Arrhythmias: Hyperfunction
advertisement

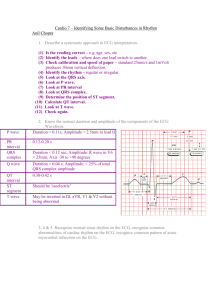
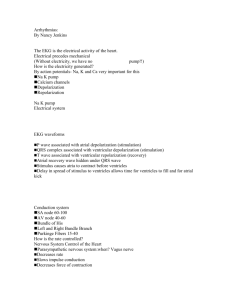
Dysrhythmias EKG DANCE-click here Dysrhythmias Abnormal cardiac rhythms are termed dysrhythmias. Prompt assessment of dysrhythmias and patient’s response to the rhythm is critical. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 2 EKG shows electrical activity of the heart. Electrical precedes mechanical (Without electricity…no pump!!) Click here How is the electricity generated? By action potentials (click for animated visuals) Na K pump (animation) Calcium channels Depolarization-contraction RepolarizationThink about this when administering cardiac meds…antidysrhytmics *ECG wave forms- Produced by movement of charged ions across the semipermeable membranes of myocardial cells. Click hereYouTube- How Body Works-A Nerve Impulse Understanding cardiac action potential & meds Cardiac action potential of a fast-response Purkinje fiber. Arrows indicate the approximate time and direction of movement of each ion influencing membrane potential. Ca++ movement out of the cell is not well defined but is thought to occur during phase 4 Key Characteristics of Cardiac Cells Multimedia Tutorials *Great site Cardiac cells- either contractile cells influencing pumping action or pacemaker cells influencing electrical activity of heart Automaticity Excitability Conductivity Contractility *Refractoriness Relative Absolute Each beat generated from same pacemaker - look identical. Impulses from other cardiac cells = “ectopic” (PVC, PAC) Electrical activity produces mechanical activity= waveforms Refractory Period Myocardial cells resistive to stimulation; **dysrhythmias triggered during relative refractory and absolute refractory periods •Absolute refractory period: no depolarization can occur- from Q wave until middle of T wave •Relative refractory period: greater than normal stimulus needed for depolarization (contraction); goes through 2nd half T wave Conduction System of the Heart Fig. 32-4. A, Conduction system of the heart. AV, Atrioventricular; SA, sinoatrial. B, The normal electrocardiogram (ECG) pattern. The P wave represents depolarization of the atria. The QRS complex indicates depolarization of the ventricles. The T wave represents repolarization of the ventricles. The U wave, if present, may represent repolarization of the Purkinje fibers or it may be associated with hypokalemia. The PR, QRS, and QT intervals reflect the length of time it takes for the impulse to travel from one area of the heart to another. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 8 Intrinsic rates Yellow = isoelectric phase. SA node 60-100 AV node 40-60 Bundle of His; Left and Right Bundle Branch; Purkinge Fibers 15-40 Purple= "P"wave. Purple and yellow split = "PR" interval Red = "Q" wave; Light blue = “R" wave Light green = "S" wave; Black = "ST" segment Orange = "T" wave; Yellow again = isoelectric. Dark blue ="U" wave (seldom seen)* risk for *hypokalemia, med effect, hypercalcemia, . EKG waveforms P wave associated with atrial depolarization (stimulation) QRS complex associated with ventricular depolarization (stimulation) T wave associated with ventricular repolarization (recovery) Atrial recovery wave hidden under QRS wave Stimulus causes atria to contract before ventricles Delay in spread of stimulus to ventricles allows time for ventricles to fill and for atrial kick Pacemakers other than *SA node •Pacemaker from another site > lead to dysrhythmias; may be discharged in number of ways. oSecondary pacemakers- may originate from AV node or His-Purkinje system. oSecondary pacemakers can originate when they discharge more rapidly than normal pacemaker of SA node. oTriggered beats (early or late) may come from ectopic focus (area outside normal conduction pathway) in atria, AV node, or ventricles. How is rate controlled? Nervous System Control of Heart Parasympathetic nervous system: when? Vagus nerve Dec. rate Slows impulse conduction Dec. force of contraction Sympathetic nervous system: when? Inc. rate Inc. force of contraction EKG graph paper Horizontal measures time Vertical measures voltage Helps to determine rate Width of complexes Duration of complexes Graphic tracing of electrical impulses produced by heart; waveforms of ECG represent activity of charged ions across membranes of myocardial cells. Each small square box on the graph paper is equal to: 1. 2. 3. 4. 0.06 sec. 0.08 sec. 0.04 sec. 0.20 sec. If you didn’t know, look at previous slide- 0.04 Cardiac Monitoring- based on 12 lead EKG Each lead has positive, negative and ground electrode. Each lead looks at different area of heart. *Can be diagnostic as in case of an MI RNCEU’s Lead II positive R arm looking to LL neg 3 lead placement: Depolarization wave moving toward a positive lead will be upright. Depolarization wave moving toward a negative lead will inverted. Depolarization wave moving between negative and positive leads will have both upright and inverted components. *Five lead placement allows viewing all leads within limits of monitor Leads to monitor EKG Best- lead II and MCL or V1 leads- lead II easy to see P waves. MCL or V1 easy to view ventricular rhythms. If impulse goes toward positive electrode complex is positively deflected or upright If impulse goes away from positive electrode complex is negatively deflected or goes down form baseline Five lead system- uses all leads shown: three lead system uses only black, white and red leads. Two lead telemetry systems use black and red leads- placement may change depending on what EKG lead (view) is required. Black and white leads are placed on shoulder area; green and red leads placed on lowest rib on both sides of torso, and brown lead (ground) is placed at 4th intercostal space, just to right of sternum. (follow guidelines of facility) Lead Placement Fig. 36-4. A, Lead placement for MCL, using a three-lead system. B, Lead placement for V1 or V6 using a five-lead system. C, Typical electrocardiogram tracing in lead MCL1. C, Chest; LA, left arm; LL, left leg; MCL, modified chest lead; RA, right arm; RL, right leg. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 18 Risk Factors for Dysrhythmia (Arrhythmia) Hypoxia Structural changes Electrolyte imbalances Central nervous system stimulation Medications Lifestyle behaviors Who is/are at Greatest Risk for Dysrhythmia? Patient(s) with 1. COPD 2. MI MI; valvular disease (best two answers3. Valvular disease have high risk for hypoxia (MI) and structural 4. Colon resection chg with valvular) Evaluation of Dysrhythmias Holter monitoring Event recorder monitoring Exercise treadmill testing Signal-averaged ECG Electrophysiologic study Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 20 Calculate rate (*know how to do this) Count Big block Little block Number of R waves in 6 sec times 10 Calculate rhythm-reg or irreg Measure PR interval, <0.20 QRS interval .04- 0.12 P to QRS relationship *Recognize artifact 1. Number of QRS complexes in 1 minute R-R intervals in 6 seconds; multiply by 10 2. Number of small squares between one R-R interval; divide this number into 1500 3. Number of large squares between one R-R interval; divide this number into 300 Rate Calculation 1 lg box= .20 5 lg boxes =1 sec *Therefore 300 lg boxes in 1 min. 30 lg boxes =6 secs Each small box = 0.04 seconds on horizontal axis and 1 mm or 0.1 millivolt on vertical axis. PR interval-measured from beginning of P wave to beginning of QRS complex; QRS complex -measured from beginning of Q wave to end of S wave; QT interval measured from beginning of Q wave to end of T wave; and TP interval- measured from end of T wave to beginning of next P wave. If there are 10 small squares between 2 QRS waves, the rate would be: 1. 2. 3. 4. 75 100 150 100 *Rate 150; 1500 / 10 = 150 Normal Sinus Rhythm Follows normal conduction pattern Normal P wave PR interval<.20 QRS.04-.12 T wave for every complex Rate is regular 60-100 *Rate >100: Sinus Tachycardia Causes-anxiety, hypoxia, shock, pain, caffeine, drugs Treatment-eliminate cause Sinus Bradycardia- brady heart song Normal in sleep; aerobically trained athlete Clinical assoc.: Response to carotid sinus massage; hypothermia; inc vagal tone; adm. parasympathomimetic drugs (Beta blockers; digoxin), head injuries (inc ICP), inferior MI, hypothyroidism Sinus node fires <60 bpm; Normal conduction; rhythm regular; P: QRS: 1:1; PR interval: 0:12 to .20 sec.; QRS complex: 0.04 to 0.12 sec Clinical significance- Dependent on symptoms Hypotension Pale, cool skin Weakness Angina Dizziness or syncope; shortness of breath Confusion or disorientation Shortness of breath Treatment- if symptomatic, atropine or pacer Sinus BradycardiaTreatment- if symptomatic, atropine or pacer Patients with bradycardia are likely to display which of these symptoms: 1. 2. 3. 4. Heart rate less than 60 Dizziness Hypertension Confusion 1. 2. 3. 4. Heart rate less than 60 Dizziness Hypertension (all except) Confusion Sinus Tachycardia Rhythm: Rate: P Waves: PR Interval: QRS Complex: Regular Fast (>/= 100 bpm) “Normal” and upright, one for each QRS “Normal” (0.12-0.20 seconds) “Normal” (0.08-0.12 seconds) •Due to inc. in rate of sinus node discharge (vagal inhibition). •Common dysrhythmia; many causes as exercise, fever, caffeine, anxiety, smoking, heart failure, hypovolemia, etc. •Treatment : address underlying cause and/or determine if it is even a problem (Medsadenosine?, beta adrenergic blockers (dec. heart rate & myocardial oxygen consumption)*, antipyretics for fever); analgesic for pain Clinical significance Dizziness and hypotension due to decreased CO Inc. myocardial oxygen consumption may lead to angina Name these rhythms & count rate!! (What you just covered) Sinus Dysrhythmias (Arrhythmia) (SA) Rate 60-100 Irregular rhythm- increases with inspiration, decreases with expiration P, QRS,T wave normal Cause- children, drugs (Morphine sulphate), MI Treatment- none Sinus Arrest •See pauses •May see ectopic beats (PAC’s PVC’s)*don’t treat •Due to MI •Treatment Atropine Isoproterenol (Isuprel) Pacemaker Isoproterenol-synthetic sympathomimetic amine Atrial Dysrhythmias Atria is pacemaker Atrial rate contributes 25-30% of cardiac reserve Serious in patients with MI- WHY? Medications - to treat atrial dysrhythmias (if patient symptomatic) •Diltiazem (Cardizem) (Identify class) •Amiodarone (Cordarone) (Identify class) •Dofetilide (Tikosyn) (Identify class) Verapamil (Calan) (Identify class) Metoprololol (Lopressor) Identify class Digoxin (Lanoxin) Atropine Think-rate too slow, too fast?? Ref to Tab. 36-9-next slide Premature Atrial Contraction (PAC’s) P wave abnormally shaped-contraction originates from ectopic focus in atrium other than SA Node PR interval shorter-travels abnormal pathway (distorted “P” waves) QRS normal Cause-age, MI, CHF, stimulants, dig, electrolyte imbalance; valvular disease; hypoxia Treatment- remove stimulants; watch for SVT, depends upon cause; isolated not significant; B-adrenergic blockers Supraventricular Tachycardia (SVT)/PSVT (paroxysmal SVT) Rate- 150-250 (Very fast!) Originates in ectopic focus above bifurcation of bundle of His- atria=pacemaker (may not see p waves); *Paroxysmal = abrupt onset and termination Cause-SNS stimulation, MI, CHF,sepsis SVT/Paroxysmal Supraventricular Tachycardia (PSVT) Clinical significance Prolonged episode and HR >180 bpm may precipitate ↓ CO Palpitations Hypotension Dyspnea Angina •Treatment•Meds: adenosine, digoxin, diltiazem (Cardizem) or verapamil (calcium channel blockers), propranolol (inderal), dofetilide (Tikosyn) •Vagal stimulation This YouTube site explains supraventriventricular tachycardias plus atrial flutter and atrial fibrillation- Click here to locate additional videos Atrial Flutter Rate of atria is 250-300, vent rate varies Regular rhythm P waves saw tooth, ratio 2:1, 3:1, 4:1 Flutter waves-*Originate from single ectopic focus; No PR interval Cause-diseased heart (mitral valve), PE, chronic lung; hyperthyroidism, drugs as dig, quinidine, epinephrine 3:1 flutter Video Atrial flutter Atrial Flutter Clinical significance High ventricular rates (>100) and loss of the atrial “kick” can dec. CO and precipitate HF, angina Risk for stroke due to risk of thrombus formation in atria Treatment- *Goal slow ventricular resopnse Cardioversion Calcium channel blockers and beta blockers, amiodorone (What classes?) Ablation , warfarin (Coumadin) Atrial Fibrillation-**most common Rate of atria 350-600- (total disorganized rhythm); *multiple ectopic foci > loss effective atrial contraction Ventricular response irregular No P waves, “garbage baseline” Cause-#1 arrhythmia in elderly, heart disease- CAD, rheumatic heart disease, HF, cardiomyopathy, caffeine, alcohol, etc. Complications- dec. CO due to loss atrial kick and rapid ventricular response; thrombi (stroke) from blood stasis Treatment-Goal dec. ventricular rate; pvt stroke; *convert if possible); Meds: digoxin, calcium channel blockers, beta adrenergic blockers, amiodorone, cardioversion (TEE ck for thrombus) warfarin - ck PT and INR, *ablation, Maze procedure (involves open heart) or Mini Maze (modified) Atrial Fibrillation Rsult in dec. in CO due to ineffective atrial contractions (loss of atrial kick) and rapid ventricular response Thrombi may form in atria as a result of blood stasis Embolus may develop and travel to the brain, causing a stroke *Thrombus formation, pulse deficit Click to view You Tube video on Abalation for Atrial fibrillation! Dysrhythmias- AV Node AV Conduction Blocks Junctional Rhythm Dysrhythmia that originates in area of AV node AV node is pacemaker- slow rhythm (40-60) but regular impulse goes to atria from AV nodebackward); SA node failed to fire or impulse delayed or blocked at AV node P wave patterns Absent or hidden; Short < .0.12 or negative or PR interval; P wave precedes QRS inverted in II, III, and AVF or P wave hidden in QRS or P wave follows QRS QRS normal Often no treatment . Junctional Dysrhythmias Junctional Dysrhythmia Clinical significance Serves as safety mechanism when SA node has not been effective Escape rhythms should not be suppressed. If rhythms rapid >result in reduction of CO and HF Treatment If symptomatic, atropine Accelerated junctional rhythm and junctional tachycardia caused by digoxin toxicity; digoxin is held -Adrenergic blockers, calcium channel blockers, and amiodarone for rate control for junctional tachycardia not caused by digoxin toxicity DC cardioversion is contraindicated Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 44 First Degree AV Block Transmission through AV node delayed PR interval >0.20 QRS normal and regular Cause-dig toxicity, MI, CAD, vagal stimulation; hyperthyroidism, betaadrenergic drugs; calcium channel blockers, flecainaide drugs Treatment- none but watch for further blockage First-Degree AV Block Clinical significance Usually asymptomatic May be a precursor to higher degrees of AV block Treatment Check medications. Continue to monitor. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 46 Characteristics of 1st degree block include ? 1. Regular rhythm 2. Long PR interval 3. More P’s than QRS’s 4. Rate less than 100 1. 2. 3. 4. Regular rhythm Long PR interval More P’s than QRS’s Rate less than 100 Second Degree AV Block more P’s than QRS’s A. Mobitz I (Wenckebach) YouTube - Diagnosis Wenckebach PR progressively longer then drops QRS due to prolonged AV conduction; atrial impulse non-conducted and a QRS complex is blocked Cause- MI, drug toxicity Treatment- watch for type II and 3rd degree B. Mobitz II More P’s but skips QRS in regular pattern 2:1,3:1, 4:1 Constant PR interval Treatment-Pacemaker Second-Degree AV Block, Type 1 (Mobitz I, Wenckebach) Clinical significance/associations Usually result of myocardial ischemia or infarction Almost always transient; well tolerated May be a warning signal of more serious AV conduction disturbance Drugs: Digoxin, -adrenergic blockers Associated with CAD and other diseases that can slow AV conduction Second-Degree AV Block, Type 2 (Mobitz II) Clinical significance Often progresses to third-degree AV block ; associated with poor prognosis Reduced HR often results in dec. CO with subsequent hypotension and myocardial ischemia Second-Degree AV Block, Type 2 (Mobitz II) Fig. 36-16. Heart block. C, Second-degree AV block, type II, with constant PR intervals and variable blocked QRS complexes. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 51 Second-Degree AV Block, Type 2 (Mobitz II) Clinical associations Rheumatic heart disease CAD Anterior MI Digitalis toxicity Treatment If symptomatic (e.g., hypotension, angina) before permanent pacemaker can be inserted, temporary transvenous or transcutaneous pacemaker Permanent pacemaker Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 52 Mobitz type 1 or Wenchebach has a constant PR interval. 1. True 2. False Answer: False-Mobitz I (Wenckebach)PR progressively longer then drops QRS 3rd Degree AV Block Atria and ventricles beat independently (ventricular rhythm is “escape” rhythm Atrial rate- 60-100 Slow ventricular rate 20-40 No PR interval Wide or normal QRS (depends on where block is) Cause- severe heart disease, systemic diseases; meds as digoxin, beta-adrenergic blockers, calcium channels blockers Complications- dec. CO, ischemia, HF, shock, bradycardia, syncope, possible asystole Third-Degree AV Heart Block (Complete Heart Block) Fig. 36-16. D, Third-degree AV block. Note that there is no relationship between P waves and QRS complexes. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 55 Third-Degree AV Heart Block (Complete Heart Block) Treatment If symptomatic, transcutaneous pacemaker until a temporary transvenous pacemaker can be inserted Drugs (e.g., atropine, epinephrine): Temporary measure to increase HR and support BP until temporary pacing is initiated Permanent pacemaker as soon as possible Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 56 Bundle Branch Blocks *not in text- & no test items but to understand concept Left BBB Right BBB QRS.12 or greater Rabbit ears- RR’ No change in rhythm Normal bundle conduction Right Bundle Branch Block Ventricular Arrythmias Most serious Easy to recognize Premature Ventricular Contractions (PVC’s)-ectopic QRS wide and bizarre No P waves T opposite deflection of PVC Cause- 90% with MI, stimulants, dig, electrolyte imbalance Treatment- O2, lidocaine, procainamide (Pronestyl), *amiodarone, *abalation No longer prophylactic Premature Ventricular Contractions Multifocal- from more than one foci Bigeminy- every other beat is a PVC trigeminy- every third beat is a PVC Couplet- 2 PVC’s in a row Fig. 36-17. Various forms of premature ventricular contractions (PVCs). Note: Recorded from lead II. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 61 Premature Ventricular Contractions Clinical significance In normal heart, usually benign In heart disease, PVCs may dec. CO and precipitate angina and HF **Patient’s response to PVCs must be monitored PVCs often do not generate a sufficient ventricular contraction to result in a peripheral pulse **Apical-radial pulse rate- assess to determine if pulse deficit exists Premature Ventricular Contractions Clinical significance **Ventricular irritability > Ventricular Fibrillation . May occur After lysis of coronary artery clot with thrombolytic therapy in acute MI— reperfusion dysrhythmias Following plaque reduction after percutaneous coronary intervention Treat if: >5 PVC’s a minute Runs of PVC’s Multi focal PVC’s “R on T” What is this? Ventricular Tachycardia (VT) Ventricular rate 150-250, regular or irregular No P waves QRS>.12 Can be stable- pulse or unstable –no pulse Cause- electrolyte imbalance, MI, CAD, dig Life- threatening, dec. CO, watch for V-fib Treatment- same as for PVC’s and defibrillate for sustained (if not responsive) Ventricular Tachycardia Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 66 Ventricular Tachycardia Clinical significance VT can be stable (patient has a pulse) or unstable (patient is pulseless) Sustained VT: Severe dec. in CO • Hypotension • Pulmonary edema • Decreased cerebral blood flow • Cardiopulmonary arrest Ventricular Tachycardia Clinical significance Treatment for VT must be rapid May recur if prophylactic treatment is not initiated Ventricular fibrillation may develop Polymorphic Ventricular Tachycardia- Torsades de Pointes” (“twisting around a point”) Rhythm: Rate: P Waves: PR Interval: QRS Complexes: Well…irregular…but… 100-250 bpm Usually not seen (buried in QRS if they exist) None Wide, distorted, bizarre, and “rhythmic” – getting smaller, then larger, then smaller, then… AKA: “Torsades de Pointes” (“twisting around a point”) Usually caused by hypo/hyperkalemia, HYPOMAGNESEMIA, TCA OD, and some antidysrhythmic medications. Treatment - includes treating cause(s), medications, and defibrillation or cardioversion. VT- Torsades de Pointes French for twisting of the points Ventricular Tachycardia Treatment Precipitating causes must be identified and treated (e.g., hypoxia). Monomorphic VT Hemodynamically stable (e.g., + pulse) + preserved LV function: IV procainamide, sotalol, amiodarone, or lidocaine Hemodynamically unstable or poor LV function: IV amiodarone or lidocaine followed by cardioversion Polymorphic VT with a normal baseline QT interval: adrenergic blockers, lidocaine, amiodarone, procainamide, or sotalol; cardioversion used if drug therapy is ineffective. Polymorphic VT with a prolonged baseline QT interval: IV magnesium, isoproterenol, phenytoin, lidocaine, or antitachycardia pacing; Drugs that prolong QT interval should be discontinued if rhythm is not converted, cardioversion may be needed. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 71 Ventricular Tachycardia Treatment VT without a pulse is a life-threatening situation. Cardiopulmonary resuscitation (CPR) and rapid defibrillation • Epinephrine if defibrillation is unsuccessful Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 72 Ventricular Fibrillation Garbage baseline-quivering No P’s No QRS’s No CO Cause-MI, CAD, CMP, shock, altered K+, hypoxia, acidosis, and drugs Treatment- code situation, ACLS, CPR, **defibrillate *cannot cardiovert…no rhythm to cardiovert Asystole Clinical significance Unresponsive, pulseless, and apneic state Prognosis for asystole is extremely poor. Treatment CPR with initiation of ACLS measures (e.g., intubation, transcutaneous pacing, IV therapy with epinephrine and atropine) Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 75 Pulseless Electrical Activity (PEA) Electrical activity can be observed on ECG, but no mechanical activity of ventricles is evident; patient has no pulse. Treatment CPR > intubation > IV epinephrine Atropine if ventricular rate is slow. Treatment directed toward correction of underlying cause. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 76 Sudden Cardiac Death (SCD) Death from a cardiac cause Majority of SCDs result from ventricular dysrhythmias. Ventricular tachycardia Ventricular fibrillation Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 77 Complications Dysrhythmias Hypotension Tissue ischemia Thrombi- low dose heparin, or ASA Heart failure Shock Death Diagnostic Tests •Telemetry- 5 lead (lead II and V1) •12 lead EKG •Holter or event monitoring •Exercise stress test •Electrophysiology studies- induce arrhythmias under controlled situation > Ablation to correct underlying problem . Nursing Assessment Apical rate and rhythm Apical/radial deficit Blood pressure Skin Urine output Signs of dec. cardiac output Nursing Diagnoses •Dec. cardiac output •Dec. tissue perfusion •Activity intolerance •Anxiety and Fear •Knowledge deficit Goals/Outcomes?? Interventions Medications Pacemaker (Types) Mapping Ablation Maze & modified Maze CPR Cardioversion Defibrillation Medications- review *Know your meds Classified by effect on action potential Class I- fast Na blocking agents-ventricular Quinidine, Pronestyl, Norpace,Lidocaine, Rhythmol Class II- beta blockers (esmolol, inderal) SVT, Atrial fibrillation, Atrial flutter Class III- K blocking (sotalol, amiodorone)both atrial and ventricular Class IV- Calcium channel blockers (verapamil, diltiazem(cardiazem) for SVT, Afib, atrial flutter Other- adenosine, dig, atropine, magnesium (correct electrolytes) Antiarrhythmics Remember-phrase “Some Block Potassium Channels” Class I "Some" = S = Sodium Class II "Block" = B =Beta blockers Class III "Potassium" = Potassium channel blockers Class IV "Channels" = C =Calcium channel blockers Comfort Measures Rest- dec. cardiac demands; careful monitoring!! O2 IV access; Select appropriate therapy Relieve fear and anxiety- Diazepam (valium) Defibrillation Most effective method of terminating VF and pulseless VT Passage of DC electrical shock through heart to depolarize cells of myocardium to allow SA node to resume the role of pacemaker Output is measured in joules or watts per second. Recommended energy for initial shocks in defibrillation Biphasic defibrillators: First and successive shocks: 150 to 200 joules Monophasic defibrillators: Initial shock at 360 joules Safety precautions** After initial shock, chest compressions (CPR) should be started AED’s Fig. 36-20. Paddle placement and current flow in monophasic defibrillation (A) and biphasic defibrillation (B). Fig. 36-21. LifePak contains monitor, defibrillator, & transcutaneous pacemaker. Synchronized Cardioversion Choice of therapy for hemodynamically unstable ventricular or supraventricular tachydysrhythmias Synchronized circuit delivers countershock on R wave of QRS complex of ECG. Synchronizer switch must be turned ON. Use for Ventricular Tachycardia, SVT or a- fib, flutter to convert Usually planned Get permit Start at 50 watt/sec Awake, give O2 and sedation Have to synchronize with rhythm http://www.dearnurses.net/ cardioversion To defibrillate a rhythm, it needs to be synchronized to the QRS? True or False? False! No QRS to synchronize with!! Implantable Cardioverter-Defibrillator (ICD) Appropriate for patients who have survived SCD spontaneous sustained VT syncope with inducible ventricular tachycardia/fibrillation during EPS at high risk for future life-threatening dysrhythmias Consists of lead system placed via subclavian vein to endocardium Battery-powered pulse generator is implanted subcutaneously. Equipped with antitachycardia and antibradycardia pacemakers. Initiate overdrive pacing of supraventricular and ventricular tachycardias; Provide backup pacing for bradydysrhythmias that may occur after defibrillation discharges Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 88 Implanted Cardiac Defibrillator (ICD) Senses rate and width of QRS Goes off 3 times, then have to be reset Some combined with pacemaker If fires- seek medical attention! Teaching critical! Pacemaker Used to pace heart when normal conduction pathway damaged or diseased Pacing circuit consists of a power source, one or more conducting (pacing) leads, and myocardium. Permanent- battery under skin Temporary- battery outside body Types Transvenous Epicardial- bypass surgery Transcutaneous- emergency Modes Asynchronous- at preset time without fail Synchronous or demand- when HR goes below set rate Review classifications- (Wikipedia) Pacemaker resources View Pacemaker insertion Transcutaneousemergency Temporary Transvenous Pacemaker Fig. 36-26. Temporary transvenous pacemaker catheter insertion. A single lead is positioned in the right ventricle through either the basilic or jugular vein. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 92 Pacemaker Spike Fig. 36-23. Ventricular capture (depolarization) secondary to signal (pacemaker spike) from pacemaker lead in the right ventricle. Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 93 Pacemakers Antibradycardia pacing Antitachycardia pacing: Delivery of a stimulus to the ventricle to terminate tachydysrhythmias Overdrive pacing: Pacing the atrium at rates of 200 to 500 impulses per minute to terminate atrial tachycardias Permanent pacemaker: Implanted totally within the body Cardiac resynchronization therapy (CRT): Pacing technique that resynchronizes cardiac cycle by pacing both ventricles Pacemaker Problems (next slide) Teaching critical (text table 36-11) Copyright © 2011, 2007 by Mosby, Inc., an affiliate of Elsevier Inc. 94 Pacemaker Problems: •Failure to sense •Failure to capture Radiofrequency Catheter Ablation Therapy Electrode-tipped ablation catheter “burns” accessory pathways or ectopic sites in atria, AV node, and ventricles. Nonpharmacologic treatment for AV nodal reentrant tachycardia Reentrant tachycardia related to accessory bypass tracts Control of ventricular response of certain tachydysrhythmias Done in special cardiac procedures lab Use a laser to burn abnormal pathway View video 96 EKG changes in an acute MI EKG CHANGES ASSOCIATED WITH ACUTE CORONARY SYNDROME 12-lead ECG - primary diagnostic tool used to evaluate patients presenting with ACS. Definitive ECG changes occur in response to ischemia, injury, or infarction of myocardial cells; seen in leads that face area of involvement. Typical ECG changes seen in myocardial ischemia include STsegment depression and/or T wave inversion. Typical ECG change seen during myocardial injury is STsegment elevation. ST-segment elevation and a pathologic Q wave may be seen on ECG with myocardial infarction. 3 ECG Changes Associated with Acute Coronary Syndrome (ACS)> STEMI Ischemia ST segment depression and/or T wave inversion ST segment depression- significant if at least 1 mm (one small box) below isoelectric line Injury/Infarction ST segment elevation is significant if >1 mm above isoelectric line If treatment is prompt & effective, may avoid infarction • If serum cardiac markers present, an ST-segment-elevation myocardial infarction (STEMI) has occurred Infarction/Necrosis Note: physiologic Q wave is first negative deflection following P wave Small and narrow (<0.04 second in duration) *Pathologic Q wave- deep and >0.03 second in duration ECG Changes Associated with Acute Coronary Syndrome (ACS) Typical EKG changes associated with an MI include: 1. 2. 3. 4. Long PR interval Q waves ST segment elevation T wave inversion 1. 2. 3. 4. Long PR interval Q waves (Pathological) ST segment elevation T wave inversion Syncope Brief lapse in consciousness CausesVasovagal Cardiac dysrhythmias Other- hypoglycemia, seizure, hypertrophic cardiomyopathy 1-year mortality rate as high as 30% for syncope from cardiovascular cause Casestudies Practice! Prioritization Question A client with atrial fibrillation is ambulating in the hall on the coronary step-down unit and suddenly tells you, “I feel really dizzy.” which action should you take first? A. Help the client sit down. B. Check the client’s apical pulse C. Take the client’s blood pressure D. Have the client breathe deeply Prioritization Question A client with atrial fibrillation is ambulating in the hall on the coronary step-down unit and suddenly tells you, “I feel really dizzy.” which action should you take first? A. Help the client sit down. B. Check the client’s apical pulse C. Take the client’s blood pressure D. Have the client breathe deeply Prioritization question Cardiac rhythms are being observed for clients in the CCU. Which client needs immediate intervention? A client: A. admitted with heart failure who has atrial fibrillation with a rate of 88 while at rest. B. with a newly implanted demand ventricular pacemaker, who has occasional periods of sinus rhythm, rate 90-100. C. who has just arrived on the unit with an acute MI and has sinus rhythm, rate 76, with frequent PVC’s. D. who recently started taking atenolol (Tenormin)) and has a first-degree heart block rate 58. Prioritization question Cardiac rhythms are being observed for clients in the CCU. Which client needs immediate intervention? A client: A. admitted with heart failure who has atrial fibrillation with a rate of 88 while at rest. B. with a newly implanted demand ventricular pacemaker, who has occasional periods of sinus rhythm, rate 90-100. C. who has just arrived on the unit with an acute MI and has sinus rhythm, rate 76, with frequent PVC’s. D. who recently started taking atenolol (Tenormin)) and has a first-degree heart block rate 58. Prioritization question A diagnosis of ventricular fibrillation is identified for an unresponsive 50 year old client who has just arrived in the ED. Which action should be taken first? A. Defibrillate at 200 joules B. Begin CPR C. Administer epinephrine 1 mg IV D. Intubate and manually ventilate. Prioritization questions A diagnosis of ventricular fibrillation is identified for an unresponsive 50 year old client who has just arrived in the ED. Which action should be taken first? A. Defibrillate at 200 joules B. Begin CPR C. Administer epinephrine 1 mg IV D. Intubate and manually ventilate.