Cardiovascular Summary AP and EKGs
advertisement
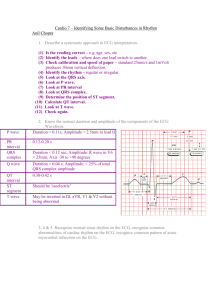
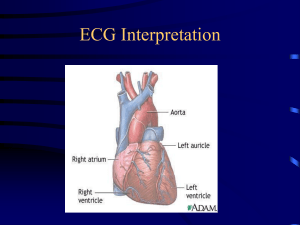
THE CARDIOVASCULAR SYSTEM THE HEART AS A PUMP WHAT MAMMAL HAS THE LARGEST HEART? WHAT MAMMAL HAS THE LARGEST HEART? The Blue Whale It’s aorta is large enough that an adult can crawl through it. It pumps approximately 15,000 pints of blood compared to 8 pints in a human being. WHICH MAMMAL HAS THE NEXT LARGEST HEART, SECOND TO THE BLUE WHALE? WHICH MAMMAL HAS THE NEXT LARGEST HEART, SECOND TO THE BLUE WHALE? WHY? HOW BIG IS THE HUMAN HEART? Adults: the size of two fists Pediatrics: the size of a fist THE HEART BEATS APROX. 100,000 TIMES A DAY In an average lifetime the heart will beat 2.5 Billion times! THE HEART PUMPS ABOUT 1 MILLION BARRELS OF BLOOD DURING AN AVERAGE LIFETIME That is enough to fill 3 supertankers A KITCHEN FAUCET WOULD NEED TO BE TURNED ON FULL BLAST FOR 45 YEARS TO EQUAL THE AMOUNT OF BLOOD PUMPED BY THE HEART IN A LIFETIME. THE HEART PUMPS BLOOD TO ALMOST ALL OF THE 75 TRILLION CELLS IN THE BODY. THE ONLY CELLS WITH NO BLOOD SUPPLY ARE THE CORNEAS. THE LUB-DUB SOUND MADE BY THE HEART IS SOUND MADE BY THE 4 VALVES WHEN THEY CLOSE. THE HEART DOES MORE WORK THAN ANY OTHER MUSCLE IN THE BODY. THE HEART BEGINS BEATING 4 WEEKS AFTER CONCEPTION. A WOMAN’S HEART BEATS FASTER THAN THAT OF A MAN’S. The average heart rate for a man is 70 while it is 78 for a woman. WHEN THE BODY IS AT REST: IT TAKES ONLY 6 SECONDS FOR THE BLOOD TO TRAVEL FROM THE HEART TO THE LUNGS AND BACK 8 SECONDS TO TRAVEL TO THE BRAIN AND BACK 16 SECONDS TO TRAVEL TO THE TOES AND BAC K THE PULMONARY ARTERIES ARE THE ONLY ARTERIES TO CARRY UNOXYGENTATED BLOOD AND THE PULMONARY VEINS ARE THE ONLY VEINS TO CARRY OXYGENATED BLOOD. VIDEOS https://www.youtube.com/watch?v=7XaftdE_ h60 https://www.youtube.com/watch?v=K57qjYYj gIY Label The Following Structures Superior Vena Cava Inferior Vena Cava Pulmonary Artery Pulmonary Vein Aorta R Atrium L Atrium R Ventricle L Ventricle Tricuspid Valve Mitral Valve Pulmonic Valve Aortic Valve Write Oxygenated Blood on the side w/Oxygenated Blood and Unoxygenated blood on the side w/Unoxigenated blood. Heart Valves Memory Tip Tricuspid Valve is on the Right side of the Heart by noting the letters R and T are close together in the alphabet. Mitral Valve is on the Left side of the Heart , so remember L and M are side by side in the alphabet. Tricuspid Valve The valve between the R atrium and R ventricle. Pulmonic Valve The valve between the r ventricle and the pulmonary arteries. Mitral Valve The valve between the L atrium and L ventricle. Aortic Valve The valve between the L ventricle and the Aorta. Stenosis of the Valve Stenosis is the term for a valve that doesn’t open properly. The flaps of a valve thicken, stiffen, or fuse together. As a result, the valve cannot fully open. Thus, the heart has to work harder to pump blood through the valve, and the body may suffer from a reduced supply of oxygen. http://www.heart.org/HEARTORG/Conditions/M ore/HeartValveProblemsandDisease/ProblemHeart-Valve-Stenosis_UCM_450369_Article.jsp Valve Regurgitation Regurgitation is the name for leaking heart valves. Sometimes the condition is minor and may not require treatment, but other times valve regurgitation places a strain on the heart. It can cause the heart to work harder to pump the same amount of blood. http://www.heart.org/HEARTORG/Conditions/M ore/HeartValveProblemsandDisease/ProblemHeart-ValveRegurgitation_UCM_450736_Article.jsp Heart Murmur The sound made by a valve that is not functioning properly. Types of Valve Replacements: Mechanical Valve Donor Valve Valve Replacement Surgery THE ELECTRICAL COMPONENT OF THE HEART Physiology of Cardiac Conduction In an adult with a healthy heart, the heart rate is usually about 72 beats per minute. The excitatory and electrical conduction system of the heart is responsible for the contraction and relaxation of the heart muscle. Sinoatrial Node (SA Node) Pacemaker of the heart This node is located along the posterior wall of the right atrium right beneath the opening of the superior vena cava. It is crescent shaped and about 3 mm wide and 1 cm long. Atrioventricular Node (AV Node) The impulse travels from the SA node through the internodal pathways to the atrioventricular node (AV node). The AV node is responsible for conduction of the impulse from the atria to the ventricles. The impulse is delayed slightly at this point to allow complete emptying of the atria before the ventricles contract. The impulse continues through the AV bundle and down the left and right bundle branches of the Purkinje fibers. The Purkinje fibers conduct the impulse to all parts of the ventricles, causing contraction (Guyton, 1982). ECG or EKG Electrocardiogram A recording of the electrical activity of the heart. An ECG is a piece of graph paper containing a record of the electrical events in the heart. EKG A 12 lead EKG shows 12 different views of the electrical activity of the heart Abnormal heart rhythms occur for several reasons. The vagal stimulation of the parasympathetic nervous system can cause a decrease in the rate at the SA node and can also decrease the excitability of the AV junction fibers. This causes a slowing of the heart rate, and in severe cases a complete blockage of the impulse through the AV junction. Sympathetic stimulation also effects cardiac rhythm and conduction. It increases the rate at the SA node and increases the rate of conduction and excitability throughout the heart. It also increases the force of myocardial contraction. Subsequently, the overall workload on the heart is increased. A small area of the heart can become more excitable than normal, which causes abnormal heart beats called ectopy. Ectopic foci are usually caused by an irritable area in the heart. This irritability can be caused by ischemia, stimulants such as nicotine and caffeine, lack of sleep or anxiety (Guyton, 1982). Parasympathetic stimulation of the heart can: A. Increase the heart rate B. Increase contractility of the heart C. Decrease the heart rate Cardiac Arrhythmias The heart usually follows a sequence of events at regular intervals. Normally the rhythm is regular and the rate is between 60-100 beats per minute. Sometimes irregular beats occur, these are called arrhythmias. Cardiac Arrhythmias Arrhythmias usually originate in the atria or AV node and aren’t a problem Those that originate in the ventricles are more dangerous and can be life threatening because they affect blood flow. Lead Placement (5 lead) Where? What color lead? Right Arm- White Left Arm- Black Chest- Brown Right lower-Green Left lower- Red Lead Placement (5 lead) Remember Smoke over Fire Clouds over Grass White on Right Lead Placement (12 Lead) Systematic Interpretation Is the rhythm regular or irregular? Regularity between an R to the next R-wave What is the ventricular rate? Rate Is there a P wave for every QRS? P:R ratio What is the measurement from the beginning of the P wave to the beginning of the QRS complex? P-R Interval What is the measurement from the beginning of the Q-wave to the end of the S-wave? QRS duration What is the interpretation of the rhythm? Interpretation Measurement of Regularity Regular or Irregular? Regular or Irregular? Regular or Irregular? Counting a 6 second strip There are a few ways to count ECGs Determine that you have a 6 second strip Count the number of R Waves Multiply by 10 You have your heart rate! Rate? Rate? Rate? How to Read an EKG Strip EKG paper is a grid where Time is measured along the horizontal axis. Each small square is 1 mm in length and represents 0.04 seconds. Each larger square is 5 mm in length and represents 0.2 seconds. How to Read an EKG Strip Voltage is measured along the vertical axis. 10 mm is equal to 1mV in voltage. How to Count Squares… A few simple guidelines: Each small square on the EKG graph is .04 seconds If the count begins or ends at the middle of a square add .02 seconds. WATCH YOUR DECIMAL POINTS! Normal EKG tracings consist of waveform components that indicate electrical events during one heart beat. These waveforms are labeled P, Q, R, S, T and U. The following descriptions are with respect to Lead II. P wave is the first deflection and is normally a positive (upward) waveform. It indicates atrial depolarization (when the atrial contraction occurs). QRS complex follows the P wave. It normally begins with a downward deflection, Q; a larger upward deflection, R; and then a downward S wave. The QRS complex represents ventricular depolarization and contraction. T wave is normally a modest upward waveform, representing ventricular repolarization. U wave indicates the recovery of the Purkinje conduction fibers. This wave component may not be observable PR Interval The measurement from the beginning of the P wave to the beginning of the R wave. How to Read an EKG Strip EKG paper is a grid where Time is measured along the horizontal axis. Each small square is 1 mm in length and represents 0.04 seconds. Each larger square is 5 mm in length and represents 0.2 seconds. How to calculate the PRN interval To measure the PR interval, count the number of small squares between the start of the p wave to the start of the QRS complex; then multiply the number of squares by 0.04 seconds. Normal PR Interval= 0.12-.20 seconds Also evaluate if PR Intervals are constant or varying across the EKG strip. If they vary, determine if the variations are a steady lengthening until the point where an expected QRS does not appear. PR Interval questions to address: ◦Does the PR-Interval fall within the norm of 0.12- 0.20 seconds? ◦Is the PR-Interval constant across the ECG tracing? YOUR TURN On the samples in your packet measure the P-R interval of the strips. Once you’ve completed those go to the following website and complete the practice quiz. http://www.practicalclinicalskills.com/ekglesson-PRInterval-Quiz.aspx?courseid=301 QRS Interval The QRS complex indicates ventricular depolarization. Depolarization triggers contraction of the ventricles. Because of the larger tissue mass, the QRS complex is larger than the P wave QRS Interval In this step, measure the QRS interval from the end of the PR interval to the end of the S wave. Use calipers, marking paper or by counting small boxes. Normally this interval is 0.06 to 0.12 seconds (1.5 to 3 boxes). QRS Questions: ◦Does the QRS interval fall within the range of 0.08-0.12 seconds? ◦Are the QRS complexes similar in appearance across the ECG tracing? Your Turn On the samples in your packet measure the P-R interval of the strips. Once you’ve completed those go to the following website and complete the practice quiz. http://www.practicalclinicalskills.com/ekglesson-QRSInterval-Quiz.aspx?courseid=301 T Wave The T wave indicates the repolarization of the ventricles. It is a slightly asymmetrical waveform that follows (after a pause), the QRS complex. Take note of T waves that have a downward (negative) deflection or of T waves with tall, pointed peaks. Sinus Rhythms The dysrhythmias in this category occur as a result of influences on the Sinoatrial (SA) node. Rhythms in this category will share similarities in a normal appearing P wave, the PR interval will measure in the “normal range” of 0.12 – 0.20 second, and the QRS typically will measure in the “normal range” of 0.06 – 0.10 second. For the most part, dysrhythmias in this category either effect the rate, rhythm regularity or both within a particular tracing. We will be discussing the following complexes and rhythms: ◦Normal Sinus Rhythm ◦Sinus Bradycardia ◦Sinus Tachycardia ◦Sinus Dysrhythmia (Arrhythmia) ◦Sinus Arrest ◦Sinus Exit Block Normal Sinus Rhythm ◦Also known as Sinus Rhythm is the only rhythm when each of the five steps of rhythm analysis are “normal”. This rhythm will be regular, in a heart rate range between 60 – 100 bpm, P waves are upright and uniform in appearance (in Lead II), a P wave for each QRS complex the PR interval will measure in the normal range of 0.12 – 0.20 second (and measure the same each time), the QRS complex morphology will be similar beatto-beat and measure between 0.06 – 0.10 second (and measure the same each time). Sinus Bradycardia Everything will be normal like in Sinus Rhythm except the rate will be less than 60 bpm. Sinus Tachycardia The only difference between Normal Sinus Rhythm and Sinus Tachycardia is the rate exceeds 100 bpm. All other steps of rhythm analysis will be “normal. ◦An additional challenge that will present as rhythm rates accelerate is that the cardiac complexes will come closer together. This can result in the P wave becoming partially or completely buried within the T wave of the previous cardiac complex. Sinus Arrhythmia Sinus Dysrhythmia closely resembles Normal Sinus Rhythm with the only distinction being the intervals from one cardiac complex to the next are changing as influenced by the patients respiratory pattern. Note the changing R to R Intervals. PAC- Premature Atrial Contraction Sinus Arrest (Pause) Sinus Arrest occurs when there is a sudden absence of electrical activity initiated by the SA node. This results in a pause in the electrical activity seen on the tracing. Remember, no electrical activity = no depolarization and contraction. A pause of six-seconds is considered a medical emergency and emergency procedures must be initiated!! Sinus Arrest (Pause) It is important to measure the duration of the pause and report this information along with the frequency of the pauses if there are more than one. ◦The pause is measured by placing your caliper tips on the last R wave just prior to the pause and the R wave immediately following the pause. Count the number of small boxes and multiply by 0.04 second. This will be reported as part of the interpretation. Atrial Flutter Atrial Flutter occurs when there is an obstruction within the atrial electrical conduction system. Due to this impediment a series of rapid depolarizations occur. These depolarizations may occur two, three, four or more times per QRS complex. The AV node functions like a “gate keeper” blocking the extra impulses until the ventricular conduction system is able to accept the impulse. The impulse that is accepted will cause the QRS complex to occur. Atrial Flutter Each flutter wave represents atrial depolarization. This will be noted next to the P wave step in rhythm analysis. There is no PR interval measurement. When the tracing is interpreted, the ratio of P waves to each QRS complex will be documented along with the rhythm i.e. Atrial Flutter 4:1 (indicates 4 “P” waves to each QRS complex). Not all Atrial Flutter will have a regular rhythm. In that case just document and report your observations. Atrial Fibrillation Not all fibrillatory waves are created equal. The “P" waves can be coarse (majority measure 3 mm or more) or can be fine (majority of waveforms measure less than 3 mm) to almost absent. Regardless always report your observations. Many times when a patient has "new onset" Atrial Fibrillation the patient will report with a heart rate of 160 bpm or more. Atrial Fibrillation When a patient experiences A-fib, the atria are not contracting as they normally would. They are just quivering. This absence of contraction of the atria can result in a loss of cardiac output anywhere from 15 - 30% due to the absence of "atrial kick". This is why the heart rate is so high. The body is trying to maintain homeostasis. It will be impossible to determine the atrial rate. You will only be able to analyze and report the ventricular rate. Atrial Fibrillation with a ventricular response in excess of 100 bpm is commonly referred to as Atrial Fibrillation with “rapid ventricular response” or "uncontrolled A-fib". A Flutter VS A Fib Ventricular Rhythms Rhythms are often named according to the origin of the electrical activity in the heart or the structure where the problem is occurring. Ventricular Rhythms are aptly named due to the area of stimulation occurs in the ventricles. Dysrhythmias in this category occur as a result of either a failure of the higher (faster) pacemakers within the heart or an abnormal locus of stimulation within the ventricles is occurring at a faster rate than the other pacemaker sites and thus takes over as the pacemaker of the heart. Remember, the fastest electricity in the heart (regardless of location) will dictate the heart rate. Ventricular Rhythms Each rhythm in this category will share unique morphologic features which separate them from other rhythms. Other than Asystole and Ventricular Fibrillation which are unique even within this category, the remaining ventricular rhythms typically present without P waves and will display a wide, bizarre QRS complex (measuring 0.12 seconds or greater). After learning the unique features just described, it is simply a matter of recalling the heart rate range associated with the dysrhythmia. Important Terminology Unifocal – abnormal complexes are of the same shape Multifocal – abnormal complexes are of two or more different shapes. This indicates the impulse causing the PVC’s are coming from different locations. Important Terminology Bigeminy – abnormal complexes occur every second complex Trigeminy– abnormal complexes occur every third complex Important Terminology Couplet – Two PVC’s together Run of Ventricular Tachycardia (V Tach) – Three or more PVC’s in a row at a rate of 100 bpm or greater. Also known as Triplet PVC’s or Salvo PVC’s Premature Ventricular Contraction (PVC) PVC’s may occur for a number of different reasons i.e., diet, fatigue, stress, disease, ischemia to name a few. PVC’s occur when an early electrical impulse occurs from a location in either ventricle The locus of stimulation being different, results in a change in the morphology of the cardiac complex. Note the absence of P wave and the wide, bizarre QRS complex. PVC’s can occur occasionally or frequently. PVC’s can be observed with or without a pattern PVC Agonal Rhythm This is a life-threatening dysrhythmia. Agonal rhythm is often the last ordered semblance of organized electrical activity in the heart prior to death. Heart rate is less than 20 bpm, without P waves and a wide, bizarre QRS complex. The rate is often so slow, that on a singular six-second rhythm strip it will be impossible to determine whether the rhythm is regular or irregular. There must be at lest three complexes on the tracing to make this call. Many times there will only be one or two complexes captured on the tracing. This is a MEDICAL EMERGENCY Ventricular Tachycardia The morphologic features continue with the dysrhythmia. No P wave, wide and bizarre QRS. Ventricular Tachycardia occurs when the rate exceeds 100 bpm. This rhythm must always be reported whether the patient appears stable or not. Depending upon their level of consciousness and blood pressure. The patient may be treated with medications, synchronized cardioversion or in the worst case scenario a defibrillator and BLS/ACLS response. Ventricular Fibrillation The morphologic features are different with this dysrhythmia. No P wave and no QRS complexes. This rhythm presents with a chaotic waveform which reflects the electrical chaos occurring within the heart. The heart is not actually beating as we know it. The chaos occurs as a result of small regions of tissue which are independently depolarizing. Ventricular Fibrillation Fibrillatory waves may be coarse or very fine. This is based upon their size. The longer V Fib occurs, the smaller the waveforms are likely to be. Coarse V Fib is when a majority of the waveforms measure 3 mm or greater Fine V Fib is when a majority of the waveforms measure less than 3 mm This is absolutely a life-threatening dysrhythmia which requires, immediate, effective, and aggressive care. If your patient is talking to you when you see this on the monitor, then your patient is not in V Fib. Always, check your patient first, but there will likely be a loose or disconnected lead wire or electrode. Ventricular Fibrillation Asystole This dysrhythmia occurs when there is a total absence of electrical activity in the heart. The patient is clinically dead. Sometimes this tracing is referred to as straight line or flat line. There will be an absence of P waves and QRS complexes. True Asystole is an absolute medical emergency! If your patient is speaking to you, they are NOT in Asystole. Check your attachments and equipment. Asystole Pulseless Electrical Activity PEA In PEA the heart muscle looses its ability to contract even though electrical activity is present. On an ECG you will see evidence of organized electrical activity but you won’t be able to palpate a pulse or measure the blood pressure. Treat as Asystole! Heart Blocks In people with heart block the electrical pulses that control the heart rate are disrupted, causing the heart to beat more slowly. It's a type of arrhythmia, which is a medical term used to describe problems with the rate or rhythm of the heartbeat. There are three levels of heart block, and usually only the most serious type causes symptoms Types of heart block There are three main types of heart block: • first-degree heart block • second-degree heart block • third-degree heart block First Degree Block In first-degree heart block, there's a split-second delay in the time it takes electrical pulses to move through the AV node. First-degree heart block rarely causes any noticeable symptoms. Will look like Sinus Rhythm with one exception: The P-R interval will be constant throughout the tracing and measure greater than 0.20 seconds Second Degree Heart Block In second-degree heart block there's a series of increasing delays in the time it takes the AV node to send the pulse to the ventricle. This will eventually lead to a heartbeat being skipped. There are two sub-types of second-degree heart block. Second Degree Type I Wenckebach This is the less serious type. It occasionally causes mild dizziness and doesn't usually require treatment. The unique feature (hallmark) of this dysrhythmia is the presence of a prolonging P-R interval from one cardiac complex to the next, until it reaches a point where the QRS complex is non-conducted ( blocked or more simply missing). Then the pattern starts over again. Second Degree Type I Wenckebach P-R Interval gets wider and wider and then drops the QRS. https://www.youtube.com/watch?feature=player_embedded&v=hO_ny2_ 2N8o Second Degree Type II Mobitz Type II • The hallmark of this dysrhythmia is a constant P-R interval with missing QRS complexes. • This dysrhythmia may present in a couple of different ways. • A. QRS complexes occurring in a specific pattern in a ratio with the P waves. This is often referred to as 2:1 or 3:1 block depending upon the ratio of P waves to each QRS complex. • B. QRS complexes occur in a more unstable, unpredictable manner. Second Degree Type II Mobitz Type II Either presentation requires immediate reporting due to its potential for conversion to Third Degree (Complete) Heart Block. Third Degree Heart Block Complete Heart Block In third-degree or complete heart block there's no transmission of electrical pulses between the atria and the ventricles through the AV node. • The outcome of this impediment are two independently functioning pacemakers within the heart (typically one is supraventricular, the other is ventricular). • Essentially, the atria and ventricles are electrically separated (dissociated) from one another. What will be seen are regularly occurring P waves and QRS complexes, but at two distinctly different rates. Complete heart block presents with Regular P to P and R to R intervals and a variable P-R interval. What is this Rhythm? What is this Rhythm? What is this Rhythm? ST Elevation STEMI STEMI Medical Emergency!! Pt NEEDS the CATH LAB STAT.