Cardio82-12LeadECG
advertisement
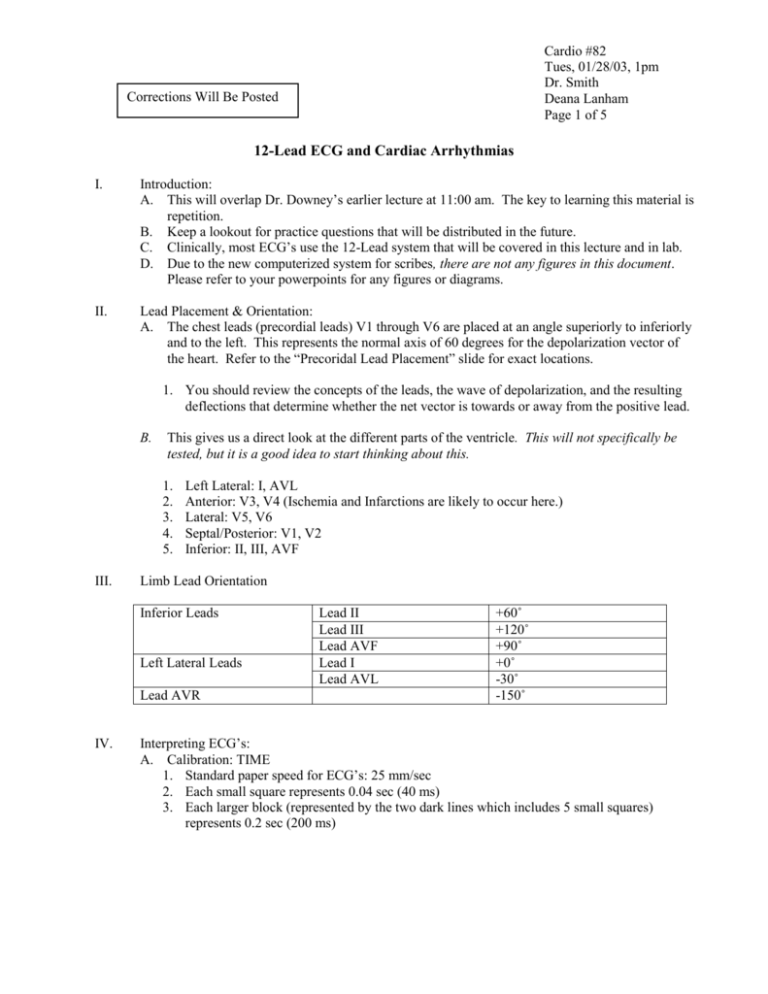
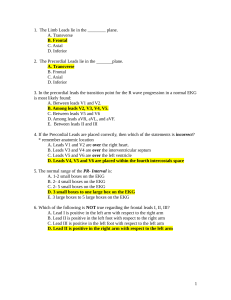
Cardio #82 Tues, 01/28/03, 1pm Dr. Smith Deana Lanham Page 1 of 5 Corrections Will Be Posted 12-Lead ECG and Cardiac Arrhythmias I. Introduction: A. This will overlap Dr. Downey’s earlier lecture at 11:00 am. The key to learning this material is repetition. B. Keep a lookout for practice questions that will be distributed in the future. C. Clinically, most ECG’s use the 12-Lead system that will be covered in this lecture and in lab. D. Due to the new computerized system for scribes, there are not any figures in this document. Please refer to your powerpoints for any figures or diagrams. II. Lead Placement & Orientation: A. The chest leads (precordial leads) V1 through V6 are placed at an angle superiorly to inferiorly and to the left. This represents the normal axis of 60 degrees for the depolarization vector of the heart. Refer to the “Precoridal Lead Placement” slide for exact locations. 1. You should review the concepts of the leads, the wave of depolarization, and the resulting deflections that determine whether the net vector is towards or away from the positive lead. B. This gives us a direct look at the different parts of the ventricle. This will not specifically be tested, but it is a good idea to start thinking about this. 1. 2. 3. 4. 5. III. Left Lateral: I, AVL Anterior: V3, V4 (Ischemia and Infarctions are likely to occur here.) Lateral: V5, V6 Septal/Posterior: V1, V2 Inferior: II, III, AVF Limb Lead Orientation Inferior Leads Left Lateral Leads Lead AVR IV. Lead II Lead III Lead AVF Lead I Lead AVL +60˚ +120˚ +90˚ +0˚ -30˚ -150˚ Interpreting ECG’s: A. Calibration: TIME 1. Standard paper speed for ECG’s: 25 mm/sec 2. Each small square represents 0.04 sec (40 ms) 3. Each larger block (represented by the two dark lines which includes 5 small squares) represents 0.2 sec (200 ms) Cardio #82 Tues, 01/28/03, 1pm Dr. Smith Deana Lanham Page 2 of 5 B. Calibration: VOLTAGE 1. Standard: 10 mm/mV 2. 2 big blocks represent 1 mV. C. Calculating the RATE 1. Normally when calculating the rate, you would calculate the R-R interval (ventricular rate). You can also calculate the P-P interval (atrial rate). In “normal” circumstances or normal sinus rhythm the R-R and P-P interval should be equal. In normal sinus rhythm, the depolarization originates in the SA node and normal rate and rhythm exist. The primary arrhythmia where the R-R and P-P intervals are not the same and completely dissociated is during a third degree complete AV Block. Use Dr. Downey’s syllabus notes to calculate the R-R and P-P intervals to practice determining the atrial and ventricular rates. 2. Quick Calculations Use the ECG located on the “RATE” slide. Calculate (300 / # of big lines) to determine the rate. Units: bpm For example: For three big lines calculate 300/3= 100 bpm. A sinus-conducted rate (“normal” figure) is around 200 bpm. 300 bpm and above is abnormal. If you had a heart beat every second, you would have a heart rate of 60 bpm (5 big blocks). The heart rate in this ECG is most likely a little slower than 75 bpm. 3. More Accurate Calculations Rate = 60/(ratio of R-R interval in small boxes to 25) Specifically, Rate = 60/ (x/25) For example, if your R-R interval is 20 small boxes then your calculation would be: o 60/ (20/25) = 75 bpm. This is equivalent to four big blocks. If your R-R interval is 18 small boxes your calculation would be: o 60/ (18/25) = 83.3 bpm. The ratio x/25 defines your cardiac cycle length or the number of seconds between each beat. Multiply by 100 to get ms. The cardiac cycle length is inversely related to the heart rate. Ideally, you should take more than one R-R interval measurement because your heart rate fluctuates with your respiration. This is termed respiratory sinus arrhythmia. The rate might be misrepresented if only a single R-R interval was chosen for calculations. 4. Key Points for Rate Quick Access: Brady = <60bpm (>5 blocks) Tachy = >100 bpm (< 3 blocks) Ask yourself if the atrial and ventricular rates are equal. Ideally they should be. Also ask if there is a sinus or ectopic pacemaker. An ectopic pacemaker should change the shape of the P wave and the activation of the atria only. Cardio #82 Tues, 01/28/03, 1pm Dr. Smith Deana Lanham Page 3 of 5 The QRS would be normal. The P wave would be buried in the QRS complex, but the artia would still contract. To determine if the heart rate is in normal sinus rhythm look for the P wave and the appropriate P-R interval. D. Rhythms 1. Define the rhythm by where it originates, (atrial or ventricular?) and by its pattern (tachycardia or bradycardia?). 2. DISREGARD the “normal rhythm” definition. Rhythms can vary (as in respiratory sinus arrhythmia) and still be considered normal. 3. Abnormal Rhythms (Arrhythmias) Sinus Arrhythmia: o Normal respiratory sinus arrhythmia o Respirations cause variation in vagal activity. When parasympathetic activity increases, the diastolic membrane potential of the SA node gets more negative. Wandering Pacemaker o If different cells end up being faster to depolarize or reach threshold, they will end up being the pacemakers. o If there is no SA node (in sick sinus syndrome for example) other cells will take over, and the AV site is an important site where this occurs. Atrial Fibrillation o Rapid rhythm where a multiple number of sites are provoking the atrium. Consequently, the atrium is not effective as a pump. 5. Extra/Ectopic Beats (e.g. PVC) Premature Atrial Contractions (PAC): o Spontaneous depolarizations o Just having a few will not affect your heart rate. Premature Ventricular Contractions (PVC): o Could be due to an ectopic beat in an abnormal location. o Also referred to as PVB in other books. The B stands for beat. Escape Beats (Ventricular Escape): o This is where you have a strong enough vagal activation to where the SA node does not fire for up to about 8 seconds, but the ventricles occasionally beat on their own. 6. Rapid Rhythms Sinus Tachycardia: increased rate originating in the SA node Atrial Tachycardia: increased rate originating outside of the SA node. Ventricular Tachycardia: o Increased rate originating in the ventricles. o A classic cause for this would be reentry Cardio #82 Tues, 01/28/03, 1pm Dr. Smith Deana Lanham Page 4 of 5 o Monomorphic: less threatening; only has one pattern o Polymorphic: more than one pattern; can lead to ventricular fibrillation Atrial Flutter: volume & rhythm of pulse are irregular. Atrial Fibrillation Ventricular Fibrillation: o Life Threatening; will lead to a loss of consciousness within a few seconds o Irregular continuous and uncoordinated twitchings of the ventricular muscle fibers. It is ineffective as a pump. o Feels like “a bag of quivering worms.” 7. Heart Blocks (e.g. AV Block) AV Nodal Block: 1st degree, 2nd degree, and complete AV Block Bundle Branch Block: o Refers to the right and left bundles; conduction occurs after the AV node. o A right block is less serious than a left block. o QRS will get longer and may have a double hump. V. Typical Print Out of a 12-Lead (Refer to Slide #9) A. Depicts lead I, II, III, and shows a series of 9 heartbeats. B. The bottom strip is a rhythm strip that is set at lead II. C. The configuration in the machine switched to the augmented leads during the third beat (represented by AVR, AVL, AVF). D. The last two periods show the chest leads V1 through V6. E. Note: When the machine makes the switch to augmented leads, it shows an electrical artifact that does not represent an abnormal finding (i.e. It does not represent arrhythmia or any kind of heart beats.) F. When using the machine, do your own diagnosis to confirm the computer diagnosis. Do NOT only rely on the computer program. VI. Axis Determination A. Rapid Approach: 1. Lead I: if positive, vector is towards the left 2. AVF: If positive, vector is downward 3. Axis can also be determined for P & T. B. Abberant Axes (Deviations): 1. QRS positive in I and AVF, vector = 0-90˚ 2. Left Axis Deviation: More negative than -30˚ 3. 1st look: QRS negative in AVF & III, positive in I. 4. Right Axis Deviation: Vector more than or equal to 110˚ 5. 1st look: QRS negative in I 6. Extreme Right Axis Deviation: QRS is negative, both in I & AVF 7. REMEMBER: You can calculate the vector from any limb leads. PRACTICE THIS! The rest of the slides were not discussed in class, but most of the information will be included here. The end of the powerpoints illustrates different ECG’s for abnormal findings that will not be included in this scribe because of the numerous figures. Cardio #82 Tues, 01/28/03, 1pm Dr. Smith Deana Lanham Page 5 of 5 VII. Intervals & Segments A. Normal PR Interval: 0.12-0.20 seconds 1. Decreases as heart rate increases 2. > 0.2 indicates heart block 3. <0.12 (during sinus rhythm) is an indication of pre-excitation syndrome (e.g. WPW) B. C. Normal QRS Interval: < 0.10 seconds 1. Decreases as heart rate increases 2. > or = “wide” QRS is a possible indication of conduction delay through ventricles or conduction asynchrony within ventricles. 3. e.g. right or left bundle branch blocks, ischemia, heart failure QT Interval D. ST Segment 1. Segment depression & elevation can be indicator of ischemia or infarction or conduction abnormally in the ventricles. E. VIII. T Wave 1. Size 2. Direction 3. Duration ECG & Clinical Diagnosis A. What is the interpretation of ECG? B. C. Clinical diagnosis relates ECG to other signs, symptoms, and tests. All of these direct treatment decisions. Drugs 1. Rate, rhythm, decrease cardiac work, protect against adverse stimuli (e.g. SNA) 2. RFA (radio frequency ablation): target and treat abnormal conduction pathways 3. Pacemaker: target and treat inadequate rates 4. ICD (Internal Cardiac Defibrillator): target and treat potentially fatal arrhythmias D. Mechanisms for some types of arrhythmias: 1. Ectopic Foci 2. Accessory Pathway (reentrant tachycardia, Lown-Gangong-Levine) 3. Bundle Branch Block 4. Predict Effects on: PR interval, QRS duration, conduction velocity, ST segment, P wave, QRS morphology