 1000-1500), which can typically be managed as OPD • F.N is defined as Fever 38.30 or 380 over 1 h with ANC of 500 /mm3 or less or a count of less than 1000/mm3 with expected drop to below 500/mm3 in the next 48 hours. • Remember: • Neutropenic patient can present w/o fever despite infection especially in elderly patients, those on steroids, and or paracetamol. • Deal with patients on chemotherapy who are critically ill, hypotensive, tachcardiac or desaturated as being F.N untill proven otherwise. • Risk of infection and severity of infection related to ANC level and duration of neutropenia. • Neutropenia can occur via 4 mechanisms: • Decreased production • Ineffective granulopoiesis • Shift of circulating PMNS to vascular endothelium or tissue pools • Enhanced peripheral destruction • 2 Categories • Acquired • Congenital • 2 Categories • Acquired • Congenital • Acquired: • Most common is post infectious (bacterial, viral, parasitic, rickettsial) • 2nd most common is drug induced: • Drugs with highest risk: clozapine, antithyroid drugs, antidiabetics, chloramphenicol, cytotoxics (post chemo….), bactrim and sulfasalazine. • Hypersplenism • Bone marrow disorders (aplastic anemia, leukemias, myelodysplasia, neutropenia is not isolated defect in cases like these) INITIAL ASSESSMENT Guidelines are not a substitute for a good clinical judgment. • First and most imp…..listen to your patient: Do not forget to ask about any CNS manifestations. • Thorough physical examination: Vital signs including pain… What is meant by hemodynamic instability? Pay attention for VAD Perianal inspection: avoiding digital exams or rectal temps INVESTIGATIONS • Investigations should include: CBC diff, Basic chemistries, Cultures from all potential sites, along with two sets of blood cultures from peripheral veins or one set each from a peripheral vein and a central VAD. Do not discard the first few cm of blood from VAD Chest radiographs. o Other investigations are guided by the clinical situation. o Although a specific organism will not be found in more than half of patients with F.N, a presumptive diagnosis of infection is important. o (DTTP), which is the difference in time between positivity of results between catheter culture and peripheral blood culture. A DTTP of ‡2 h is a highly sensitive and specific indicator of catheter-related bacteremia. o All cases of catheter-related infection (CRI) in the setting of FN require decision making on the choice and duration of i.v. antibiotics, and the need for catheter removal. o When CRI is suspected, and the patient is stable, the catheter should not be removed without microbiological evidence of infection [ESMO,2010]. THE UGLY TRUTH Patient presented to his assigned clinic, he cannot come in a different day? Lucky if someone noticed he is febrile and needs admission! Few hours passed till he is admitted. No Antibiotics till next day. At 7-8 PM, the Resident call the senior staff asking what to do ? Do cultures? Give antibiotics? Send to ICU? IF YOU ARE AN ONCOLOGIST....DO NO HARM Urgent assessment…any time any day is needed Urgent Admission Urgent treatment within 30-60 mint of presentation! Urgent ICU referral if needed • Currently, Gram-positive organisms are the predominant bacterial pathogens in this setting, with coagulase-negative staphylococci, Staphylococcus aureus, Enterococcus spp., and viridans group streptococci being isolated most often.4 • Among Gram-negative bacilli, Escherichia coli, Klebsiella spp., and Pseudomonas aeruginosa remain the predominant species, although other Enterobacteriaceae, Stenotrophomonas maltophilia, and Acinetobacter spp. are isolated frequently.5 o Approximately 10% to 15% of bacteremias are polymicrobial, with Gram-negative bacilli being isolated from more than 80% of these infections.6 o Resistance to Antimicrobials o Of particular concern, more than 50% of Staphylococcus aureus isolates are MRSA, and vancomycin resistance among enterococci constitutes nearly 30% of enterococcal isolates. o Local epidemiological bacterial isolates and resistance patterns are crucially important in determining firstchoice empirical therapy, since coverage for MRSA or resistant Gram-negative bacteria may be required (ESMO,2010). MANAGEMENT Best way to treat F.N is to prevent its occurrence. Prophylaxis is a big subject with many controversies will be discussed in another session. Empiric, broad-spectrum antibiotic therapy should be administered promptly to all patients with febrile neutropenia. 9 Patients’ risk should be quickly assessed to determine …mono or combinations, hospital or home. Low-risk patients may be defined as ambulatory patients with good performance status and no serious comorbidity and anticipated short duration of severe neutropenia or those with an index score of 21 or more.11 RISK STATUS ASSESSMENT Is my patient in need for Vancomycin? Catheter-related infection/Port tunnel infection/cellulitis Gram-positive organisms on blood culture Hypotension Mucosal damage e.g. (CCRT) Colonization with penicillin-resistant pneumococci or methicillinresistant Staphylococcus aureus. Should I start G-CSF? G-CSF should not be used routinely in the treatment of established febrile neutropenia, although they may be considered in patients at increased risk for serious complications including mortality, ANC ≤ 100, and or age ≥ 65 with comorbidities. G-CSF use is discouraged in afebrile neutropenia! Should I call ICU? CONTINUATION OF ANTIBIOTIC TREATMENT SPECIAL SITUATIONS SIMPLE MEASURES AND ONGOING CARE • Monitor CBC diff and biochemical profile daily. • Assess intravenous sites daily for any signs of infection. • Assess the oral cavity status every 12 hours. • Assess the skin daily for breakdown, lesions, rashes etc. • Assess any wounds for signs of infection. • Assess for any change in urinary function including dysuria frequency, and hematuria. • Assess for any changes in bowel habit. • Assess female patients for vaginal candidiasis. • Assess patients for any signs of peri-anal infection. SIMPLE MEASURES AND ONGOING CARE • Patients will be cared for in an environment that minimizes the risk of infection from other patients, staff and visitors. • Protected isolation must be clearly indicated as per the policy. • Educate the patient and relatives about the need to restrict visitors with transmissible illnesses Or recently vaccinated with live vaccines. • Careful hand washing is the single most important action for the health professional, patient, the patient’s family and visitors, in preventing cross infection. • Fresh flowers, plants should not be placed in the patient’s room. • Denture mugs and soap dishes should also be removed. • Food may be a source of infection and dietary restrictions may be necessary. • Sanitary towels should be used instead of tampons. • Ensure patients are encouraged/assisted to shower daily. • The rooms should be cleaned daily and all surfaces damp dusted. LIST OF DONOT DO Do not underestimate F.N; it can kill. Do not take too much time to give first dose of Antibiotics. Do not wait for Lab results…. Use your clinical judgement. Do not do PR examination. Do not forget… you are caring for a whole patient not only F.N. Do not hesitate calling for help from ICU if needed. Do not stop treatment early…relapse of not-fully treated infections is dangerous. Do not forget to adjust doses of chemotherapy for the subsequent cycles and or Renal/Liver impairment. THE FUTURE….I HOPE WILL NOT BE UGLY • Post chemotherapy Note Card. • Emergency admission any day anytime. • Resident: “Hello Dr/Khaled. Mr/Ahmed has a temp of 39C, neutrophils are 0.1. He is quite well, BP 140/70, pulse 100, and sats 95%. I have taken cultures, and I have given first doses of antibiotics”, Do you have anything more to add? REFERENCES • 1- Hughes WT, Armstrong D, Bodey GP, et al: 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34:730-751, 2002 • 2- Bodey GP, Buckley M, Sathe YS, et al: Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med 64:328-340, 1966. • 3- Kuderer NM, Dale DC, Crawford J, et al: Mortality, morbidity, and cost associatedbwith febrile neutropenia in adult cancer patients. Cancer 106:2258-2266, 2006. • 4- Yadegarynia D, Tarrand J, Raad I, et al: Current spectrum of bacterial infections in patients with cancer. Clin Infect Dis 37:1144-1145, 2003. • 5- Safdar A, Rolston KV: Immunocompromised hosts: Stenotrophomonas maltophilia— Changing spectrum of a serious bacterial pathogen in patients with cancer. Clin Infect Dis 45:1602-1609, 2007. • 6- Rolston KV, Bodey GP, Safdar A: Polymicrobial infection in patients with cancer: An underappreciated and underreported entity. Clin Infect Dis 45:228- 233, 2007. 7- Klastersky J, Ameye L, Maertens J, et al: Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents 30:S51-S59, 2007 (suppl 1). 8- Rolston KV: Challenges in the treatment of infections caused by gram positive and gram negative bacteria in patients with cancer and neutropenia. Clin Infect Dis 40:S246-S252, 2005 (suppl 4). 9- Hughes WT, Armstrong D, Bodey GP, et al: 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34:730- 751, 2002. 10- Kern WV: Risk assessment and treatment of low-risk patients with febrile neutropenia. Clin Infect Dis 42:533-540, 2006. 11- Klastersky J, Paesmans M, Rubenstein EB, et al: The Multinational Association for Supportive Care in Cancer risk index: A multinational scoring system for identifying low -risk febrile neutropenic cancer patients. J Clin Oncol 18:3038-3051, 2000. 12- Rolston KVI, Frisbee-Hume SE, Patel S, et al: Oral moxifloxacin for outpatient treatment of low-risk, febrile neutropenic patients. Support Care Cancer 18:89-94, 2010. 13- Klastersky J, Paesmans M, Georgala A, et al: Outpatient oral antibiotics for febrile neutropenic cancer patients using a score predictive for complications. J Clin Oncol 24:41294134, 2006