Chapter 20

Cardiovascular System
The Heart
20-1
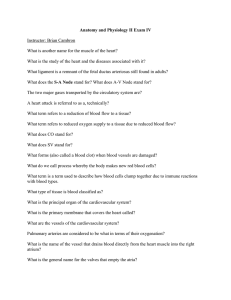
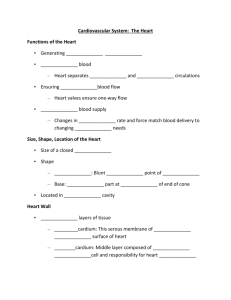
Functions of the Heart
• Generating blood pressure
• Routing blood
–
Heart separates pulmonary and systemic circulations
• Ensuring one-way blood flow
–
Heart valves ensure one-way flow
• Regulating blood supply
–
Changes in contraction rate and force match blood delivery to changing metabolic needs
20-2
Size, Shape, Location of the Heart
• Size of a closed fist
• Shape
– Apex : Blunt rounded point of cone
– Base : Flat part at opposite of end of cone
• Located in thoracic cavity in mediastinum
20-3
Heart Cross Section
20-4
Pericardium
20-5
Heart Wall
• Three layers of tissue
–
Epicardium : This serous membrane of smooth outer surface of heart
–
Myocardium : Middle layer composed of cardiac muscle cell and responsibility for heart contracting
– Endocardium : Smooth inner surface of heart chambers
20-6
Heart Wall
20-7
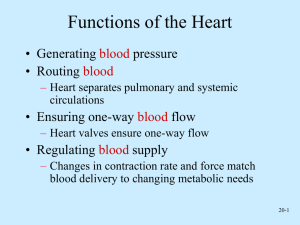
External Anatomy
• Four chambers
–
2 atria
–
2 ventricles
• Auricles
•
Major veins
– Superior vena cava
– Pulmonary veins
•
Major arteries
–
Aorta
– Pulmonary trunk
20-8
External Anatomy
20-9
Coronary Circulation
20-10
Heart Valves
• Atrioventricular
–
Tricuspid
–
Bicuspid or mitral
• Semilunar
–
Aortic
–
Pulmonary
• Prevent blood from flowing back
20-11
Heart Valves
20-12
Function of the Heart Valves
20-13
Blood Flow Through Heart
20-14
Systemic and Pulmonary
Circulation
20-15
Heart Skeleton
• Consists of plate of fibrous connective tissue between atria and ventricles
• Fibrous rings around valves to support
• Serves as electrical insulation between atria and ventricles
• Provides site for muscle attachment
20-16
Cardiac Muscle
• Elongated, branching cells containing 1-2 centrally located nuclei
• Contains actin and myosin myofilaments
• Intercalated disks : Specialized cell-cell contacts
• Desmosomes hold cells together and gap junctions allow action potentials
• Electrically, cardiac muscle behaves as single unit
20-17
Conducting System of Heart
20-18
Electrical Properties
• Resting membrane potential (
RMP ) present
• Action potentials
–
Rapid depolarization followed by rapid, partial early repolarization. Prolonged period of slow repolarization which is plateau phase and a rapid final repolarization phase
–
Voltage-gated channels
20-19
Action Potentials in
Skeletal and Cardiac Muscle
20-20
SA Node Action Potential
20-21
Refractory Period
•
Absolute : Cardiac muscle cell completely insensitive to further stimulation
•
Relative : Cell exhibits reduced sensitivity to additional stimulation
• Long refractory period prevents tetanic contractions
20-22
Electrocardiogram
• Action potentials through myocardium during cardiac cycle produces electric currents than can be measured
• Pattern
– P wave
• Atria depolarization
– QRS complex
• Ventricle depolarization
• Atria repolarization
– T wave:
• Ventricle repolarization
20-23
Cardiac Arrhythmias
•
Tachycardia : Heart rate in excess of 100bpm
•
Bradycardia : Heart rate less than 60 bpm
•
Sinus arrhythmia : Heart rate varies 5% during respiratory cycle and up to 30% during deep respiration
•
Premature atrial contractions : Occasional shortened intervals between one contraction and succeeding, frequently occurs in healthy people
20-24
Alterations in Electrocardiogram
20-25
Cardiac Cycle
• Heart is two pumps that work together, right and left half
• Repetitive contraction ( systole ) and relaxation ( diastole ) of heart chambers
• Blood moves through circulatory system from areas of higher to lower pressure.
–
Contraction of heart produces the pressure
20-26
Cardiac Cycle
20-27
Events during Cardiac Cycle
20-28
Heart Sounds
• First heart sound or “lubb”
–
Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole
• Second heart sound or “dupp”
– Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer
•
Third heart sound (occasional)
– Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole
20-29
Location of Heart Valves
20-30
Mean Arterial Pressure (MAP)
• Average blood pressure in aorta
• MAP=CO x PR
–
CO is amount of blood pumped by heart per minute
• CO=SV x HR
–
SV : Stroke volume of blood pumped during each heart beat
– HR : Heart rate or number of times heart beats per minute
• Cardiac reserve: Difference between CO at rest and maximum CO
– PR is total resistance against which blood must be pumped
20-31
Factors Affecting MAP
20-32
Regulation of the Heart
• Intrinsic regulation : Results from normal functional characteristics, not on neural or hormonal regulation
– Starling’s law of the heart
•
Extrinsic regulation : Involves neural and hormonal control
– Parasympathetic stimulation
• Supplied by vagus nerve, decreases heart rate, acetylcholine secreted
–
Sympathetic stimulation
• Supplied by cardiac nerves, increases heart rate and force of contraction, epinephrine and norepinephrine released
20-33
Heart Homeostasis
• Effect of blood pressure
–
Baroreceptors monitor blood pressure
•
Effect of pH, carbon dioxide, oxygen
– Chemoreceptors monitor
•
Effect of extracellular ion concentration
–
Increase or decrease in extracellular K + decreases heart rate
•
Effect of body temperature
–
Heart rate increases when body temperature increases, heart rate decreases when body temperature decreases
20-34
Baroreceptor and Chemoreceptor
Reflexes
20-35
Baroreceptor Reflex
20-36
Chemoreceptor Reflex-pH
20-37
Effects of Aging on the Heart
• Gradual changes in heart function, minor under resting condition, more significant during exercise
• Hypertrophy of left ventricle
• Maximum heart rate decreases
• Increased tendency for valves to function abnormally and arrhythmias to occur
• Increased oxygen consumption required to pump same amount of blood
20-38