File
advertisement

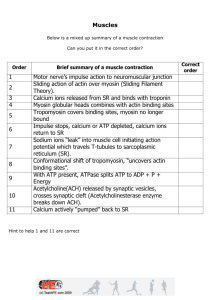
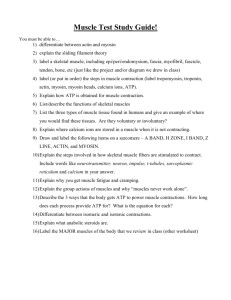
Muscles I. Types of muscles A. Skeletal muscle 1. Attached to bones 2. Striated 3. Somatic neuron innervation = cxn 4. Function: a. Body movement b. Posture maintenance c. Joints stability B. Cardiac muscle (the heart) 1. Pumps blood 2. Striated 3. Autorhythmicity C. Smooth muscle 1. On internal organ walls and blood vessels 2. Non-striated 3. Autorhythmicity 4. Function: a. Moves materials within body b. Move materials into and out of the body II. Characteristics of muscles ( The “CEEE”) A. Contractility = Generate force in response to AP Excitation-contraction coupling B. Excitability = response to a stimulus C. Extensibility = ability to stretch w/o damage D. Elasticity = ability to return to normal after stretching III. Structure of Skeletal muscle A. Epimysiummuscleperimysiumfascicleendomysiumsarcolemma--> myofibermyofibrilmyofilaments B. Muscle cell = muscle fiber 1. Sarcolemma 2. Sarcoplasm 3. Myofibrils (80% of fiber) 4. Multi-nuclei 5. Sarcoplasmic reticulum (stores Ca2+) 6. Myoglobin a. Red pigmentation b. Contains iron (Fe2+) binding to O2, act as O2 reservoir C. Myofibrils 1. Striated = D (a) rk “A” bands and L (i) ght “I” bands 2. Sarcomere = from Z disc to Z disc a. Consist of… b. “thick” filaments = myosin 1) ~300 myosin molecules/thick filament 2) Composed of a head and a tail 3) Myosin head has 2 binding sites Contractile proteins a) One for ATP b) One for Actin c. “thin” filaments 1) Actin 2) Troponin a) Attached + moves tropomyosin Regulatory proteins b) Has Ca2+ binding site 3) Tropomyosin a) Covering myosin binding site on actin D. Sarcomere 1. Structure a. ZI-MHA-ZI= sarcomere 1) “M” line = Proteins that anchor think filaments 2) “H” zone = “Heavy only” length shortens during cxn 3) “A” band = Length remains constant during cxn 4) “Z” disk = Made of proteins that anchor thin filaments 5) “I” band = length shortens/disappears in cxn E. Sarcoplasmic reticulum (SR) 1. Inside sarcolemma, wrapped around myofibrils 2. Triad a. T – tubules = channel of sarcolemma around myofibrils 1) Function: Transmit AP to every SR of every sarcomere b. Terminal cisternae = Part of SR IV. Contraction of skeletal muscle fiber (excitation-contraction coupling A. Creating action potential (Excitation) 1. Myelinated neurons attach to muscle fiber via neuromuscular junction 2. Influx of Ca2+ to neuron causes out-flux of Ach from the terminal 3. Ach binds to nicotinic receptors on sarcolemma 4. Sodium ion channels open, letting sodium ions in 5. Creates an AP that is transmitted through T-tubules B. Influx of Ca2+ from sarcoplasmic reticulum to sarcoplasm 1. Ca2+ bathe sarcomere and attaches to troponin 2. Troponin moves tropomyosin away from myosin binding site on actin C. Sliding filament mechanism (Contraction) 1. (High Energy)Myosin head raise up to attach to actin (cross bridge formation) 2. (Low Energy)And does “power stroke” in the process 3. (ATP binds) detach myosin from actin 4. ATP hydrolysis keeps the myosin head “cocking” or facing up = ADP and inorganic phosphate 5. Myosin head pull thin filaments toward “M” line through repeated power stokes 6. Cxn of sarcomere, muscle fiber, and eventually the muscle D. Relaxation 1. Ca2+ actively pumped back into SR 2. Lowering Ca2+ covers actin from myosin 3. Relaxation occurs V. A twitch A. Motor unit = one somatic motor neuron and all skeletal muscle fibers it stimulates (~150 muscle fibers) B. Twitch = stimulation of a weak contraction by one motor unit to a single AP C. More precise movement = Many smaller motor units D. Periods of muscle twitch = latent contraction relaxation VI. Rigor mortis A. Cell death B. Membrane breaks down and leaks Ca2+ C. Causing crossbridge formation D. Cannot relax because ATP is needed E. ATP only exist in live cells VII. Muscle Tension A. Muscle tension: force created by contracting muscle on an object “the push or pull” B. Variety of muscle movement is due to… 1. Wave summation (increased frequency of contraction by each fiber) a. Increase firing rate of neuron b. Increase Ca2+ release c. Increase frequency of contraction d. Increase in force e. Unfused tetanus: sustained contraction with partial relaxation f. Fused tetanus: sustained contraction with no relaxation 2. Recruitment (increasing # of motor unit involved in cxn) C. Asynchronous recruitment: motor unit alternate between cxn and relaxation 1. Importance = allows sustained muscle cxn a. Prevents fatigue b. Maintain posture c. Maintain muscle tone (with constant stimulation) D. More space for actin-myosin overlap = more tension can be produced E. Overview: 1. Increase Contractile Force = a. Increase # of involved motor unitIncrease # of activated muscle fibers b. Increase size of muscle (more actin and myosin) c. Increase firing rate of neuron Increase frequency of stimulation d. Increased sarcomere stretch VIII. Muscle Metabolism A. Catabolic reaction: break down of molecules (ATP ADP + P + energy) B. Anabolic reaction: formation of molecules (ADP + P + energyATP) C. ATP synthesis 1. ADP + P + energy 2. Energy gained from catabolism of food molecules D. ATP is important in cxn 1. Detachment of myosin from actin 2. Re-energizing myosin head 3. Actively pumping Ca2+ back to SR for relaxation E. Nutrients 1. Free fatty acid (lipids) and glucose 2. Getting nutrients a. Catabolism of glycogen (in liver and skeletal muscle) into glucose then released into blood b. Catabolism of triglycerides (in adipose tissue) into glycerol + FFA then released into blood c. Glucose and FFA pools in blood and transported to skeletal muscle d. F. ATP synthesis w/o nutrients 1. Creatine phosphate pathway (lasts only 15 seconds) a. Creatine phosphate Give P to ADP (creatine-kinase) and becomes creatine ATP!!! b. Good for short burst of energy G. ATP synthesis w/ nutrients 1. Anaerobic pathway (lactic acid fermentation) a. Occurs lacking sufficient O2 b. Occur in cytoplasm (sarcoplasm) c. Makes 2 ATP per glucose d. Steps 1) Glycolysis: glucose pyruvate 2) Pyruvate lactic acid e. Enough energy for 30 – 40 seconds of cxn f. Advantages: IT’S QUICK! g. Limitation 1) Low ATP production vs. aerobic respiration 2) Build up lactic acid (not always bad) = acidosis a) Inhibits enzymes in glycolysis b) Decrease ATP synthesis c) Muscle soreness 2. Aerobic cellular respiration a. Steps: Occurs in mitochondria 1) (Glucose Glycolysis –> pyruvic acid) or fatty acid Krebs cycle oxidative phosphorylation 2) Generate 32 – 36 ATP per glucose 3) Generate ~100 ATP per free fatty acid 4) 90% - 95% of ATP used during rest and aerobic (endurance exercise) comes from aerobic respiration H. Short duration exercise 1. 6 sec = Stored ATP used up 2. 10 sec = ATP formed from creatine phosphate 3. 30 – 40 sec = Glycogen in muscle break down glucose oxidase ATP I. Long duration exercise 1. Hours = aerobic respiration from break down of FFA and glucose, and uses oxygen from blood J. Muscle Fatigue: muscle’s inability to cxn and respond to stimulus 1. Different from “central fatigue” = CNS signal tiredness 2. Possible causes a. Decrease Ca2+ release from SR b. Lactic acid accumulation c. Glycogen depletion K. Main muscle characteristics 1. Speed of cxn: a. Slow fibers (slow twitch = slow movement of myosin head) b. Fast fibers (fast twitch) 2. Pathway of ATP formation a. Oxidative fibers = aerobic respiration b. Glycolytic fibers = anaerobic glycolysis L. Type of muscle fibers 1. Slow oxidative fibers a. Speed of contraction = slow b. Rate of fatigue = slow c. Activity type = endurance d. Mitochondria = many e. ATP formation = aerobic f. Myoglobin content = high g. Color = red 2. Fast glycolytic fibers a. Speed of contraction = fast b. Rate of fatigue = fast c. Activity type = short and powerful d. Mitochondria = few e. ATP formation = anaerobic glycolysis f. Myoglobin content = low g. Color = white 3. Fast glycolytic-oxidative M. Effects of exercise on skeletal muscle 1. Endurance exercise: fast glycolytic fast oxidative 2. Weight training: increase size of fast glycolytic fibers (hypertrophy) a. Increase actin and myosin 3. Atrophy = loss of muscle mass a. Healthy motor unit can reverse atrophy Blood I. Blood: Liquid connective tissue transported by blood vessels A. Males: 5 – 6 L Females: 4 – 5 L B. Elements:99% Erythrocytes (RBC) and leukocytes (WBC) and platelets 1. RBC a. function 1) Transport gases, nutrients, hormones, and waste 2) Helps regulates pH 3) Protection a) clotting prevents blood loss b) Leukocytes fight infections b. Hematocrit = % of whole blood 1) Males: 42-52% 2) Females: 37-47% c. Structure 1) Thin, biconcaved disk, no nucleus and organelles 2) Hemoglobin a) 4 proteins arranged together into molecule b) Four heme: has iron that binds O2; give red color c) Each molecule bind to four O2 d. Transporting respiratory gases 1) Oxyhemoglobin = Hb bound to O2; bright red 2) Deoxyhemoglobin = Hb not bound to O2; dark, purplish red 2. WBC types and function a. Neutrophils = phagocytosis (engulfing) of unwanted substances b. Eosinophil = Release of destructive enzymes to kill parasites c. Basophil = Promote blood flow to tissues d. Lymphocytes = In the form of natural killer cells, they immediately release antibody that kills foreign substances in the body e. Monocytes = Phagocytosis of unwanted substances C. Liquid: Plasma 1. ~55% - 58% blood 2. Water, proteins, dissolved organics, ions, vitamins, and dissolved gases 3. Plasma proteins (produced by liver) a. Albumin ~54% of plasma proteins b. Transport steroid hormones and fatty acid in blood c. Keep blood circulating d. Create osmotic pressure of plasma (prevent fluid loss in capillary beds) 1) A.K.A. colloid osmotic pressure or oncotic pressure 2) Edema: swelling due to accumulation of fluid in the interstitial compartment e. Not too important proteins 1) Globulins 2) Clotting proteins D. Fibers: Dissolved fibers become insoluble in clotting process II. Hematopoiesis = synthesis of blood cell A. Occurs in… 1. Adults: in red bone marrow 2. Fetal development: liver, spleen, thymus, lymph nodes B. Develops from… 1. Stem cell: cell that has potential to develop to different cell types (pluripotent). C. Erythropoiesis: erythrocyte synthesis 1. Low oxygen in blood kidney and liver secrete erythropoietin hormone release erythrocytes production by bone marrow 2. Hypoxia = low oxygen availability to tissues 3. RBC can live ~120 4. Broken down in spleen, liver, and bone marrow a. A byproduct is bilirubin (yellowish pigment) 1) Become part of bile 2) Bile is secreted into small intestine during digestion 3) Byproduct of bilirubin a) Stercobilin (brown pigment in stinky poop) b) Urobilin (yellow pigment in urine) 4) Jaundice: yellowing of tissues due to bilirubin accumulation D. Anemia: blood has a low O2-carrying capacity 1. Causes a. Hemorrphage b. Iron deficiency c. Vitamin B12 deficiency d. Abnormal hemoglobin (e.g. sickle cell anemia) The Heart and Blood Vessel I. II. III. IV. V. Surrounding the Heart A. Pericardium: Membrane surrounding heart 1. Prevents overstretching 2. Protection 3. Anchor heart in position B. Myocardium: cardiac muscle around heart 1. One heartbeat = 1 cxn and 1 relaxation Heart Champers A. Right atrium: pump deoxygenated blood to right ventricle B. Right Ventricle: pump blood out of heart to lungs C. Left atrium: pump oxygenated blood to left ventricle D. Left ventricle: pump blood out of heart to body Heart arteries (leaving heart) A. Aorta (largest artery): branch off left ventricle (To body) B. Pulmonary trunk: Branch off right ventricle (To lungs) Heart valves (one-way!) A. Atrioventricular valve: between atrium and ventricle 1. Tricuspid valve: between right atria and ventricle (three parts – 2 lungs and heart) 2. Bicuspid (mitral) valve: between (two parts – heart and body) B. Semilunar valves: between ventricles and major arteries (UU shape looks like moons) 1. Pulmonary valve: Before pulmonary trunk 2. Aortic valve: Before the aorta Blood movement A. Right side of the heart 1. Vena cavae R atrium tricuspid valve R ventricle Pulmonary valve Pulmonary trunk Lungs B. Lift side of the heart 1. Pulmonary veins L atrium bicuspid valve L ventricle aortic valve Aorta Body VI. Vessels = arteries arterioles capillaries venules + veins A. Artery = Away from the heart, lots of smooth muscles, stiff and springy B. Arteriole = only vessel affected by sympathetic and parasympathetic stimulation 1. Constricts and dilate 2. Have Cholinergic and adrenergic receptors 3. Systemic and coronary circuits = carry oxygenated blood 4. Pulmonary circuit = carry deoxygenated blood C. Capillaries = no smooth muscle, one cell thick 1. Defuses gases, nutrients, and waste a. Deliver: O2 and nutrients to cells b. Receive: CO2 and waste from cells 2. Pressures a. Oncotic pressure: caused by proteins in plasma, retains fluids in leaky capillaries b. Hydrostatic pressure: fluid pressure on capillary wall, pushes fluid and nutrients out D. Vein = back to the heart 1. Carry 65% of total blood supply 2. Some have valves to prevent backflow 3. Systemic and coronary circuits = carry deoxygenated blood 4. Pulmonary circuit: veins carry oxygenated blood 5. Venule = small veins VII. Heart circulation/circuits A. Systemic and pulmonary circulations 1. Systemic circuit: blood to body tissues, except lungs 2. Pulmonary circuit: Blood to alveoli of lungs oxygenate blood 3. Use capillaries for gas exchange B. Coronary circuit: Blood to myocardium, gives O2 to heart muscle for ATP synthesis cxn 1. Vessels in myocardium 2. Supplies blood (oxygen) The Cardiac Cycle I. The “Lup Dup” cycle A. “Lup” 1. Vena cava flow blood to atria in diastole state 2. As hydrostatic pressure in atria becomes > ventricle 3. Blood flow to ventricle in diastole state 4. Atrial systole to squeeze last amount of blood into ventricle 5. As hydrostatic pressure in ventricle becomes > atria 6. Atrioventricular valve snap shut as blood tries to enter atria “Lup” a. End-diastolic volume (EDV) of ventricle = ~120 ml 7. Pressure in ventricle causes tricuspid and bicuspid (semilunar) valves to open 8. Blood flow to aorta and pulmonary artery 9. Ventricular systole to squeeze last amount of blood into artery a. Isovolumetric cxn = ventricle blood constant, but systole to increase pressure 10. As hydrostatic pressure in artery becomes > ventricle 11. Semilunar valves snap shut “Dup” a. End-systolic volume (ESV) of ventricle = ~ 50 – 70 ml B. Beat = one complete cardiac cycle C. Stoke volume (SV) = amount of blood pumped out per ventricle per beat II. Myocardium function A. Types of musclefibers (cells) 1. Autorhythmic fibers a. Pace makers b. Conduction system sponstaneously conducts action potential w/o NS 1) Sinoatrial (SA) node generates impulse “P” a) Generates 90-100 beats/min b) Parasympathetic NS give tonic activity: slows to 70-80 beat/min 2) Goes through internodal pathway 3) Pauses at atroventricular (AV) node a) Important for atria-first, ventricle-second sequence 4) Splits at atrioventricular (AV) bundle 5) Goes through bundle branches and conduct impulse at inter-ventricular septum 6) Travel to Purkinje fibers and depolarize contractile fibers in both ventricle c. P-QRS-T Electrocardiogram (ECG: 1) P = Atrial depolarization Electrical recording of 2) Pause = at atriaventricular node myocardium during heart 3) QRS = Ventricular depolarization activity. 4) Pause = depolarization complete 5) T = Begins repolarization 6) Pause = repolarization complete d. Makes the heart autorhythmic (beat without nervous system) e. 1% of fibers f. Do not contract 2. Contractile fibers a. 99% of fibers b. Fire AP via autorhythmic fibers and cxn c. Accept Ca2+ by both SR and extracellular fluid (different from skeletal muscles) d. Cxn by crossbridge of myosin and actin B. Intercalated disks 1. Exist between fibers 2. Have gap junctions (holes) that allow ions to flow fiber to fiber 3. Essential for quick depolarization Regulation of the Heart I. Autonomic NS regulation of heart A. Controlled by cardiac center made of neurons in the medulla oblongata B. Parasympathetic: decreases heart rate C. Sympathetic: increases heart rate and contractility II. Heart conditions A. Normal heart rate: 60 – 100 beats/min (can change and still be healthy) B. Bradycardia: HR < 60 beats/min 1. Conductoin problems 2. Athlete at rest 3. Drugs mimic parasympathetic C. Tachycadia: HR > 100 beats/min 1. Exercise 2. Sympathetic stimulation 3. Drugs mimic sympathetic D. Fibrillation 1. Random and uncoordinated cxn 2. Heart attack! III. CO = SV x HR A. CO = cardiac output B. SV = stroke volume (ml/beat) 1. ESV Strength of ventricle muscle contractility Ca2+ 2. Preload EDV Venous return pressure due to muscular activity a. Frank Starling Law of the heart: increase preload increase stroke volume b. Preload: Stretch on heart before cxn c. Venous return: blood returned to the heart 3. HR = Heart rate (beats/min) a. Sympathetic (faster) b. Parasympathetic (slower) IV. Blood pressure (mmHg = millimeter of mercury) : hydrostatic pressure exerted by blood on vessel wall A. Highest in arteries and decreases along the way B. Measured via arterial pressure in large arteries close to heart 1. Systolic/diastolic 2. Systolic P = highest pressure in artery before ventricle systole 3. Diastole P = highest pressure in artery before ventricle diastole C. Mean arterial pressure = blood pressure 1. Leaned toward diastole before diastole lasts longer 2. Not mathematical mean V. MAP = CO x TPR A. MAP = Mean arterial pressure B. CO = Cardiac output C. TPR = Total peripheral resistance 1. friction of blood and vessel epithelium 2. Determined by arterio diameter a. Vasocontriction (sympathetic) = increase blood flow = increase TPR b. Vasodilation (parasympathetic) = decrease blood flow = decrease TPR 3. Determined by blood viscosity (thickness of blood) D. Another determinate of MAP: blood volume 1. More blood = more pressure against vessel walls, more blood trying to push through 2. More pressure = more blood pressure VI. Atherosclerosis A. Narrowing of arteries due to fatty plaques (clogging) B. Increases TPR (blood-vessel friction) C. Increases BP