Therapeutic Approaches
advertisement

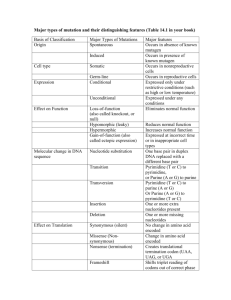
NEW CONCEPTS IN VASOACTIVE THERAPY Jerrold H Levy, MD Professor of Anesthesiology Deputy Chairman for Research Emory University School of Medicine Cardiothoracic Anesthesiology and Critical Care Emory Healthcare Atlanta, Georgia VASOACTIVE THERAPY Vasodilators BP = SVR X Beta Blockers Other agents CO (SV x HR) Vasoconstrictors Inotropes PHARMACOLOGIC APPROACHES FOR BIVENTRICULAR DYSFUNCTION PERIOPERATIVELY AND IN THE ICU • Vasodilator therapy • Pulmonary vasodilators • Inotropic agents – PDE inhibitors – Catecholamines – Inhaled NO – Phosphodiesterase • Prostaglandin inhibitors s – Digoxin, calcium , • New agents T3 Nesiritide, Levosimendan Bailey JM, Levy JH: Cardiac surgical pharmacology. Edmunds H (ed), McGraw Hill, New York, pp. 225-254, 1997. Levy JH: Milrinone. Ann Thorac Surg 2002;73:325-30. Levy JH: Postoperative circulatory control. Cardiac Anesthesia, 1233-1258, 4th Edition, W.B. Saunders, Philadelphia, 1998. VASODILATORS(1) • • • • • • • ACE inhibitors Adenosine A-II antagonists Alpha1 adrenergic antagonists Alpha2 adrenergic agonists BNP (nesiritide) Beta2 adrenergic agonists VASODILATORS(2) • • • • • • • Calcium channel blockers Dopamine1 agonists Hydralazine Nitrovasodilators Nitric oxide Phosphodiesterase inhibitors Prostaglandins SELECTIVE VASODILATORS • Nitroglycerin: due to selective metabolism to nitric oxide • Inhaled nitric oxide: due to optimizing ventilation/perfusion ratios and minimizing intrapulmonary shunting Mechanisms of Nitrate Tolerance • • • • • Decreased bioconversion to nitric oxide1 Cellular depletion of sulfhydryl groups2,3 Neurohumoral adaptations4 Superoxide anion production5 Upregulation of endothelin 16 1. 2. 3. 4. 5. 6. Münzel T. Am J Cardiol. 1996;77:24C-30C. Parker JD, Parker JO. N Engl J Med. 1998;338:520-531. Needleman P, Johnson EMJ. J Pharmacol Exp Ther. 1973;184:709-715. Münzel T, et al. J Am Coll Cardiol. 1996;27:297-303. Münzel T, et al. J Clin Invest. 1995;95:187-194. Münzel T, et al. Proc Natl Acad Sci. 1995;92:5244-5248. Nitrovasodilators Sodium Nitroprusside NO+ CN CN Na+ CN Fe++ CN Na+ CN NITROPRUSSIDE THERAPY • Potent venodilator/arterial vasodilator • Cardiac output is often affected due to venodilation • Volume replacement is often required for venodilation Limitations of Nitrovasodilators for Acute Heart Failure • Nitroglycerin – Efficacy in CHF ±1 – Tachycardia2 – Tachyphylaxis3 – Neurohormonal activation due to reflexive sympathetic activity4 1 2 3 4 5 • Nitroprusside – Difficult titration – Arterial line monitoring due to excessive hypotension risk3 – Tachycardia3 – Coronary steal3 – Pulmonary shunting3 – Thiocyanate toxicity3 – Neurohormonal activation due to reflexive sympathetic activity4,5 Publication Committee for the VMAC Investigators. JAMA 2002; 287 (12): 1531-40. Robertson R, et al. ''Chapter 32: Drugs Used for the Treatment of Myocardial Ischemia'' in Pharmacologic Basis of Therapeutics,Goodman and Gilman, Eds. 9th. Edition 1996, McGraw-Hill. Kelly and T Smith, ‘‘Chapter 34: Pharmacologic Treatment of Heart Failure’‘, in The Pharmacologic Basis of Therapeutics, 9th. Ed. Goodman and Gilman, eds. 1996 McGraw-Hill. Abraham W. Natriuretic peptides in heart failure. Heart Failure 1996; 12:391-393. J Oates, J. Chapter 33: Antihypertensive Agents and Drug Treatment of Hypertension’‘, in The Pharmacologic Basis of Therapeutics, 9th. Ed. Goodman and Gilman, eds. 1996 McGraw-Hill. MAINSTAY VASOACTIVE THERAPY FOR ACUTE HEART FAILURE IN CRITICALLY ILL PATIENTS • • • • • • Diuretics Dobutamine Enalaprilat Milrinone Nesiritide Nitrovasodilators MAINSTAY IV THERAPY FOR HYPERTENSION IN CRITICALLY ILL PATIENTS • Beta adrenergic blockers • Dihydropyridine (DHP) calcium channel blockers (Nicardipine IV) • Enalaprilat • Hydralazine • Nitrovasodilators (nitroprusside and nitroglycerin IV DHP CALCIUM CHANNEL BLOCKERS • 1st generation: nifedipine • 2nd generation: nicardipine, isradipine • 3rd generation: clevidipine DHP CALCIUM CHANNEL BLOCKERS:CLINICAL APPLICATIONS • • • • No effects on SA/AV node No myocardial depression Cerebral and coronary vasodilator Important applications in the ICU and perioperative management of neuro and CV disease. Has also been reported for pregnancy induced hypertension • Nicardipine is the first IV drug of this class available in the US (94) HEMODYNAMIC EFFECTS OF IV NICARDIPINE HR MAP PAOP MPAP RAP CI LV LVEF Control 71 ± 13 107 ± 14 9±4 15 ± 3 8±3 2.2 ± 0.3 1509 ± 376 57 ± 9 Nicardipine 70 ± 14 80 ± 9 8±3 16 ± 4 8±2 2.8 ± 0.4 1680 ± 485 68 ± 7 Lambert CR: Am J Cardiol 1993;71:420 HEMODYNAMIC EFFECTS OF IV ISRADIPINE Variable SBP DBP Baseline 150 ± 20 75 ± 9 30 Minutes -30 ± 30‡ -18 ± 8.0‡ MAP HR CI 101 ± 10 89 ± 12 2.7 ± 0.6 -23 ± 11.0‡ 4 ± 12* 0.4 ± 0.6‡ SVR SVI PADP PCW 470 ± 417 0.0310 ± 0.006 13.4 ± 3.9 11.7 ± 4.3 -478 ± 281‡ 0.004 ± 0.006† 0.2 ± 3.2 -0.0 ± 3.0 PVR 1.25 ± 0.9 -0.05 ± 0.47 Leslie: Circulation. 1994 Nov;90(5 Pt 2):II256 Should a moratorium be placed on sublingual nifedipine capsules given more hypertensive emergencies and pseudo emergencies? Gross et al: JAMA 1996:276;1342-3 Nicardipine IV Dosing (PI) • • Initiation: 5 mg/hr (50 ml/hr) Titration for gradual BP reduction: • For more rapid BP reduction: • Maintenance: Following achievement of BP goal, adjust infusion rate to 3 mg/hr, (30 ml/hr) rate 2.5 mg/hr (25 ml/hr) q 15 min to a maximum of 15 mg/hr (150 ml/hr) until blood pressure reduction achieved rate 2.5 mg/hr (25 ml/hr) q 5 min to a maximum of 15 mg/hr (150 ml/hr) until blood pressure reduction achieved Nicardipine IV Dosing (FRANCE) • For hypertensive urgency, Rx should be adapted so BP decrease is not >25% in 1 hr to avoid myocardial, cerebral or renal ischemia. • Rapid effect: 1 mg/min to 10 mg • Progressive effect: 8-15 mg/h to 30 min, then 2 to 4 mg/h maintenance • Infant: 1 to 2 mg/m2 of body surface in 5 minutes. Ref: http://www.biam2.org/www/Spe4359.html#Voie Clevidipine in CABG: a dose-finding study. Bailey JM et al:Anesthesiology 2002;96:1086 • Clevidipine, an ultrashort acting agent, decreased MAP and SVR, without changes in heart rate, CVP, PAOP, or CI at increasing doses. • The early phase of drug disposition had a half-life of 0.6 min. The context-sensitive half-time <2 min for up to 12 h of administration. • CONCLUSION: Clevidipine is a dihydropyridine CCB that lowers BP without changing heart rate, CI, or cardiac filling pressures. Fenoldopam (Corlopam) • Selective vascular DA1 agonist • Produces arterial vasodilation, increases renal perfusion, and natruresis • Short duration of action/half life • Approved in June 1997 • Expense and potency are major issues NOVEL AGENTS: Nesiritide (Human B-type Natriuretic Peptide) Natriuretic Peptides: The Heart as a Secretory Organ •Secretory granules found on EM of atria. Kisch, Exp Med Surg 1956 •Balloon catheter in atria of dogs resulted in diuresis: Henry and Pearce, J Exp Phys 1956 •Homogenized atrium injected IV cuases natriuresis, diuresis. DeBold, Life Sciences, 1981 •ANP identified in 1984. Kangawa •BNP identified in 1988 in porcine brain. Nature, 1988 •Amino acid sequence and DNA clones: Sudoh et al, 1988 and Seilhamer et al, 1989 Natriuretic Peptides NH 22N- Ser H2N- Ser Pro ANP Leu Arg Arg Gly Phe Ser Ser Gly Arg Asp S S COOH- Gin Gly Ser IIe Gly Leu Arg Gly Ser Gly Phe Arg Lys Met Asp Gly Cys Gly Cys Ser Phe BNP Val Arg Cys Asn Lys Met Met Ala Gin Arg IIe S S Tyr Val Ser Cys Lys Gly Ser Leu Leu Arg Gly Ser Ser Arg HOOC- His Pro Ala Thr Arg Ser Urodilatin Leu Arg Arg Gly Phe Ser NH NH2 Ser Cys Gly Arg Arg IIe S S Ser Phe Arg HOOC- Tyr Cys Asn Gly H H2N- Gly Leu Met Asp Gly Ala Leu Gin Gly Ser CNP Gly Phe Ser Lys Gly Leu Lys Leu Asp Arg Cys IIe S S HOOC- Cys Gly Gly Ser Leu Gly Ser Met hBNP for Rx of decompensated heart failure Nesiritide (h-BNP) is identical to the endogenous naturally occurring hormone, with identical pharmacological profile D M K R G F S P K M V Q G S R I S S C G S S S S G L H G R C R K V L 32 amino acid sequence Recombinant technology using E-coli NOTE: hBNP affects assay for BNP, but can still use proBNP or one of the proANP assays Physiology of Natriuretic Peptides + Cardiac Wall Stress - Urodilatin ANP+BNP Neutral Endopeptidases Clearance CNP NPR-A/NPR-B NPR-B ?NPR-D NPR-C Decreased Vascular Growth Decreased Blood Pressure Increased Na/H20 Excretion Adapted from Wilkins MR. Redondo J. Brown LA. Lancet 1997;349:1307-1310 B-Type Natriuretic Peptide (BNP) Physiologic Effects • Systemic Hemodynamic – Preload reduction1,5 – Afterload reduction1,5 – Increased CI1,5 – No tachycardia1,5 • Neurohormonal • Coronary Arteries – Vasodilates2,3 • Renal – Diureses and natriuresis1 – Increased filtration fraction6 – GFR effect variable6 1Colucci – Decrease endothelin-14 – Inhibit RAA axis1,5 – Decrease norepinephrine5 WS, et al. NEJM 2000; 343(4):246-253 Kato H. Yasue H. Yoshimura M.Tanaka H. Miyao Y. Okumura K. Am Heart J 1994; 128: 1098-1104 3 Okumura K, et al. J Am Coll Cardiol 1995 Feb;25(2):342-8. 4Aronson D, et al. J Am Coll Cardiol, February 2001. Abstract from Poster Session 1046 5Abraham WT, et al. J Card Failure 1998; 4(1): 37-44 6Jensen KT, et al. Clinic Sci 1999;96:5-15 2 Clearance Pathways Vascular Smooth Muscle Cell GC= Guanylate Cyclase GC-A GTP G/C cGMP GC-B Biological Effects G/C hBNP ? NP-C NP=neutral endopeptidase Clearance receptor clearance pathway Nakao et al Can J Physiol Pharmacol, 1991, 69: 1500-1506 Neurohumoral Activation in Heart Failure Myocardial injury Fall in LV performance Activation of RAAS, SNS, ET, and others Myocardial toxicity - ANP BNP Peripheral vasoconstriction Hemodynamic alterations Remodeling and progressive worsening of LV function Heart failure symptoms Morbidity and mortality The Natriuretic Peptide System is Overwhelmed in Acute Decompensated Heart Failure ANP BNP Endothelin Aldosterone Angiotensin II Epinephrine Adapted from Burnett JC, J Hypertens 1999 Natriuretic Peptide System Sympatho-inhibitory ET inhibition Vasodilation ANP BNP ANP ANP BNP CNP ANP BNP Antiproliferation effect BNP ANP BNP Anti-fibrotic Lusitropic Vasodilation •veins •arteries •coronaries •pulmonary Aldosterone inhibition Natriuresis Renin inhibition Pharmacologic Actions of Human BNP R I SS D S M S K G R L G H G F R C C S S K V LR G S PK M V Q GS Cardiac • lusitropic • anti-fibrotic • anti-remodeling Hemodynamic veins arteries coronary arteries Neurohumoral aldosterone endothelin-1 norepinephrine Renal diuresis natriuresis Nesiritide Reconstitution and Standard Dosing • 1.5 mg vial reconstituted with 5 mL NS, 1/2NS, 1/4NS, or D5W • Add 5 mL from reconstituted vial into 250 mL bag for a final concentration of 6 mg/mL • Administration via peripheral IV or non-heparin coated central line catheter Standard Dosing: 2 mcg/kg bolus + 0.01 mcg/kg/min continuous infusion • Bolus volume (ml): Patient weight (Kg) / 3 • Infusion (ml/hour): 0.1 x patient weight (Kg) • Duration: Dependent on clinical need – NO maximum duration NB: Most patients are expected to be managed without dose adjustment Nesiritide Clinical Summary • Nine clinical trials in CHF. Over 900 CHF patients studied. • Trials included patients with ACS, renal disease, serious arrhythmias • Studied with a wide variety of concomitant medications Summary of Trial Data: • Improves hemodynamics and CHF symptoms such as dyspnea • Decreases diuretic need and/or increases urine output • Suppresses neurohormones • More effective than IV NTG • No tachyphylaxis • No tachycardic or proarrhythmic effects • Can be used safely with b-blockers • Hypotension is the major side effect NOVEL AGENTS: Levosimendan Calcium Sensitisation by Levosimendan • Enhanced contractility of myocardial cell by amplifying trigger for contraction with no change in total intracellular Ca2+ Effects of Opening ATP-Sensitive Potassium Channels • Reduces preload and afterload • Increased coronary blood flow (Lilleberg et al. Eur Heart J. 1998;19:660-668.) • Anti-ischemic effect (Kersten et al. Anesth Analg. 2000;90:5-11;Kaheinen et al. J Cardiovasc Pharmacol. 2001;37:367-374.) Opening of ATP-Sensitive Potassium Channels •Activation of KATP channels in coronary vascular smooth muscle (Kaheinen J Cardiovasc Pharmacol. 2001;37:367374.) •Results in venous, arterial, and systemic vasodilation Pharmacokinetic Profile • Active drug (t1/2= 1h) – Rapid onset of action – Titratability • Active metabolite (t1/2= ~80h) – Sustained hemodynamic response VasoactiveTherapy.com