Arrhythmias:
advertisement

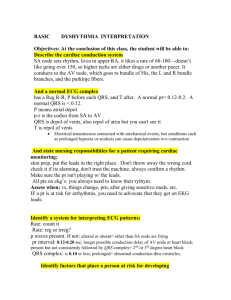
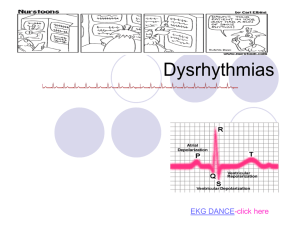
Arrhythmias: By Nancy Jenkins The EKG is the electrical activity of the heart. Electrical precedes mechanical (Without electricity, we have no pump!!) How is the electricity generated? By action potentials- Na, K and Ca very important for this Na K pump Calcium channels Depolarization Repolarization Na K pump Electrical system EKG waveforms P wave associated with atrial depolarization (stimulation) QRS complex associated with ventricular depolarization (stimulation) T wave associated with ventricular repolarization (recovery) Atrial recovery wave hidden under QRS wave Stimulus causes atria to contract before ventricles Delay in spread of stimulus to ventricles allows time for ventricles to fill and for atrial kick Conduction system SA node 60-100 AV node 40-60 Bundle of His Left and Right Bundle Branch Purkinge Fibers 15-40 How is the rate controlled? Nervous System Control of the Heart Parasympathetic nervous system:when? Vagus nerve Decreases rate Slows impulse conduction Decreases force of contraction Sympathetic nervous system: when? Increases rate Increases force of contraction Pacemakers other than SA node EKG graph paper Horizontal measures time Vertical measures voltage Helps us determine rate Width of complexes Duration of complexes Monitoring leads- based on 12 lead EKG Each lead has positive, negative and ground electrode. Each lead looks at a different area of the heart. This can be diagnostic in the case of an MI Leads to monitor in EKG leads Cardiac cells are either contractile cells influencing the pumping action or pacemaker cells influencing the electrical activity of the heart 4 Characteristics of Cardiac Cells Automaticity Excitability Conductivity Contractility Refractoriness Relative absolute Refractory Period Risk Factors for Arrhythmias Hypoxia Structural changes Electrolyte imbalances Central nervous system stimulation Medications Lifestyle behaviors Assessment Calculate rate Big block Little block Number of R waves in 6 sec times 10 Calculate rhythm-reg or irreg Measure PR interval, <.20 QRS interval .06-.10 P to QRS relationship Sinus Rhythm Normal P wave PR interval<.20 QRS.06-.10 T wave for every complex Rate is regular 60-100 Rate >100: Sinus Tachycardia Causes-anxiety, hypoxia, shock, pain, caffeine, drugs Treatment-eliminate cause Sinus Tachycardia Clinical significance Dizziness and hypotension due to decreased CO Increased myocardial oxygen consumption may lead to angina Rate<60: Sinus Bradycardia- relative-symptomatic, absolute-normal Cause-vagal stimulation, athlete, drugs (Blockers and digoxin), head injuries, MI Watch for syncope Treatment- if symptomatic, atropine or pacer Sinus Bradycardia Clinical significance Dependent on symptoms Hypotension Pale, cool skin Weakness Angina Dizziness or syncope Confusion or disorientation Shortness of breath Sinus Arrhythmia (SA) Rate 60-100 Irregular rhythm- increases with inspiration, decreases with expiration P, QRS,T wave normal Cause- children, drugs(MS04), MI Treatment- none Sinus Arrest See pauses May see ectopic beats(PAC’s PVC’s) do not treat Cause MI Treatment Atropine Isuprel Pacemaker Atrial Arrythmias Atria is the pacemaker Atrial rate contributes 25-30% of cardiac reserve Serious in patients with MI- WHY? Medications used to treat the atrial rhythms Cardizem Digoxin Amiodarone Tikosyn Verapamil Premature Atrial Contraction (PAC’s)-ectopic P wave abnormally shaped PR interval shorter QRS normal Cause-age, MI, CHF, stimulants, dig, electrolyte imbalance Treatment- remove stimulants and watch for SVT Paroxysmal Supraventricular Tachycardia (PSVT) Rate is 150-300, regular, p often hidden Atria is pacemaker (may not see p waves) Cause-SNS stimulation, MI, CHF,sepsis Treatment- vagal stimulation, * adenosine, digoxin, verapamil, inderal, cardizem,tikosyn, or cardioversion Paroxysmal Supraventricular Tachycardia (PSVT) Clinical significance Prolonged episode and HR >180 bpm may precipitate ↓ CO Palpitations Hypotension Dyspnea Angina Atrial Flutter Rate of atria is 250-300, vent rate varies Regular rhythm P waves saw tooth, ratio 2:1, 3:1, 4:1 Flutter waves- No PR interval Cause-diseased heart, dig Treatment- cardioversion, calcium channel blockers and beta blockers, amiodorone, ablation coumadin Atrial Flutter Clinical significance High ventricular rates (>100) and loss of the atrial “kick” can decrease CO and precipitate HF, angina Risk for stroke due to risk of thrombus formation in the atria Atrial Fibrillation-most common Rate of atria 350-600- (disorganized rhythm) Ventricular response irregular No P waves, “garbage baseline” Cause-#1 arrhythmia in elderly, heart disease- CAD, rheumatic, CHF, alcohol Complications- dec. CO and thrombi (stroke) Treatment- start with digoxin, ca channel blockers, beta blockers, amiodorone, pronestyl, cardioversion (TEE to see if clots before) Coumadin- check PT and INR, ablation and Maze Thrombus formation, pulse deficit, AR>RR Atrial Fibrillation Atrial Fibrillation Clinical significance Can result in decrease in CO due to ineffective atrial contractions (loss of atrial kick) and rapid ventricular response Thrombi may form in the atria as a result of blood stasis Embolus may develop and travel to the brain, causing a stroke Arrhythmias of AV Node AV Conduction Blocks First Degree AV Block Transmission through AV node delayed PR interval >.20 QRS normal and regular Cause-dig toxicity, MI, CAD vagal, and blocker drugs Treatment- none but watch for further blockage First-Degree AV Block Clinical significance Usually asymptomatic May be a precursor to higher degrees of AV block Treatment Check medications Continue to monitor Second Degree AV Block more P’s than QRS’s A. Mobitz I (Wenckebach) YouTube - Diagnosis Wenckebach PR progressively longer then drops QRS Cause- MI, drug toxicity rd Treatment- watch for type II and 3 degree B. MobitzII More P’s but skips QRS in regular pattern 2:1,3:1, 4:1(QRS usually greater than .12- BBB) Constant PR interval- can be normal or prolonged Treatment-Pacemaker Occurs in HIS bundle with bundle branch block Second-Degree AV Block, Type 1 (Mobitz I, Wenckebach) Clinical significance Usually a result of myocardial ischemia or infarction Almost always transient and well tolerated May be a warning signal of a more serious AV conduction disturbance Second-Degree AV Block, Type 2 (Mobitz II) Clinical significance Often progresses to third-degree AV block and is associated with a poor prognosis Reduced HR often results in decreased CO with subsequent hypotension and myocardial ischemia 3rd Degree AV Block Atria and ventricles beat independently Atrial rate- 60-100 Slow ventricular rate 20-40 No PR interval Wide or normal QRS (depends on where block is) Cause- severe heart disease, blockers elderly, MI Complications- dec. CO, ischemia, HF, shock, and syncope Treatment- atropine, pacemaker Third-Degree AV Heart Block (Complete Heart Block) Clinical significance Decreased CO with subsequent ischemia, HF, and shock Syncope may result from severe bradycardia or even periods of asystole (patient may present with history of fall) 3rd Degree Bundle Branch Blocks Left BBB Right BBB QRS.12 or greater Rabbit ears- RR’ No change in rhythm Junctional Rhythm AV node is pacemaker- slow rhythm (40-60) but very regular impulse goes to atria from AV node- backward) P wave patterns Absent P wave precedes QRS inverted in II, III, and AVF P wave hidden in QRS P wave follows QRS . Cont. PR interval Absent or hidden Short <.12 Negative or RP interval QRS normal No treatment Ventricular Arrythmias Most serious Easy to recognize Premature Ventricular Contractions (PVC’s)-ectopic QRS wide and bizarre No P waves T opposite deflection of PVC Cause- 90% with MI, stimulants, dig, electrolyte imbalance Treatment- O2, lidocaine, pronestyl,amiodarone No longer prophylactic Premature Ventricular Contractions Clinical significance In normal heart, usually benign In heart disease, PVCs may decrease CO and precipitate angina and HF Patient’s response to PVCs must be monitored PVCs often do not generate a sufficient ventricular contraction to result in a peripheral pulse Apical-radial pulse rate should be assessed to determine if pulse deficit exists Premature Ventricular Contractions Clinical significance Represents ventricular irritability May occur After lysis of a coronary artery clot with thrombolytic therapy in acute MI—reperfusion dysrhythmias Following plaque reduction after percutaneous coronary intervention PVC’s-unifocal Treat if: >5 PVC’s a minute Runs of PVC’s Multi focal PVC’s R on T Ventricular Tachycardia (VT) Ventricular rate 150-250, regular or irregular No P waves QRS>.12 Can be stable- pulse or unstable –no pulse Cause- electrolyte imbalance, MI, CAD, dig Life- threatening, dec. CO, watch for V-fib Treatment- same as for PVC’s and defibrillate for sustained Ventricular Tachycardia Clinical significance VT can be stable (patient has a pulse) or unstable (patient is pulseless) Sustained VT: Severe decrease in CO Hypotension Pulmonary edema Decreased cerebral blood flow Cardiopulmonary arrest Ventricular Tachycardia Clinical significance Treatment for VT must be rapid May recur if prophylactic treatment is not initiated Ventricular fibrillation may develop VT- Torsades de Pointes Ventricular Fibrillation Garbage baseline-quivering No P’s No QRS’s No CO Cause-MI, CAD, CMP, shock, K+, hypoxia, acidosis, and drugs Treatment- code situation, ACLS, CPR, **defibrillate Complications of Arrhythmias Hypotension Tissue ischemia Thrombi- low dose heparin, or ASA Heart failure Shock Death Diagnostic Tests Telemetry- 5 lead( lead II and V1) 12 lead EKG Holter monitor- pt. keeps a diary Event monitoring- pt. records only when having the event Exercise stress test Electrophysiology studies- induce arrhythmias under controlled situation Nursing Assessment Apical rate and rhythm Apical/radial deficit Blood pressure Skin Urine output Signs of decreased cardiac output Nursing Diagnoses Decreased cardiac output Decreased tissue perfusion Activity intolerance Anxiety and Fear Knowledge deficit Goals Medications Classified by effect on action potential Class I- fast Na blocking agents-ventricular Quinidine, Pronestyl, Norpace,Lidocaine, Rhythmol Class II-beta blockers (esmolol, atenolol, inderal) SVT,Afib,flutter Class III- K blocking (amiodorone, tikosyn, sotalol)both atrial and ventricular Class IV- Ca, channel blockers (verapamil cardiazem)SVT,Afib,flutter Other- adenosine, dig, atropine, covert, magnesium Comfort Measures Rest O2 Relieve fear and anxiety- valium Invasive procedures Defibrillation Emergency- start at 200 watt/sec, go to 400 Safety precautions AED’s now Synchronized Cardioversion- for vent. or SVT Can be planned- if stable Get permit Start at 50 watt/sec Awake, give O2 and sedation Have to synchronize with rhythm Implanted Cardiac Defibrillator (ICD) Senses rate and width of QRS Goes off 3 times, then have to be reset Combined with pacemaker- overdrive pacing or back up pacing Implantable Cardioverter- Defibrillator (ICD) Pacemaker Permanent- battery under skin Temporary- battery outside body Types Transvenous Epicardial- bypass surgery Transcutaneous- emergency Modes Asynchronous- at preset time without fail Synchronous or demand- when HR goes below set rate Review classifications-http://en.wikipedia.org/wiki/Artificial_pacemaker Pacemakers Ablation Done in special cardiac procedures lab Use a laser to burn abnormal pathway 3 ECG Changes Associated with Acute Coronary Syndrome (ACS) Ischemia ST segment depression and/or T wave inversion ST segment depression is significant if it is at least 1 mm (one small box) below the isoelectric line ECG Changes Associated with Acute Coronary Syndrome (ACS) Injury/Infarction ST segment elevation is significant if >1 mm above the isoelectric line If treatment is prompt and effective, may avoid infarction If serum cardiac markers are present, an ST-segment-elevation myocardial infarction (STEMI) has occurred ECG Changes Associated with Acute Coronary Syndrome (ACS) Infarction/Necrosis Note: physiologic Q wave is the first negative deflection following the P wave Small and narrow (<0.04 second in duration) Pathologic Q wave is deep and >0.03 second in duration EKG changes in an acute MI ECG Changes Associated with Acute Coronary Syndrome (ACS) ECG Changes Associated with Acute Coronary Syndrome (ACS) ECG Changes Associated with Acute Coronary Syndrome (ACS) Syncope Brief lapse in consciousness CausesVasovagal Cardiac dysrhythmias Other- hypoglycemia, seizure, hypertrophic cardiomyopathy 1-year mortality rate as high as 30% for syncope from cardiovascular cause QuizzesDiscussionQuestions Casestudies Video acting out rhythms Prioritization Question A client with atrial fibrillation is ambulating in the hall on the coronary step-down unit and suddenly tells you, “I feel really dizzy.” which action should you take first? A. Help the client sit down. B. Check the client’s apical pulse C. Take the client’s blood pressure D. Have the client breathe deeply Prioritization question Cardiac rhythms are being observed for clients in the CCU. Which client will need immediate intervention? A client: A. admitted with heart failure who has atrial fibrillation with a rate of 88 while at rest. B. with a newly implanted demand ventricular pacemaker, who has occasional periods of sinus rhythm, rate 90-100. C. who has just arrived on the unit with an acute MI and has sinus rhythm, rate 76, with frequent PVC’s. D. who recently started taking atenolol (Tenormin)) and has a first-degree heart block rate 58. Prioritization question A diagnosis of ventricular fibrillation is identified for an unresponsive 50 year old client who has just arrived in the ED. Which action should be taken first? A. Defibrillate at 200 joules B. Begin CPR C. Administer epinephrine 1 mg IV D.Intubate and manually ventilate.