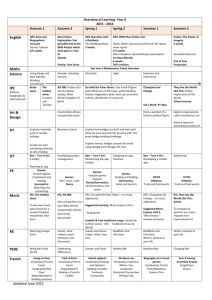
Appendix 6: Infection Prevention and Control Team 2014/15 Audit
advertisement
ANNUAL REPORT OF INFECTION PREVENTION AND CONTROL April 2014 to March 2015 Infection Prevention Control Annual Report 2014/15 CONTENTS Executive introduction from the Director of Nursing & Operations and Director of Infection Prevention & Control Section One: Introduction..................................................................................... 1 Section Two: Who we are, our duties, arrangements and assurance ............. 3 Who we are ............................................................................................................. 3 Our Duties and Arrangements ................................................................................. 3 Assurance and Reporting to the Board .................................................................... 4 Section Three: Position in Relation to Health Care Associated Infections ..... 6 MRSA Bacteraemia Trust Target............................................................................. 6 Actions taken to prevent MRSA bacteraemia .......................................................... 7 MRSA Screening ..................................................................................................... 7 Clostridium difficile Infection (CDI) Targets.............................................................. 8 CDI 30 day mortality rate ....................................................................................... 10 Actions to reduce CDI ............................................................................................ 10 Periods of Increased Incidence ............................................................................. 12 Outbreaks .............................................................................................................. 12 Gastrointestinal Infection ....................................................................................... 12 Influenza Outbreaks .............................................................................................. 14 Glycopeptide-Resistant Enterococci (GRE) also known as Vancomycin-Resistant Enterococci (VRE) ................................................................................................. 15 Extended Spectrum Beta-Lactamase (ESBL)........................................................ 16 Carbapenemase-producing Enterobacteriaceae (CPE) ........................................ 16 Safe Care Shropshire ............................................................................................ 16 Catheter-associated Urinary Tract Infection (CAUTI) Sub Group .......................... 16 The NHS Trust Development Authority (TDA) visit 14-15 May 2014 ..................... 17 Section Four: Progress against 2014/15 Infection Prevention and Control Programme........................................................................................................... 19 Criterion 1 – Systems to manage and monitor the prevention and control of infection. These systems use risk assessments and consider how susceptible service users are and any risk that their environment and other users may pose to them. ..................................................................................................................... 19 Criterion 2 - Provide and maintain a clean and appropriate environment in a managed premises that facilitates the prevention and control of infections ........... 20 Criterion 3 - Provide suitable accurate information on infections to service users and their visitors .................................................................................................... 24 Criterion 4 - Provide suitable accurate information on infections in a timely fashion to any person concerned with providing further support or nursing / medical care 24 Criterion 5 - Ensure that people who have or develop an infection are identified promptly and receive the appropriate treatment and care to reduce the risk of passing on the infection to other people ................................................................ 25 Criterion 6 - Ensure that all staff and those employed to provide care in all settings are fully involved in the process of preventing and controlling infection ................ 26 Criterion 7 - Provide or secure adequate isolation facilities ................................... 27 Criterion 8 - Secure adequate access to laboratory support as appropriate .......... 27 Criterion 9 - Have and adhere to policies, designed for the individual's care and provider organisations that will help to prevent and control infections ................... 27 Medicines Management Report ............................................................................. 28 Infection Prevention Control Annual Report 2014/15 Criterion 10 - Ensure, so far as reasonably practicable, that care workers are free of and are protected from exposure to infections that can be caught at work and that all staff are suitably educated in the prevention and control of infection associated with the provision of health and social care ......................................... 29 Section Five: Hand Hygiene ............................................................................... 38 Hand Washing Assessments ................................................................................. 38 Hand Hygiene Observational Audit ........................................................................ 38 Bare Below the Elbows .......................................................................................... 39 Section Six: 2014/15 Infection Prevention and Control Team Audit Programme........................................................................................................... 40 Overall Score and Compliance Rating ................................................................... 40 Reporting and Monitoring ...................................................................................... 40 Summary of audit findings and actions taken: ....................................................... 40 Self-audits/checklists ............................................................................................. 40 Section Seven: Looking Forward to 2015/16 .................................................... 42 An Overview of Infection Prevention and Control Programme 2015/16 ................. 42 2015/16 Local Infection Prevention and Control Commissioning Objectives ......... 43 2015/16 Infection Targets ...................................................................................... 43 2015/16 IPC Key Performance Indicator ............................................................... 43 Section Eight: Glossary of Terms ...................................................................... 44 Appendix 1: 2014/15 Community Hospital Audit Programme ................................ 46 Appendix 2: 2014/15 Community Services Audit Programme ............................... 50 Appendix 3: 2014/15 Community Hospital Cleanliness Audit Scores .................... 52 Appendix 4: Analysis of HCAI Audits in Community Hospitals .............................. 55 Appendix 5: 2014/15 Community Hospital Self-Audit Scores ................................ 58 Appendix 6: Infection Prevention and Control Team 2014/15 Audit Programme ... 62 Infection Prevention Control Annual Report 2014/15 Executive introduction from the Director of Nursing & Operations and Director of Infection Prevention & Control Dear Staff, Patients, Carers, Service Users and Partners Welcome to Shropshire Community Health Trust’s Infection Prevention and Control Annual report which has been developed in collaboration with the Head of Infection Prevention and Control and the Infection Prevention and Control team. The purpose of this report is to outline the activities of SCHT relating to infection prevention and control for the year from April 2014 to March 2015 and explain how SCHT has arrangements in place to reduce the spread of infections. It also reviews accountability arrangements, policies and procedures relating to infection prevention and control, audit, and education necessary in order to support prevention and control of infection. Our key achievements were: Zero MRSA bacteraemia attributed to SCHT The set target of no more than three post 72 hour cases of Clostridium difficile infections was achieved The set target of 95% MRSA screening compliance was exceeded Mandatory training including Infection Prevention and Control attended by 95.5% of clinical staff Positive report by the Head of Infection Prevention and Control at the NHS Trust Development Authority following their visit in June. Constructive advice was implemented through service improvement plans. No follow up visit was required Looking forward to 2015-2016 the IPC team and all SCHT staff will continue to work hard and focus on the prevention of all infections. Steve Gregory Director of Nursing & Operations and Director of Infection Prevention & Control Infection Prevention Control Annual Report 2014/15 Section One: Introduction The purpose of this report to provide assurance to the Board of Directors and the public for the reporting period 01 April 2014 – 31 March 2015 regarding the Infection Prevention and Control (IPC) activity including compliance with the Health & Social Care Act 2008: Code of Practice on the prevention and control of infections and related guidance (commonly known as The Hygiene Code) and also in relation to National Institute for Health and Clinical Excellence (NICE) guidance. This annual report fulfils its statutory requirements under the Health & Social Care Act 2008: Code of Practice on the prevention and control of infections, which sets out 10 compliance criteria against which a registered provider will be judged on how it complies with the registration requirements for cleanliness and infection prevention and control. It sets the basis of our annual programme which is monitored at the Shropshire Community Health Trust (SCHT) Infection Prevention and Control bi-monthly meeting. The aim of the Infection Prevention and Control team is to increase organisational focus and collaborative working so to ensure continued compliance and quality improvement. SCHT is registered with the Care Quality Commission (CQC) and declared full compliance with the ten compliance criteria as detailed in Table 1. Table 1: The requirements of the Health and Social Care Act (2008) Compliance What the registered provider will need to demonstrate criterion 1 2 3 4 5 6 7 8 9 10 Systems to manage and monitor the prevention and control of infection. These systems use risk assessments and consider how susceptible service users are and any risks that their environment and other users may pose to them Provide and maintain a clean and appropriate environment in managed premises that facilitates the prevention and control of infections Provide suitable accurate information on infections to service users and their visitors Provide suitable accurate information on infections to any person concerned with providing further support or nursing / medical care in a timely fashion Ensure that people who have or develop an infection are identified promptly and receive the appropriate treatment and care to reduce the risk of passing on the infection to other people Ensure that all staff and those employed to provide care in all settings are fully involved in the process of preventing and controlling infection Provide or secure adequate isolation facilities Secure adequate access to laboratory support as appropriate Have and adhere to policies, designed for the individual’s care and provider organisations that will help to prevent and control infections Ensure, so far as is reasonably practicable, that care workers are free of and are protected from exposure to infections that can be caught at work and that all staff are suitably educated in the prevention and control of infection associated with the provision of health and social care Infection Prevention Control Annual Report 2014/15 Page 1 of 62 The SCHT Board and ultimately the Chief Executive Officer carries responsibility for infection prevention and control (IPC) throughout SCHT and is a vital component of Quality and Safety. The day to day management is delegated to the Director of Infection Prevention and Control (DIPC). All managers and clinicians ensure that the management of IPC risks is one of their fundamental duties. Every clinical member of staff demonstrates commitment to reducing the risk of HCAI through standard infection prevention and control measures. The IPC team endeavours to provide a comprehensive proactive service, which is responsive to the needs of staff and public alike, and is committed to the promotion of excellence within everyday practice of IPC. The 2014/15 NHS Outcomes Framework included reducing the incidence of Healthcare Associated Infections (HCAIs), in particular Meticillin Resistant Staphylococcus aureus (MRSA) bacteraemia and Clostridium difficile infections (CDI) as areas for improvement. Within Domain 5: Treating and caring for people in a safe environment and protecting them from avoidable harm of the Outcomes Framework reducing all HCAIs remained a priority. As reported last year, the extension to the mandatory surveillance to meticillin sensitive Staphylococcus aureus (MSSA) bacteraemia infections since January 2011 and Escherichia coli (E.coli) bacteraemia infections since June 2011, together with the meticillin resistant Staphylococcus aureus (MRSA) bacteraemia and Clostridium difficile national reduction targets set for Acute and Clinical Commissioning Groups (CCGs) reflects the zero tolerance approach for all avoidable HCAIs. This report will provide information of the activities and performance of Key Performance Indicators (KPI) for IPC during the period 1 April 2014 to 31 March 2015 by SCHT. The report is aligned to the 2014/15 Infection Prevention and Control Programme, informing progress against the objectives set and outlines performance of SCHT against the MRSA bacteraemia and CDI reduction targets. In addition the report aims to reassure the public that reducing the risk of infection through robust infection prevention and control practice is a key priority for SCHT and supports the provision of high quality services for patients and a safe working environment for staff. Infection Prevention Control Annual Report 2014/15 Page 2 of 62 Section Two: Who we are, our duties, arrangements and assurance Who we are SCHT provides community-based health services to around 460,000 people in Shropshire and Telford and Wrekin. These include for example four community hospitals, community nursing and inter-disciplinary teams, health visiting, advanced primary care services and children’s services. SCHT has a committed IPC team that is very clear on the actions necessary to deliver and maintain patient safety. Equally, it is recognised that infection prevention and control is the responsibility of every member of staff and must remain a high priority for all to ensure the best outcome for patients. The IPC team utilises a proactive approach with the emphasis on being visible so making their accessibility for guidance and advice a priority. This in turn has led to an improved IPC team image i.e. being a regular familiar face rather than only visiting for an audit or when there are problems. Looking forward it is critical that we maintain this level of commitment. As in previous years, we will continue to work with Shrewsbury and Telford Hospital Trust (SaTH), Robert Jones and Agnes Hunt Hospital, Shropshire Clinical Commissioning Group (SCCG), Telford and Wrekin Clinical Commissioning Group (TWCCG) in the Local Health Economy (LHE) as well as experts in other organisations, Public Health England (PHE) and the NHS Trust Development Authority (TDA), Midlands and East of England. Our Duties and Arrangements Infection Prevention and Control Service: Director of Infection Prevention & Control (also Director of Nursing and Operations) Head of Infection Prevention and Control (0.8 WTE) Infection Prevention and Control Nurses (1.6 WTE) Infection Prevention and Control Nurse (1.0 WTE) left December 2014 - post not replaced Infection Prevention and Control Secretary (1.0 WTE) Reduced staffing since the beginning of 2015 has proved to be challenging however it created an opportunity to review the team’s priorities and new ways of working. The IPC team is led by Steve Gregory, Director of Nursing and Operations who is the Director for Infection Prevention and Control (DIPC) and reports directly to the Chief Executive. The IPC team devises and implements a robust Annual Programme of Work to reduce HCAI. This is achieved by working in collaboration with all SCHT services and staff. The IPC team perform a number of activities that minimise the risk of infection to patients, staff and visitors including advice on all aspects of infection prevention and The IPC team: From left to right: Head of IPC Rachael Allen, team secretary Alison Davies, IPC nurse Liz Jones and IPC nurse Lizzie Watkins Infection Prevention Control Annual Report 2014/15 Page 3 of 62 control; education and training; audit; formulating policies and procedures; interpreting and implementing national guidance at local level, alert organisms surveillance and managing outbreaks of infection. SCHT has a Service Level Agreement for specialist support from a Consultant Microbiologist at SaTH to act as SCHT’s IPC Doctor. SCHT also sought advice from Public Health England when additional advice was required. Medical microbiology support is provided 24 hours a day, 365 days a year through on-call arrangements by SaTH. The IPC team also works with a team of 57 IPC link staff, with 35 working in community services, 21 from the community hospitals and one from Stoke Heath Prison, who receive additional training in infection prevention and control and also support clinical staff. Assurance and Reporting to the Board Trust Board – SCHT’s performance against the Meticillin Resistant Staphylococcus aureus (MRSA) bacteraemia and Clostridium difficile infection (CDI) national reduction targets and the MRSA screening threshold are included in the Performance Report and Quality Safety Report which are presented at each SCHT Board meeting. Quality and Safety Committee – Quarterly IPC reports are presented to the Quality and Safety Committee meetings. Infection Prevention and Control Meeting – The membership is multi-disciplinary and includes representation from the operations and quality directorates, estates department and medicines management. Additional members are, a Health Protection Nurse from Public Health England; Shropshire and Telford & Wrekin CCGs’ Head of IPC and a patient representative. The meeting is chaired by the Director for Infection Prevention and Control (DIPC) and meets bi-monthly. The Terms of Reference (TOR) and membership are reviewed annually to ensure responsibility for IPC continues to be embedded across the organisation. This meeting monitors the progress of the annual IPC programmes, approves IPC policies and monitors compliance with them. Health Economy Infection Prevention and Control Group – This pan-Shropshire group was established in 2014/15 with the first meeting being held in September 2014. SCHT is represented by the Head of IPC. As with the Diagnosis Prevention and Control of Infection Implementation Group which preceded it, the new group will aim to ensure a strategic oversight. To facilitate and engage all agencies, a five year strategy has been developed to support the ability to identify local needs and aspires to a common vision for infection prevention and control for Shropshire and Telford and Wrekin. The strategy outlines five strategic objectives which are based on the NICE Guidance Prevention and Control of Infection – Quality Improvement Guide (NICE 2011) which will form the basis of the system wide approach. Infection Prevention and Control Team – The IPC nurses meet formally on a monthly basis with the IPC Doctor to offer a supportive environment within which clinical issues are discussed and a consensus obtained. Infection Prevention and Control Link Staff – All IPC link staff have signed a roles and responsibilities pro-forma. The aim of the link staff is to enhance the IPC knowledge of healthcare professionals working within SCHT, ensuring the delivery of high standards of Infection Prevention Control Annual Report 2014/15 Page 4 of 62 quality and patient safety in relation to IPC. They are also responsible for undertaking IPC audits, where required and for disseminating IPC information to colleagues. Clinical Service Managers, Sisters and Team Leaders – Clinical Service Managers (CSMs), sisters and team leaders are responsible for ensuring that their work environments are maintained at high levels of cleanliness. Bi-monthly cleanliness audits are under taken with ward and housekeeping staff. These audits are reported in the CSM’s reports to the IPC meeting. The CSMs, sisters and team leaders are responsible for ensuring the link staff are supported in performing their role and have appropriate time and resources to do this effectively. Audit and ongoing work undertaken by the link staff is included in the CSMs’ report submitted to the IPC meeting. Organisational Development Team – Arrangements are in place for staff to attend induction and mandatory training programmes which includes IPC. Arrangements are in place for staff training to be effectively recorded and maintained in staff records. Alerts inform managers of their staff’s non-compliance with mandatory training. Role of all Staff – All staff are responsible for ensuring that they follow the standard IPC precautions at all times and are familiar with IPC policies, procedures and guidance relevant to their area of work. All staff have a duty of care to report any non-compliance and take the appropriate action as appropriate. Infection Prevention Control Annual Report 2014/15 Page 5 of 62 Section Three: Position in Relation to Health Care Associated Infections The local acute Trust, whose microbiology laboratory process specimens from SCHT patients, submit data on SCHT’s behalf on Meticillin Resistant Staphylococcus aureus (MRSA) bacteraemia, Meticillin Sensitive Staphylococcus aureus (MSSA) bacteraemia, Escherichia coli (E.coli) bacteraemia infections and Clostridium difficile infections (CDI), to PHE, as part of the national mandatory surveillance programme for Healthcare Associated Infections (HCAI). SCHT does not have nationally set targets for reducing HCAIs. These targets are set for acute Trusts and CCGs. However, SCHT recognises it does have a responsibility in contributing to the overall reduction targets of both Shropshire and Telford & Wrekin CCGs and therefore agreed local infection targets with commissioners using the new 2014/15 NHS England methodology for calculating organisational CDI objectives. MRSA Bacteraemia Trust Target Table 2 below outlines the performance of SCHT against MRSA bacteraemia and confirms that SCHT succeeded in meeting its target for the second consecutive year with zero cases in 2014/15. Table 2: Pre 48hr MRSA Bacteraemia cases assigned to SCHT Actual Apr 14 0 May 14 0 Jun 14 0 Jul 14 0 Aug 14 0 Sep 14 0 Oct 14 0 Nov 14 0 Dec 14 0 Jan 15 0 Feb 15 0 Mar 15 0 Total 0 Year End Target 0 In the event of a MRSA bacteraemia the IPC team would work with the clinical team(s) involved and facilitate a Post Infection Review (PIR), followed by a multi-disciplinary review meeting. Subsequently, service improvement plans (SIPs) would be developed and lessons that have been learnt and good practices identified shared with other services as appropriate. Indeed this process was activated in June 2014 when the Shrewsbury and Atcham community nursing team and podiatry were involved in the care of a patient whose pre-48hrs blood culture was MRSA positive. A PIR was led by the SCCG IPC team and following a review meeting it was agreed that the case should not be assigned to SCHT nor was it to be finally assigned to SCCG on the national infection Data Capture System as it was unavoidable. However, a number of issues with both the SCHT services involved were identified and as a result a SIP was developed and a report was submitted to the IPC meeting. The main conclusion was that the patient had received excellent care from both SCHT and SaTH. Again in January 2015 the IPC team assisted with a PIR led by the CCG IPC team involving a pre-48 hours MRSA bacteraemia diagnosed in SaTH from a patient who was receiving care from the Newport Community Nursing team. A PIR meeting was held where it was agreed the case was unavoidable and requested that there should be a case review via the arbitration process. The final outcome finds the case was assigned to a third party as there were no lapses in patient care which would have contributed to the MRSA bacteraemia. Infection Prevention Control Annual Report 2014/15 Page 6 of 62 Actions taken to prevent MRSA bacteraemia In 2014/15 the focus continued on key interventions to prevent cases of MRSA bacteraemia. These included: Management of MRSA and MRSA Screening policies available Screening of emergency and elective admissions to community hospitals for MRSA. Compliance monitored by the IPC Meeting and included in the Performance Report - see Table 2 for details Continued emphasis on isolation and clearance treatment of MRSA infected and colonised patients within community hospitals Completion of isolation audits / checklists by ward staff on commencement of source isolation and weekly thereafter whilst patient remains on the ward Continue to monitor the care of patients with MRSA within community hospitals using the management protocol and care pathway Continued improvement in compliance with hand hygiene and alcohol hand rub available in every bedspace MRSA screening of high risk patients prior to urinary catheter change Urine specimens taken prior to and/or at urinary catheterisation Urinary catheter practices included in audit programme Community antibiotic guidelines promoted and placed on computer desk tops within community hospitals Ward pharmacists review antimicrobial prescriptions and undertake regular antibiotic prescribing audits PIR undertaken on each case of MRSA bacteraemia, including as appropriate, joint reviews between the community and the acute Trusts Insertion and on–going care of peripheral vascular devices included in selfaudit/checklist programme Letters sent to GPs informing them of MRSA diagnosed whilst an in-patient MRSA staff screening/treatment policy available Continued emphasis on importance of the cleanliness of the environment: revision of community hospital cleaning policy and schedules Continuation of the annual validation of hotel services cleanliness audits by IPC nurses Certificates awarded to areas who achieved an annual 100% MRSA screening compliance MRSA and Reducing the Risk of HCAIs information leaflets available to all services and on SCHT website MRSA Screening In addition to the local infection targets, a compliance threshold of 95% for MRSA screening for patients on admission was agreed with the CCG. Again this year the threshold has been achieved with an overall MRSA screening compliance of 99.29% a slight improvement compared with last year’s 99.1%. The Head of IPC shares the monthly compliance reports of all four sites with Ward managers, CSMs and with the Divisional Service Manager. As shown in Table 3 below, Team 2 at Whitchurch Community Hospital and Bishops Castle Hospital have consistently achieved 100% each month throughout the year and in recognition have been awarded a certificate to acknowledge this achievement (see below). Infection Prevention Control Annual Report 2014/15 Page 7 of 62 Ward Managers are responsible for investigating reasons for non-compliance and to instigate actions to improve. Table 3: Compliance in each Community Hospital with the MRSA screening policy Bishops Ludlow Ludlow Whitchurch Whitchurch Bridgnorth Overall Castle Dinham Stretton Team 1 Team 2 Apr-14 100 97 100 100 100 100 99.50 May-14 100 100 100 100 100 100 100.00 Jun-14 100 100 100 96 96 100 98.67 Jul-14 100 100 100 100 100 100 100.00 Aug-14 100 100 93 100 100 100 98.83 Sep-14 100 97 100 100 100 100 99.50 Oct-14 100 100 100 100 100 100 100.00 Nov-14 100 100 100 97 100 100 99.50 Dec-14 100 100 100 100 100 100 100.00 Jan-15 100 100 100 100 100 100 100.00 Feb-15 100 100 95 85 100 100 96.67 Mar-15 100 100 100 93 100 100 98.8 Overall 100 99.50 99.00 97.58 99.67 100 99.29 Green - >95% Amber - 90-95% Red - <90% Staff at Bishop Castle Hospital with their certificate for achieving 100% MRSA screening compliance for patients on admission Ward staff from Whitchurch Team 2 receive their certificate for achieving 100% MRSA screening compliance for patients on admission Clostridium difficile Infection (CDI) Targets The local target set for SCHT was to have no more than three cases of CDI diagnosed post 72 hours after admission in the community hospitals attributed to SCHT. Three cases were recorded as seen in Table 4. Infection Prevention Control Annual Report 2014/15 Page 8 of 62 Table 4: Post 72hr Clostridium difficile infections cases diagnosed in Community Hospitals Actual Apr 14 May 14 Jun 14 Jul 14 Aug 14 Sep 14 Oct 14 Nov 14 Dec 14 Jan 15 Feb 15 Mar 15 Total Year End Target 0 0 0 0 1 0 0 1 0 0 1 0 3 No more than 3 The first patient diagnosed with a post 72 hour CDI was in August 2014 and was transferred to Bridgnorth Community Hospital from PRH with known CDI, and immediately isolated in a side room. A further and unnecessary sample was collected at Bridgnorth Community Hospital on Day 29 (therefore classed as another case) as the patient still had diarrhoea. Both specimens were confirmed as the same Ribotype 015 therefore the second sample was not a new infection. A Root Cause Analysis (RCA) was performed and reviewed at a meeting where the findings were discussed, including issues with documentation e.g. isolation self-audits not completed, inaccurate completion of stool chart, CDI care pathway not commenced at the correct time and not always completed daily. The use of agency staff (25% in August) to cover the ward was also noted. A SIP was completed. The second CDI patient diagnosed post 72 hours was on Stretton Ward at Ludlow Community Hospital in November. The patient had a number of risk factors for CDI. A RCA was completed and at the review meeting in December the following issues were discussed: delay in stopping antibiotics; date of specimen on label incorrect; lack of precise documentation and staff awareness of patient’s condition which contributed to a delay in treatment and in transfer to SaTH. In conclusion, if the specimen had been dated correctly the case would have been deemed pre 72 hours and therefore would not show against the SCHT target. At the RCA review meeting, it was concluded that the acquisition of CDI was unavoidable; however because of the identified lapses in care the case counted against SCHT’s target. A SIP was produced to address the issues and all actions have been completed. The third post 72 hour CDI was diagnosed in February, the patient was on Stretton Ward at Ludlow Community Hospital. A joint RCA was undertaken by IPC, the ward staff and Medicines Management, which was reviewed by the Head of IPC for CCGs and it was agreed there were no lapses in care by SCHT which could have attributed to the patient acquiring CDI. However, it was noted that SCHT do need to be aware of the wider implications and importance of shared learning within the Health Economy. In line with the RCA policy all three infections were reported to and discussed at IPC meeting. Table 5 shows the total number of CDI in Shropshire and Telford Health Economy in patients over two years of age from April 2008 to March 2015, also showing the year-on-year reduction in the total number of CDI and encouragingly a 66% reduction in seven years. Infection Prevention Control Annual Report 2014/15 Page 9 of 62 Table 5: Total number and proportion deemed to be attributed to SCHT Community Hospitals Year Total Number of Cases in LHE Community Hospital Attributed 2008/09 285 2 (0.7%) 2009/10 206 3 (1.4%) 2010/11 191 4 (2.1%) 2011/12 147 1 (0.6%) 2012/13 145 6 (4.1%) 2013/14 112 2 (1.8%) 2014/15 98 3 (3%) CDI 30 day mortality rate A consultant microbiologist at SaTH monitors the local health economy CDI mortality data which includes patients in SCHT. Routinely the IPC team follows the progress of our CDI patients and therefore would be aware if they died before 30 days. All three CDI patients discussed above responded to treatment and were discharged. If the cause of death is recorded as CDI on section 1 of the death certificate it is automatically reported as a Serious Incident (SI). To improve future care and patient outcomes all Community Hospital deaths are scrutinised by the Community Hospitals’ mortality group with a checklist approach, and any unexpected deaths are subject to a review, which would include HCAI/infections including CDI. Actions to reduce CDI In 2014/15 we continued to focus on the key actions to reduce the number of cases of CDI. Actions specifically targetted at reducing CDI in 2014/15 included: Promotion of, and referral to, the guidance sheet developed in previous year for GPs, including those working in community hospitals, to support measures which need to be adopted to assist in reducing CDI and improving patient care Bespoke IPC training for medical staff working in Community Hospitals Continued monitoring of antibiotic prescribing by the community hospital pharmacists in line with community antibiotic guidelines and any non-compliance brought to the attention of the prescribing doctor Review of proton pump inhibitors in inpatients by community hospital pharmacists Continuation of 7 day rapid testing for Clostridium difficile and use of typing to search for clusters or linked cases Continual surveillance, RCA and monitoring of the care of patients who develop CDI whilst an in-patient in community hospitals and/or whilst receiving care from our community services using the management protocol and care pathway Multi-disciplinary team review meeting held after RCA completion to ensure SIP developed as appropriate Presentation of each CDI case at next IPC Meeting to discuss and gain assurance the SIP completed and lessons learnt are shared Rapid isolation of patients presenting with diarrhoea in community hospitals and on-going isolation checklist performed Revision of community hospital cleaning policy and cleaning schedules Continuation of increased cleaning, including use of chlorine based disinfectants Infection Prevention Control Annual Report 2014/15 Page 10 of 62 Continue to promote use of decontamination status bands identifying equipment which is clean and ready for use Continued emphasis on de-cluttering, cleanliness and efficient use of ward space Annual validation of hotel services’ cleanliness audits by IPC nurses Antibiotic Awareness information board in William Farr House – to reinforce key messages and remind staff about the importance of prudent antibiotic prescribing and of the need not to ask for unnecessary antibiotics In collaboration with Medicines Management promotion of the annual global antibiotic awareness day on 18 November Continued improvement in compliance with hand hygiene and emphasis on the need to use soap and water, not alcohol hand gel, with Clostridium difficile and other gastro intestinal illnesses Hand hygiene observation audits completed monthly by ward Link Staff and reported to IPC IPC training programmes focused upon Clostridium difficile prevention, management of individual cases including isolation practices Reinforced public health messages regarding inappropriate use of antibiotics, through Inform and staff desktops Continue to issue the CDI passport (see below) to help clinicians improve patient outcomes and increase patient understanding of Clostridium difficile and involvement in decisions regarding their care Letters to GPs informing them of CDI diagnosis (both infection and carrier status) whilst an in-patient The Shropshire and Telford Health Economy Clostridium difficile Task and Finish Group ceased in July 2014 and SCHT worked in conjunction with the Health Economy IPC Group on the CDI reduction programme Continued to promote the SIGHT mnemonic protocol when managing suspected potentially infectious diarrhoea Issued and encourage all ward based staff to carry the credit sized ‘SIGHT’ cards for reference : Infection Prevention Control Annual Report 2014/15 Page 11 of 62 S Suspect that a case may be infective where there is no clear alternative cause of diarrhoea I Isolate the patient (within 2 hours), clean vacated bed space and consult with the infection prevention and control team while determining the cause of diarrhoea G Gloves and aprons must be used for all contacts with the patient and the patient’s environment H Hand washing with soap and water should be carried out before and after each contact with the patient, their environment and following removal of PPE T Hand wash with soap and water Use personal protective equipment (PPE) Keep all doors closed and avoid use of fans Designate patient equipment (commodes, bedpan holders, hoist slings, glide sheets, BP cuffs, stethoscope) Allocate staff to work on affected or non-affected areas Use stool reord chart and fluid balance chart Use Fuse and Jet for cleaning and disinfecting Avoid patient transfers unless clinical emergency Inform visitors of infection risks Terminal clean when patient 48 hours free of symptoms Test faeces, by sending a specimen immediately Periods of Increased Incidence Since April 2010 all Trusts have been asked to report periods of increased incidence (PII) of cases of MRSA bacteraemias and CDIs. The definition of a PII is two or more cases within a ward in a 28 day period. In 2014/15 no PII were reported in the SCHT’s four community hospitals. Outbreaks An outbreak of infection is described as two or more people with the same disease or symptoms or the same organism isolated from a diagnostic sample and are linked through a common exposure, personal characteristics, time or location. Table 6 below summarises the outbreaks declared in the Community Hospitals during 2014/15. Table 6: Total outbreaks declared in Community Hospitals in 2014/15 Patients Affected/ Staff Affected Date Commenced Date Declared Over 14/12/2014 22/12/2014 5/2 05/01/2015 07/01/2015 2/0 07/01/2015 22/01/2015 8/5 26/02/2015 02/03/2015 3/2 11/03/2015 19/03/2015 6/0 Whitchurch Team 2 15/03/2015 26/03/2015 15/2 Whitchurch Team 1 15/03/2015 24/03/2015 5/2 Hospital & Ward Ludlow, Dinham Ludlow, Dinham Whitchurch Whitchurch Team 1 Ludlow, Dinham Symptoms Causative Organism Diarrhoea and vomiting Diarrhoea and vomiting Influenza like illness Diarrhoea and vomiting Diarrhoea and vomiting Diarrhoea and vomiting Norovirus Diarrhoea and vomiting Norovirus Norovirus Influenza Nil identified Norovirus Norovirus Gastrointestinal Infection Norovirus is the most common cause of gastroenteritis in the community but also causes outbreaks in hospitals as it is very infectious. During 2014/15 there have been six gastrointestinal infection outbreaks in SCHT’s community hospitals, one assumed to be and five of which were confirmed by the laboratory to be caused by Norovirus. The outbreaks in Infection Prevention Control Annual Report 2014/15 Page 12 of 62 Whitchurch Team 1 and Team 2 in February and March respectively resulted in bed closures to control the infection due to all areas affected on Team 2. The ward was closed for several days and reported as a SI. In all the outbreaks Norovirus was known to be circulating in the local communities. Despite continual requests and communications it was acknowledged that some visitors did not heed the advice discussed below. As part of a campaign to help reduce the introduction and spread of Norovirus within the community hospitals, all four sites erected their display banners in October (acknowledged as the start of the Norovirus season) at the entrance to the wards/reception areas. These advised visitors of the signs and symptoms of Norovirus and requested they do not visit the hospital if they are unwell or not clear of symptoms for at least 48 hours. In addition, in partnership with SaTH the IPC team used the local media and the SCHT website to reinforce these key messages. In each of the outbreaks, enhanced cleaning of the wards was immediately introduced and symptomatic patients were either nursed in a single room or cohorted in the same bay. To support the efforts of all staff in their attempts to keep these outbreaks under Banner at entrance of ward advising control, the IPC team communicated at least once daily visitors of signs and symptoms of with the affected area to offer guidance of patient norovirus management and placement, adherence to control measures and advised the use of a range of tools designed to assist in the care and monitoring of affected patients. Close monitoring in this way meant that the disruption to patients and SCHT was kept to a minimum. Throughout the outbreaks the ward staff were encouraged to complete the isolation checklist to ensure adherence with the isolation policy. The rationale being that staff address any issues immediately to ensure safety for all; therefore a SIP is not required. A copy of the checklist is faxed to IPC for assurance and advice if required. Outbreak de-brief meetings were not required following the first four Norovirus outbreaks as all the appropriate actions were taken at the time. A few IPC recommendations were made to Dinham Ward in December and were discussed at the ward meeting. A debrief meeting was held following the Whitchurch outbreaks in March, where good practice was acknowledged: the epidemic curve (see Figures 1 and 2 below) and factors which may have contributed to the outbreak discussed, including staff working on both teams; challenges maintaining some patients in isolation rooms; patients requiring 1:1 care; breaches in IPC isolation precautions e.g. doors open, fan in use, Personal Protective equipment (PPE) not used appropriately; unable to designate staff and environmental issues where some areas of the wards were too hot or too cold. A SIP was developed with realistic completion dates and a follow up review meeting arranged. Lessons learnt and best practice was shared with staff via the community hospital sisters’ and ward manager forums, IPC Link Staff meeting and the IPC meeting. Informing colleagues within the local health economy is a vital strategy to help contain the spread of Norovirus. The IPC team email all organisations involved with health and social Infection Prevention Control Annual Report 2014/15 Page 13 of 62 care to alert them of outbreaks declared within SCHT. Equally, SCHT is informed of outbreaks elsewhere within the local health economy. To enable accurate regional and national surveillance of diarrhoea and vomiting the IPC team submitted reports of outbreaks to PHE and the TDA. All outbreaks are reported to Risk Management via Datix. Norovirus Outbreak Team 1, Whitchurch Hospital March 2015 6 5 4 3 2 1 0 17th 18th 19th 21st New Cases Per Day 22nd 23rd 24th Total Cases Affected Figure 1: Whitchurch Team 1 Epidemic Curve Norovirus Outbreak Team 2, Whitchurch Hospital March 2015 16 14 12 10 8 6 4 2 0 16th 17th 18th 19th 20th New Cases Per Day 21st 22nd 23rd 24th 25th Total Cases Affected Figure 2: Whitchurch Team 2 Epidemic Curve Influenza Outbreaks Whitchurch Community Hospital Teams 1 and 2 reported to the IPC team on 7 January a number of patients with influenza-like illness (ILI), including admissions with symptoms over the New Year period. Throat/nose swabs and sputum specimens were obtained from 11 Infection Prevention Control Annual Report 2014/15 Page 14 of 62 patients in total. Five patients were confirmed as Influenza A positive and all prescribed Oseltamivir six patients’ swabs were negative. A patient was admitted from SaTH with ILI and chest infection and also tested positive for Influenza A. Subsequently, three additional patients were treated on symptoms alone and 12 asymptomatic patients sharing the rooms or bays prescribed the prophylactic dose of Oseltamivir. In total eight patients were treated as influenza positive. Patients were nursed in source isolation in co-horted bays as there were insufficient single rooms available. In addition five members of staff reported symptoms but none were swabbed. The outbreak was declared over on 22 January after only 13 days. It was acknowledged at the debrief meeting which included colleagues from PHE and a Consultant microbiologist that Influenza A was circulating in the community, including identified outbreaks in local care homes. The epidemic curve (see Figure 3 below) was discussed, with the overall conclusion the outbreak was not prolonged and it had been well managed. However, several recommendations were made and would be addressed in the SIP including the patient information leaflet not being available on the ward, delay in prescribing of and insufficient stock of anti-viral medication and ward staff not alert for influenza. Influenza Outbreak Whitchurch Hospital January 2015 10 9 8 7 6 5 4 3 2 1 0 8th 9th 10th 15th New Cases Per Day 16th 19th 20th 21st 22nd Total Cases Affected Figure 3: Whitchurch Teams 1 and 2 Epidemic Curve Glycopeptide-Resistant Enterococci (GRE) also known as Vancomycin-Resistant Enterococci (VRE) IPC surveillance of antibiotic resistance organisms also includes VRE. The year 2014-15 has seen a rise in the number of SCHT patients identified as colonised and or infected with VRE. The Enterococcus is a bacterium that everyone has in their bowel. Vancomycin is one of the antibiotics used to treat infections caused by the Enterococcus bacterium. Infection Prevention Control Annual Report 2014/15 Page 15 of 62 Healthy people can carry GRE/VRE with no ill effects or signs and symptoms. This is called colonisation. People who are colonised do not need treatment. GRE/VRE may cause infection in compromised patients such as bacteraemia, wound infections, meningitis and indwelling device infections. GRE/VRE infections can be difficult to treat because they are resistant to Vancomycin. There is no treatment to clear colonisation of GRE/VRE and therefore the control of GRE/VRE in a hospital environment can be very difficult once it has become established. Seven patients known to have VRE have been admitted to the community hospitals. In all cases IPC recommend source isolation precautions for 48 hours while an assessment of the patient is made. Prevention of transmission is through effective standard precautions. A GRE/VRE policy is available for all staff for reference. To date IPC are not aware of any patients acquiring VRE while in the community hospitals. Extended Spectrum Beta-Lactamase (ESBL) ESBL is also included in IPC’s multi resistant organism surveillance. These Gram-negative organisms are resistant to all cephalosporins, penicillins and usually also to ciprofloxacin, trimethoprim and sometimes gentamicin. Transmission within hospitals mainly occurs via the hands of healthcare workers which have been contaminated by contact with colonised or infected patients; contaminated surfaces or inanimate objects. Gram-negative bacteria may contaminate the environment around a patient and survive there for several days. Environmental contamination is increased when patients have diarrhoea or colonised skin lesions. Prevention of spread is vital and precautions include effective hand hygiene, source isolation, designated toilet facilities, keeping the environment clutter and dust free, and cleaning of equipment and the environment using a chlorine dioxide based disinfectant. Within the community hospitals the most common site for ESBL is in patients’ urine. On receipt of a positive result IPC contact the ward to discuss IPC precautions and treatment with staff. Patients’ hand hygiene is also important and advice is included in the information leaflet. Carbapenemase-producing Enterobacteriaceae (CPE) PHE have published a toolkit for acute trusts to assist them with the early detection, management and control of CPE. A key aspect of the control measures is to take special precautions for patients recently treated in countries known to have high levels of CPE or in UK hospitals with recent clusters or outbreaks of CPE. A patient safety alert was issued by PHE in March 2014 which required all acute Trusts to have implemented the toolkit by 30 June 2014. The IPC team reviewed the advice and included CPE in the revised Multi resistant gram negative policy. The PHE toolkit for the community has subsequently been issued. To date the IPC team is not aware of any in-patients diagnosed with CPE within the community hospitals. Safe Care Shropshire Catheter-associated Urinary Tract Infection (CAUTI) Sub Group SCHT is represented at Safe Care Shropshire and dedicated to the success of the project. The objectives are: To continue to develop and share best practice in relation to the reduction of avoidable harm to patients across all care settings within Shropshire and Telford & Wrekin Infection Prevention Control Annual Report 2014/15 Page 16 of 62 To work together to increase the number of patients across the Local Health Economy who are harm free as defined by the NHS Safety Thermometer point prevalence data collection and through the “sign up to safety” campaign To develop working relationships with other work streams and organisations across the Local Health Economy The aim of the CAUTI sub group is to facilitate the reduction of urethral urinary catheterisations and thus the number of CAUTIs and implement urinary catheter best practices across all health and social care providers in Shropshire and Telford. The group continue to follow a work plan which is central to the group’s work, the process of which was reviewed at the quarterly meetings with the focus on the following key priorities: Catheter assessment – insertion and removal Care and management of urinary catheter including policies and pathway Training Prescribing - catheter products and antibiotics Reinforcement of key policies Patient information SCHT Head of IPC continues to lead the CAUTI sub group and organised the expert speaker and a patient’s perspective of urinary catheters at the ‘Safe Care Shropshire’ conference held in Telford on 2 April 2014 which was to celebrate the progress made with the Safe Care: Harm Free project to reduce harm to patients in hospitals and in their own homes. The CAUTI group expert was Janet Blannin, Independent Nursing Consultant, Continence Care and Clinical Nurse Advisor to 21st Century Catheter Project who talked about her work in preventing CAUTIs. Janet was inspirational and her video showing a urinary catheter in the bladder demonstrated why all staff must think more than twice before inserting a catheter. Janet Blannin delivering her presentation at the Safe Care Shropshire event. The patient’s story about her experience of an indwelling urinary catheter was well received and caused several grimaces from the audience! The CAUTI group was well represented at the event by its members who manned the CAUTI information stand. At the July meeting Dr Brian, Consultant Microbiologist gave a presentation to the group about E.coli bacteraemias (blood stream infections) diagnosed in SaTH laboratory. A very interesting talk which reinforced everyone must avoid the insertion of catheters and to remove them as soon as possible. Also of note was the urgency about responsible use of antibiotics as many of the organisms isolated are resistant to multiple antibiotics. He left the group with the following memorable quote “If you dip a CSU then you’re going to grow a zoo” (CSU being a Catheter Specimen of Urine). A timely reminder that CAUTIs should be only be treated with antibiotics if the patient is symptomatic. The NHS Trust Development Authority (TDA) visit 14-15 May 2014 The NHS TDA provides support, oversight and governance for all NHS Trusts to help deliver high quality and safe services. In a supportive role, the Head of IPC for Midlands and East, Infection Prevention Control Annual Report 2014/15 Page 17 of 62 NHS TDA visited the four community hospitals in May 2014. A positive report was submitted which included three sections: 1. Action Points’ (must do’s). 2. Suggested Action Points. 3. Points for Review. SIPs were developed for all three sections and progress was monitored at IPC Meetings. The few outstanding actions include some Estates issues and policy amendments and will be completed in line with the 2015-16 IPC annual programmes. A number of the issues identified are reoccurring and were previously identified during IPC audits. The main concern is what policies, procedures and support mechanisms are required to be in place to ensure standards are constantly maintained. The Head of IPC for Midlands and East NHS TDA felt sufficiently reassured that a return visit this year was not required. Infection Prevention Control Annual Report 2014/15 Page 18 of 62 Section Four: Progress against 2014/15 Infection Prevention and Control Programme SCHT is legally required to register with the CQC. As a legal requirement of their registration, SCHT must protect patients, workers and others who may be at risk of acquiring an infection. Compliance is judged against the ten criteria laid down in the Health and Social Care Act 2008: Code of Practice on the prevention and control of infections (DH 2010) The 2014/15 IPC work programme is based on this and progress shown under the relevant criterion of the Code of Practice. Criterion 1 – Systems to manage and monitor the prevention and control of infection. These systems use risk assessments and consider how susceptible service users are and any risk that their environment and other users may pose to them. IPC Policy – Arrangements and Responsibilities reviewed to reflect management and reporting structure of SCHT, outlining its collective responsibility for IPC and demonstrating responsibilities are devolved to all staff/groups in the organisation IPC Meeting TOR and membership reviewed Head of IPC has provided regular reports to Quality and Safety Committee including targets, risks and progress against objectives The Annual IPC Report is produced and made available for public viewing via the SCHT website Risks associated with infection have been entered on the Operations Directorate risk register The IPC team continued to identify IPC risks and areas of weakness in policy and practice though audit and surveillance Governance and reporting frameworks in relation to IPC have been strengthened across the Operations Directorate CQC Provider Compliance Assessments completed All infection outbreaks reviewed and service improvements plans developed so that relevant learning was appropriately communicated and acted upon RCA completed for all patients who developed a CDI whilst an in-patient at community hospitals and report tabled at IPC meeting Delivered the IPC Annual Audit Programme - refer to Appendix 1 and Appendix 2 of this report for details of audits undertaken in 2014/15 IPC audit tools adapted in 2011/12 from the Department of Health/ Infection Prevention Society Quality Improvement Tools and DH Saving Lives care bundles have been revised Verification of HCAI audit SIPs to assure completion of the audit cycle In recognition of high IPC standards, Gold Certificates are issued to services with audit compliance scores of 95% and above and Silver certificates are issued to services with compliance score 91-94% The IPC team have developed and delivered IPC training programmes including a one hour update on the core mandatory day for clinical staff Alert organism/alert condition surveillance by the IPC team continues Local peer assessment of hand washing technique for all new staff and yearly for existing staff continued Infection Prevention Control Annual Report 2014/15 Page 19 of 62 Criterion 2 - Provide and maintain a clean and appropriate environment in a managed premises that facilitates the prevention and control of infections This criterion includes cleanliness and hand hygiene, but also includes the fabric of the building and services such as air and water supplies, laundry, waste disposal and decontamination of instruments. Control of MRSA bacteraemia and CDI also come within this criterion. Actions to reduce them have already been described under their specific sections but are briefly mentioned below. General Environment Issues Publicly Available Specification (PAS) 5748:2011, the framework for monitoring cleanliness standards implemented in April 2012 continues In collaboration with the Community Hospital Environment Group (CHEG), Community Hospitals’ cleaning policy and schedules revised CHEG continued to meet to address and support the implementation of environmental issues, share best practice, promote effective use of resources and implement service improvement initiatives including a standardised approach across all four sites Monthly quality reviews are undertaken in community hospitals’ clinical areas and prison healthcare unit; including general cleanliness of areas, and discussions with patients regarding their experiences of the cleanliness of the environment and staff hand hygiene practices Community Hospital cleanliness annual validation audits by IPC team continue Further consideration of in-house community hospitals’ laundry facilities-see section 4. Periodic validation audits continue to be performed by the IPC team to assess the cleanliness in community facilities cleaned by South Staffordshire and Shropshire Foundation Trust (SSSFT) IPC Team continue to advise on refurbishment/redevelopment and new build projects to ensure IPC is adequately considered at all stages Monthly report submitted to the Operations Directorate Estates Divisional meeting by IPC team noting estate issues identified through audit and or during visits PLACE undertaken with focus on service user representation Community Hospital Cleanliness Audit The ward areas and departments within the community hospitals continued to monitor core cleanliness standards using the Publicly Available Specification (PAS) 5748:2011 provided a risk based system for the planning application and measurement of cleanliness. The audits, undertaken jointly by nursing and domestic staff, were carried out bi-monthly. If compliance rates fell or there was recurrence of specific issues then they would be completed more frequently. The IPC team also undertook validation audits to ensure compliance was being reported correctly. The compliance scores were publicly displayed on the IPC notice boards. The compliance scores of the Community Hospital wards are shown in Appendix 3. Formal assessments using the Department of Health (DH) Patient Led Assessment of Care Environments (PLACE) continue. Infection Prevention Control Annual Report 2014/15 Page 20 of 62 The PLACE 2014 visits were undertaken between 3 March to week commencing 26 May, results were made public on 27 August 2014. An overall cleanliness score of 99.17% was awarded to SCHT compared with 98.24% in 2013. Table 7 shows the Community Hospitals’ scores. Table 7: Community Hospitals’ PLACE scores Cleanliness Food Privacy, Dignity and Wellbeing Condition, Appearance and Maintenance Ludlow Hospital 98.11 90.82 76.74 86.30 Bishop’s Castle Hospital 99.57 91.39 95.68 96.61 Whitchurch Hospital 99.87 93.72 83.86 96.92 Bridgnorth Hospital 99.11 95.65 95.28 98.26 Overall SCHT Scores 99.17 92.90 87.89 94.52 Site Name New Builds and Refurbishments The IPC team has been involved in reviewing and supporting refurbishments and new builds within the SCHT. It is paramount that IPC implications for planning, construction and renovation are considered at all stages. In addition the infection risk posed during construction, demolition, refurbishment and planned preventative maintenance works must be considered and action taken to minimise the risk due to environmental organisms e.g. Aspergillus fumigatus by the use of dust screens. The IPC team have advised on the following projects: Ludlow Hospital The IPC team was involved with advising on the refurbishment at Ludlow Hospital and an IPC nurse attended the weekly progress meeting during the refurbishment. IPC Standard Operating Procedures were used to minimise infection risks to patients, staff and visitors. The TDA Head of IPC noted the good seal to keep dust out during her visit to Dinham ward. Stretton ward have now had a hand wash basin installed in the sluice, an issue identified during IPC audits for a number of years and also included in the TDA IPC report. The addition of a ward commode store has addressed the issue of where to store commodes. IPC audits in Minor Injuries Unit and Out Patients Departments identified lack of facilities for disposal of body fluids and decontamination of equipment. The possibility of installation of clean / dirty utility / sluice in Minor Injuries Unit (MIU) has been explored and discussed at Capital and Estates meeting with the Estates advisor involved, surveying area and requirements. Infection Prevention Control Annual Report 2014/15 Page 21 of 62 Mayfair Church Stretton IPC have commented and advised on the plans for the Church Stretton Well Being Centre. Work has not yet commenced. Community Hospitals Clinical Hand Wash Basin Compliance Audit In view of the published Department of Health guidance in March 2012 on “water sources and potential Pseudomonas aeruginosa contamination of taps and water systems”, clinical hand wash basins in community hospitals were audited for compliance against Health Building Note 00-10: Performance requirements of building elements used in healthcare facilities. The report highlighted non-compliant clinical hand wash basins and they were added to SCHT’s risk register and will be upgraded during any future refurbishment. In the interim the Estates advisor is assessing taps and if too eroded by limescale a replacement considered. A build-up of limescale is acknowledged as a problem in Shropshire but the problem identified may be in part due to inadequate cleaning. All domestic staff have therefore been made aware of the correct cleaning procedure and a trial of limescale removal products assessed. A water softener is to be installed at Whitchurch Community Hospital and if successful will be installed in all community hospitals. Laundry The Community Hospital’s onsite laundries were audited by the IPC team in August 2013. Although some urgent issues were addressed, IPC continue to raise concerns around compliance with the DH Choice Framework for Local Policies and Procedures (CFPP) 01-04: Decontamination of linen for health and social care (2013). A Laundry Options Appraisal Report was tabled at October’s IPC meeting followed by the January’s Capital and Estates group who reported it did not clearly reflect requirement nor did it recommend a preferred option. The Deputy Director of Operations is now leading on a proposal to undertake, with financial resource, a market testing exercise to determine whether outsourcing of laundry services will be more beneficial to SCHT. Decontamination The TDA advised that Decontamination Group be convened. Decontamination is now a standing item on the IPC meeting agenda and the Chair is the SCHT Lead for Decontamination. It is acknowledged that the level of risk is low, as the Central Sterilizing Services Department (CSSD) in Telford, operated by SaTH, undertakes most of the decontamination for SCHT including instruments used by the SCHT’s day surgery unit and minor injuries units. The SCHT podiatry service changed to single use instruments in March 2015. Medical devices and associated issues continue to be addressed at Divisional meetings The Decontamination of Reusable Surgical and Dental Instruments policy is available to support all staff involved in the decontamination of these instruments at a local level as well as services which send instruments for reprocessing at the CSSD. Local Decontamination Dental The SCHT dental service is compliant with the ‘essential quality’ requirements contained in the Health Technical Memorandum 01-05 – Decontamination in Primary Care Dental Practices. Plans are in place for each clinic site to progress to ‘best practice’. Castle Foregate (downstairs) and Oswestry Health Centre clinics are now fully compliant with ‘best Infection Prevention Control Annual Report 2014/15 Page 22 of 62 practice’. Work is on-going to consider the best way forward for other clinics to progress to ‘best practice’ which includes the installation of washer disinfectors A quarterly and annual maintenance contract for ultrasonic baths is currently under review by SCHT’s Estates Advisor. Nasendoscopes The Decontamination of Flexible Nasendoscopes Policy is in place to provide guidance on the decontamination of flexible nasendoscopes as undertaken in community hospitals and Advanced Primary Care Services (APCS). A specific disinfectant wipe system is used by all SCHT locations undertaking nasendoscopy as validated in the national guidance Choice Framework for local Policy and Procedures (CFPP) 01-06 on the Decontamination of Flexible Endoscopes (June 12). The manufacturers of the Tristel wipe system provide free-of-charge training to staff required to use this method of decontamination. In response to IPC audits of the Ear Nose and Throat (ENT) clinics, a storage cabinet and trolley storage system have been purchased by Whitchurch and Bridgnorth Community Hospitals respectively to provide appropriate storage of the nasendoscopes as recommended by the manufacturers. Endoscopes A policy for the decontamination of flexible endoscopes is in place to support safe practices for the use of an automated endoscope reprocessor (AER) for washing and disinfecting these instruments. It includes national guidance on the testing for microbiological quality of the final rinse water from the AER. The IPC team is notified of results and follow up any abnormal ones. Validation of AERs is a national requirement. PuriCore have continued to service the unit in accordance with the testing standards. Automated Endoscopy Reprocessor (AER) at Bridgnorth Community Hospital Full validation and water testing has continued to be undertaken on the AER and the unit staff have received appropriate training. Anomalies with the final rinse water test results were noted several times in the summer and Puricore attended to service and change filters. There appeared to be some connection with the raised colony forming unit (cfu) and mains water replacement works in the vicinity of the hospital. The Estates advisor has written to all utility companies asking for notification of any work due to be undertaken in close proximity to SCHT premises. A specialised storage cabinet with a high-efficiency particulate air (HEPA) filter is used to store the disinfected endoscopes for up to 31 days and prevent contamination rendering them safe for immediate use and enhances efficiency. Water Safety Group The Head of IPC for the TDA advised that SCHT should have a water safety group. Following discussions, a new joint SSSFT and SCHT group has been formed. SCHT are represented by Estates, Hotel Services and IPC. The TOR has been developed and the meetings are bi-monthly at present. It is intended that the Group will monitor risk Infection Prevention Control Annual Report 2014/15 Page 23 of 62 assessments especially around Legionella, flushing regimens, annual disinfection and AERs. The water safety group report to the IPC meeting as a standing agenda item. Criterion 3 - Provide suitable accurate information on infections to service users and their visitors Head of IPC produced an annual report covering the organisation’s approach to prevention and control of infections for publication on the SCHT website Hand hygiene included in patient/visitor information leaflets Strategically placed hand hygiene products available for use with information on how to use Continued to encourage patient and public involvement in hand hygiene and cleanliness campaigns and services’ Quality Review process, satisfaction surveys and PLACE inspections In conjunction with the SCHT Communication Team key IPC messages were promoted through internal and external media communications including the SCHT website, in particular prior to and during ‘Norovirus season’ Large display boards were erected at each of the community hospitals to raise public awareness during the months when Norovirus is prevalent in the community IPC information boards designated in all community hospitals display IPC data and audit results Polices related to specific organisms and care pathways remind staff of the need to give affected patients and relatives leaflets about the infection IPC page on the SCHT website further developed and now includes monthly HCAI data Quarterly IPC newsletter produced and published in Inform as aide memoire and resource for clinical staff Information leaflets revised and placed on the SCHT website informing patient/public on specific infections and hygiene measure they can adopt to reduce the risk of infection The IPC team and other members of staff continue to respond to ad hoc requests for information related to IPC under the Freedom of Information Act Criterion 4 - Provide suitable accurate information on infections in a timely fashion to any person concerned with providing further support or nursing / medical care IPC requirements are included in the health economy transfer/discharge form Quarterly IPC newsletter produced and published in Inform as aide memoire and resource for clinical staff IPC team share infection rates and outbreak information with appropriate services based upon local, regional and national surveillance IPC page on the SCHT website MRSA bacteraemia and CDI data published on the SCHT website Alert organism surveillance by the IPC team IPC policies available IPC information boards sited on all community hospital wards and MIUs Monthly MRSA screening compliance shared with CSMs Infection Prevention Control Annual Report 2014/15 Page 24 of 62 Criterion 5 - Ensure that people who have or develop an infection are identified promptly and receive the appropriate treatment and care to reduce the risk of passing on the infection to other people Arrangements to prevent and control infection come within this criterion and should be such as to demonstrate that responsibility for IPC is effectively devolved to all groups involved with delivering care. IPC Arrangements and Responsibilities Policy reflects the management and reporting structure of SCHT outlining its collective responsibility for IPC and demonstrating responsibilities are disseminated to all staff/groups in the organisation Responsibilities of groups and staff included in IPC policies Support provided by IPC team included visits and daily telephone contact Continued to develop Link Staff and supporting of their role Link Staff Roles and Responsibilities revised and updated Continued to audit compliance with IPC polices and care pathways IPC team access to SaTH Laboratory IT systems allowed enhanced alert organism surveillance IPC team reported outbreaks and incidents of infection to our commissioners, PHE and the TDA IPC team emailed all organisations involved with health and social care to alert them of outbreaks of infection declared within SCHT IPC received notification of outbreaks of infection within the local health economy IPC specific organism e.g. MRSA, CDI policies available Community antibiotic policy available to all prescribers PIR undertaken on all MRSA bacteraemias and a RCA on CDI involving community hospitals or community services involved with the patient’s care Use of SIGHT mnemonic Issued cards with SIGHT mnemonic to ward staff to use as an aide memoire Ward staff advised to use isolation audit tool as a checklist to ensure compliance with isolation policy Awareness of the National Ward Sepsis Screening and adaption of action tool for SCHT Ebola Following advice issued by NHS England in response to the outbreak of Ebola virus, the IPC team worked in collaboration with the Health Emergency Management Specialist and MIU lead to ensure that in the event of a patient presenting with symptoms, staff were competent in the management prior to transfer to the acute hospital. Utilising national guidance, an algorithm for viral haemorrhagic fevers (VHF) and contents for decontamination boxes (containing PPE and cleaning products etc.) were developed and made available in all MIUs. The PHE Ebola poster to inform the public regarding Ebola was displayed in MIU entrances. A priority for MIU staff was to ensure they were fit tested for respiratory masks; therefore several staff received the fit test training and were then able to fit test staff locally. Staff were also made aware of the correct processes for the application and removal of PPE. Infection Prevention Control Annual Report 2014/15 Page 25 of 62 Criterion 6 - Ensure that all staff and those employed to provide care in all settings are fully involved in the process of preventing and controlling infection Facilitated by the LHE IPC group, continued to work with NHS providers to reduce all avoidable infections including MRSA bacteraemia and Clostridium difficile Continued to address the agreed maintenance Clostridium difficile plan through the LHE group Compliance with MRSA screening policy screening audited monthly As appropriate, joint investigations and reviews held between SCHT and the acute Trust on cases of MRSA bacteraemia and CDI Quarterly IPC Link Staff updates allowed information to be disseminated from the IPC team back to the individual services Annual Study Day for IPC Link Staff focused on blood borne viruses Outbreak masterclass for on-call senior managers and directors Outbreak pack available to assist staff with managing outbreaks. This included door notices, posters, monitoring forms, checklist which was emailed by IPC nurse to the member of staff on notification of outbreak IPC team continued to support SCHT to take forward national initiatives which have an IPC element including the Safe Care: Harm Free Project IPC team supported the development of SCHT clinical policies/procedures IPC Always Events Poster displayed in all clinical services/areas IPC pack developed for and distributed to medical staff who work in community hospitals New “clean safe hands” poster featuring Shrewsbury Town’s goalkeeper developed and distributed to all SCHT premises Infection Prevention Control Annual Report 2014/15 Page 26 of 62 Criterion 7 - Provide or secure adequate isolation facilities Due to the nature of the patient population, it can at times be difficult to isolate patients to minimise the spread of infection. The Isolation policy includes an Isolation Risk Assessment Tool which allows staff to consider individual requirements for isolation to ensure patients are managed on a case by case basis. IPC Isolation policy in place to support staff Audits of compliance with isolation policy undertaken in community hospitals by IPC team when incidents of infection and outbreaks occurred Risk assessments performed by ward staff with support from the IPC team when insufficient isolation facilities were available to meet demand Cohort approach taken as necessary within community hospitals during outbreaks of diarrhoea and vomiting IPC training programmes include Clostridium difficile prevention, management of individual cases including isolation practices Work completed in the summer of 2014 to provide additional en suite facilities at Ludlow Community Hospital to improve patient dignity and aid cohort nursing during outbreaks All episodes where staff are unable to isolate patients are reported to Risk Management via Datix commenced September 2014 Criterion 8 - Secure adequate access to laboratory support as appropriate Laboratory services provided by SaTH The microbiology laboratory at SaTH compliant with the standards required for accreditation by Clinical Pathology Accreditation (UK) Ltd. Continuation of seven day rapid testing for Clostridium difficile and use of typing to search for clusters and linked cases Continuation of local test for Norovirus to speed up diagnosis and outbreak management of patients with infection Adequate resources available in laboratory for MRSA screening in line with national guidance Mandatory surveillance also included MSSA and E.coli bacteraemia infections Consultant Microbiologist at SaTH is SCHT’s IPC Doctor Monthly Consultant Microbiologist and IPC nurses meetings Medical microbiology support provided by SaTH 24 hours a day 365 days a year Criterion 9 - Have and adhere to policies, designed for the individual's care and provider organisations that will help to prevent and control infections Rolling programme of policy review continues Published evidence reviewed whenever policies were developed or reviewed on publication of new national guidance to ensure they reflect up to date, evidence based, best practice national guidance New policies developed as need identified Community Hospital pharmacists and technicians review drug charts In collaboration with Medicines Management team commenced work to implement the relevant recommendations of the national 5-year strategy for antimicrobial resistance issued by the Department of Health in March 2015 Infection Prevention Control Annual Report 2014/15 Page 27 of 62 The following polices were developed or reviewed in 2014/15: Policies Reviewed: Aseptic Technique Hand Hygiene Infection Prevention and Control Arrangements and Responsibilities Influenza IPC in the Built Environment Management of Norovirus and other GI Infections Multi resistant Gram Negative Bacteria Standard Precautions including surgical hand scrub, gloving, gowning New policies developed Management of Group A Streptococcus Compliance with policies was audited locally through the hand hygiene, cleanliness and IPC audit tools and specific competency tools and peer assessments. Specific audits undertaken by the IPC team as part of their annual programme, clinical incident reporting and root cause analysis of infections including debrief meetings were also used to monitor compliance. Community hospital pharmacists reviewed antibiotic prescriptions and advised in accordance with local antibiotic policy. Antibiotic audits were undertaken by pharmacists. The IPC team has also contributed to the development/review of the following Estates policies: Waste Legionella – Include control of pseudomonas and management of drinkable and non-drinkable water supplies Pest control Contractors’ Site Access Mobile Phone Use Assistance Dogs The IPC team are members of the Clinical Policies Group which reviews and approves all clinical policies. As members it ensures accurate and relevant IPC advice is included in all clinical policies. Medicines Management Report Community Hospitals: The medicines management clinical team have undertaken antibiotic audits on a regular basis to support the antibiotic stewardship agenda. Elements measured included: Choice of antibiotic as compared to the formulary recommendation. Off formulary antibiotics were challenged with the prescriber. Exceptions included antibiotic recommendations made by the SaTH microbiologists where these were documented in the patients’ notes. Duration of the antibiotic course Allergy status Challenge to prescribers where several courses of antibiotics had been prescribed Infection Prevention Control Annual Report 2014/15 Page 28 of 62 Medical staff have been encouraged to record the indication and duration of the antibiotic on the drug chart and the new drug chart has facilitated this. The main reminder we have to give to prescribing medical staff is around defining the length of the course. Antibiotic guidance is available on each ward. District Nursing: Non-medical prescribing by community nurses is monitored via ePACT data. Where higher risk antibiotics (cephalexin, co-amoxiclav, 4-quinolones) appear on the data being scrutinised, the prescriber is required to provide assurance that the prescription matches the community antibiotics guidance. Patient Group Directions: Some antibiotics are available to patients via Patient Group Direction e.g. in Minor Injury Units. As part of the development process, consultant microbiologist advice and approval is sought. Dental emergencies: Some to take out (TTO) packs of a restricted range of antibiotics have been made available to the dental service where supply at the point of consultation is in the best interests of the patient e.g. out of hours, and only initiated by a dentist. November 18th is Antibiotic Awareness day. There is currently a particular focus on the appropriate use of antibiotics because of the increasing resistance patterns seen in the community and in hospitals. The Antibiotic Awareness day in 2014 was marked by the display of information at the community hospitals and at William Farr House about the judicious use of antibiotics. The information was aimed at both staff and the general public. The display materials comprised information, quizzes and Frequently Asked Questions. The materials also invited people to sign up to become antibiotic champions and directed people to the central website. Similar information was provided by CCG colleagues to GP practices for display in the surgeries. Medicine Management report written by: Rita O’Brien. Criterion 10 - Ensure, so far as reasonably practicable, that care workers are free of and are protected from exposure to infections that can be caught at work and that all staff are suitably educated in the prevention and control of infection associated with the provision of health and social care Staff Health The IPC team continued to work with the Occupational Health Service (OHS) to ensure that staff are protected from infection and did not pose a risk to others, including patients, from their own infections. The use of hand moisturisers has been encouraged to protect care workers’ hands from the effects of frequent hand decontamination. Influenza The OHS led the influenza campaign supported by IPC team flu champions and other flu champions dispersed across SCHT. Following an evaluation of last year’s campaign, the planning and promotion for this year was commenced earlier, the number of occupational health influenza sessions was increased and these were on a drop-in rather than an appointment basis. All staff were offered and actively encouraged to have the seasonal influenza vaccination and the communications team assisted by promoting key messages. Attendance by OHS at Infection Prevention Control Annual Report 2014/15 Page 29 of 62 various meetings, corporate induction, staff awards and training sessions was also undertaken and a series of health and wellbeing events held during the campaign also gave staff the opportunity to have their influenza vaccination along with a mini lifestyle check including blood pressure and cholesterol tests. The IPC Team flu champions also gave staff the opportunity to receive vaccination at the Link Staff sessions and through their attendance at meetings and visits. For the year 2014-15, 67.2% of SCHT frontline staff were vaccinated against influenza which is an increase on last year’s uptake of 64.8% and higher than the national average of 54.9%. SCHT was in the top three performing NHS Community Trusts behind only our colleagues in the Wirral and Leeds. This is testament to all those who worked on the campaign resulting in an increased awareness and uptake despite winter pressures and challenging times. An MRSA for Staff screening policy is available to help support the member of staff and their manager to ensure that they do not put others at risk of acquiring the organism. In addition to the MRSA policy a number of OHS policies, including staff immunisation policy, are available. The IPC policies Prevention and Management of Needlestick Injuries including inoculation incidents and Blood Borne Viruses (includes safe sharps handling), Standard Precautions policy and the Hand Hygiene policy all support staff health. The IPC nurses reviewed all infection prevention and control incidents including sharps injuries and followed up with OHS to ensure the policy had been followed. In addition all IPC incidents were reported to and monitored bi-monthly at the IPC Meeting. Sharps safety As previously reported the EU Directive 2010/32/EU was to be implemented by May 2013. This directive required all healthcare providers to introduce further protection for health care staff exposed to the risk of sharps injuries, and actions. The Head of IPC at the TDA in May 2014 raised concerns that safety engineered needle devices (SENDS) were not available and or implemented in many areas. Further work with Shropshire Healthcare Procurement Service, raising awareness of SENDS at IPC training sessions and through audit has been undertaken. Occasionally it is inappropriate to use a SENDS device in which case a formal risk assessment is undertaken and recorded on the Datix risk register. Progress with the implementation of SENDS continues to be monitored at the bi-monthly IPC meetings. Figure 4 below shows SCHT inoculation incidents for the past two years. Encouragingly in 2014-15 there has been an 18% reduction in the number of injuries reported with 23 injuries compared with 28 reported in 2013-14. Infection Prevention Control Annual Report 2014/15 Page 30 of 62 Figure 4: SCHT Inoculation incidents reported April 2013-March 2015 Education As an organisation, SCHT is committed to the principle that IPC is the responsibility of all, facilitated through a programme of education, both formal and informal, throughout the organisation. One of the principal functions of the IPC team is to inform all clinical staff of the standards expected of them. The team continued to contribute to SCHT’s induction and core mandatory training days for clinical staff and provided additional ad hoc tailored training to staff to ensure that IPC remained a high priority for all. Induction Programme The IPC team participated in the Induction Programmes for all new staff, both clinical and non-clinical, which 185 staff attended. The objective of the team’s participation was to inform staff how they could contact the IPC team, access IPC policies and raise awareness of IPC national guidelines and local initiatives. It also provided an opportunity to highlight main IPC principles and to raise awareness of the responsibility and role of IPC for all members of SCHT. A local IPC induction is facilitated by the new member of clinical staff’s manager and includes the hand washing assessment to be undertaken within the first week. Mandatory Training IPC face to face mandatory training for all clinical staff continued to be offered via SCHT’s Organisational Development (OD) team and out of a possible 1,137staff, 1086 staff (95.5%) attended the core days for clinical staff. The one hour of training focused on Standard IPC precautions, multi-resistant organisms, newly published national guidance or changes to current practices and policies. The National IPC e-learning training package was made available to all staff via OD for nonclinical staff to complete every three years and was completed by 182 staff out of a possible 395 staff (46%). Infection Prevention Control Annual Report 2014/15 Page 31 of 62 Additional Training The IPC team continued to expand the provision of IPC training to as many groups as possible including: IPC team participated on the six “administration of intravenous medication via peripheral vascular access device” study days attended by 44 SCHT staff in total. Content of the training included sources of intravenous infections, evidence-based practice related to insertion and on-going actions to reduce the risks of infection associated with peripheral vascular devices IPC team delivered IPC educational session covering standard precautions and outbreak management to 10 HCAs attending a HCA Development day run by Catherine Chaplin, Clinical Educator IPC team delivered a Hand Hygiene educational session to 34 Speech and language therapists at their study day. Bespoke Training In addition to the above the IPC team has delivered bespoke training to 121 staff of many different disciplines as shown in table 8 below. Bespoke face-to-face sessions were also arranged by the IPC team where need identified e.g. medical, domestic and portering staff Attendees names were reported to OD for recording. Infection Prevention Control Annual Report 2014/15 Page 32 of 62 Table 8: Bespoke IPC training Porters Porters GPs Volunteers GPs GPs Outbreak Management for senior managers Domestics Domestics Volunteers Domestics IPC for Ward Clerks Volunteers and League of Friends Total 08/04/2014 09/05/2014 25/06/2014 01/07/2014 21/07/2014 19/09/2014 19/11/2014 12/12/2014 22/01/2015 24/02/2015 24/02/2015 26/02/2015 23/03/2015 Ludlow Whitchurch Ludlow William Farr House Bridgnorth Whitchurch William Farr House Whitchurch Bridgnorth William Farr House Ludlow Bridgnorth Bridgnorth 3 3 8 12 7 5 10 8 10 8 17 2 28 121 The IPC Outbreak Management Master Class was attended by Senior Managers and Directors with the aim of the session to provide information to assist when dealing out of hours with infective outbreaks in SCHT community hospitals. The evaluation was very positive and attendees found the information relevant and informative. Bespoke IPC training concentrating on hand hygiene and general IPC advice concerning visiting and movement within the community hospitals and volunteer illness was delivered to volunteers Antibiotic Awareness In conjunction with Medicines Management the IPC team promoted the annual global antibiotic awareness day on 18 November 2014 with a display board erected in William Farr House during November. Information leaflets appropriate to healthcare professionals as well as to patients and visitors were made available. The aim of this initiative is to promote key messages and raise awareness of antibiotic resistance which is driven by overusing antibiotics and prescribing them inappropriately. It is important that antibiotics are used correctly to reduce the risk of antibiotic resistance and make sure these life-saving medicines remain effective now and in the future. Norovirus Roadshows The IPC team held a Norovirus roadshow in all four community hospitals during November. The information board and portable hand wash basin was particularly aimed at informing visitors of the signs and symptoms of Norovirus and the reasons why they should not visit if unwell. The portable hand washing basin was well used at the entrances to the wards; the feasibility of permanent hand wash basins at the entrances to all community hospital wards will be assessed by Estates. Radio Shropshire presenter Genevieve Tudor interviewed Head of IPC Rachael Allen and IPC nurse Lizzie Watkins when the roadshow was at Bridgnorth Community Hospital. The interview provided information about Norovirus and hand hygiene and Genevieve Tudor participated in a hand hygiene demonstration using the ‘GloBox’. She was wearing numerous rings which provided the ideal opportunity to discuss why ‘Bare below the elbow’ is part of the uniform policy for clinical staff. Infection Prevention Control Annual Report 2014/15 Page 33 of 62 The SCHT Board also invited the roadshow to attend their November meeting and a number of the Directors and Non-Executive directors took the opportunity to use the portable hand wash basin and, using the ‘GloBox’, could see how well they washed their hands. IPC nurse Lizzie Watkins, Head of IPC Rachael Allen and Radio Shropshire’s Genevieve Tudor with the portable hand wash basin at Bridgnorth’s Norovirus Roadshow Dr Ganesh Medical Director tries the portable hand wash basin in a non-clinical setting The Norovirus ‘roadshow’ Infection Prevention Control Annual Report 2014/15 Page 34 of 62 Infection Prevention and Control Link Staff Link Staff are critical in the delivery of IPC within all services. Link Staff meetings are held quarterly and provide opportunities for networking, emphasising the service provision throughout SCHT and between services. This continues to be an extremely effective way of distributing information and generates valuable question and answer sessions. All link meetings include information on national infection targets, RCA/PIR feedback, outbreak summary, safety notices, incident reports, new or revised IPC policies and discussion of IPC audits findings. All are important elements to be taken back to clinical areas and have the potential to reduce infections by promoting optimal practice. The link person disseminates the information to their area of work usually as a standing item Congratulations to Ludlow Minor Injuries Unit, who won the competition on team meeting agendas. for the most informative Norovirus IPC board The Link Staff in community hospitals manage an IPC board in their area where possible to display a different theme each quarter. Link Staff were asked to focus on norovirus for the period 1 January to 31 March. Link Staff Study Day The third annual study day for IPC Link Staff was held on 12 February 2015. Following the welcome and overview of the Director of IPC’s role by Steve Gregory, the day focused on blood borne viruses (BBV) and included sessions from a Consultant Microbiologist, a representative from the Terrence Higgins Trust and PHE. The quiz was won by Rebecca Barton, Clinical Practice Educator. The day was well attended by Link Staff across SCHT services and received excellent feedback. The IPC team intends to build on the success of this event and are already planning next year’s study day. Delegates participating in activities at the Link Staff Study Day During IPC audit The IPC team use audit visits as an educational opportunity to reinforce good practice and make suggestions how practices can be adapted and standards improved. This was consolidated through the audit report subsequently sent by the IPC nurse and in the development and return of a SIP where the score is less than 100%. Infection Prevention Control Annual Report 2014/15 Page 35 of 62 Informal Education/Awareness The IPC team continued to raise awareness of IPC issues using a variety of mediums including regular visits to community hospitals, local road-shows and service-specific clinical governance events. Posters and information leaflets were used to promote good IPC practices and advice given accordingly, including ad hoc telephone advice to all services within SCHT. Check to Protect This initiative has been developed to replace Essential Steps. Check to Protect is for clinical staff and comprises of a set of eight assessment tools, including Aseptic Technique, Catheter Care, Disposal of Sharps and PPE. It is designed to be easy to use and a straightforward peer assessment tool. Intended to be used by staff to assess their peers annually, it ensures safe, effective standards of IPC are being met and maintained within all clinical services and also identifies areas for improvement. Check to Protect for Clinical staff was launched in September 2014 as part of the Health Care Assistants’ Education Programme, with support from SCHT’s Clinical Educator and is in the process of being disseminated for use by all clinical staff. IPC Team Development The IPC nurses continue to be supported to increase their knowledge, understanding and skills to assist deliver improved quality of care for our patients by relieving the burden of avoidable healthcare associated infections. This included attendance by an IPC nurse at the Annual Infection Prevention Society (IPS) conference in Glasgow in September 2014. Among the themes addressed were the Emergence of New Pathogens including CPEs, Ebola in Africa and how IPC nurses can make care safer and combat the overuse of antibiotics. Following evidence presented at conference, Community Hospitals are advised if appropriate to isolate all patients with CDI for the duration of their stay not just their period of active infection. The Head of IPC attended an IPS Implementation Learning Laboratories Event in Birmingham in December and an IPC nurse attended a repeat session in February. The event was aimed at IPC practitioners interested in best practice and focused on helping to understand and overcome the barriers to implementing infection prevention guidance by providing a package of resources and ongoing support from IPS and colleagues. The Head of IPC attended the West Midlands PHE Carbapenemase Toolkit Launch in May 2014 which provided the opportunity to learn more about this highly resistant organism from hospital staff who have experience of managing patients with CPE. The LHE IPC nurses’ forum quarterly meetings have continued to support the implementation of national and local IPC priorities across Shropshire and Telford and provide an arena to identify and address risks in relation to IPC and ensure an integrated approach is taken to develop good practice across organisational boundaries. The monthly IPC team meeting with the consultant microbiologist is viewed as another educational opportunity for the IPC nurses as is IPC nurses meeting with feedback from meetings and study days a standing item on the agenda again to ensure information is shared. The team are members of IPS and the Healthcare Infection Society and receive weekly emails with up to date National and International IPC guidance/alerts/memo’s etc. Monthly Infection Prevention Control Annual Report 2014/15 Page 36 of 62 journals are received which are a valuable medium for acquiring evidence-based up to date research and ensures best practice is used when writing policies. Within the team the monthly journal club has continued where a peer reviewed journal article is discussed. The IPC team have maintained compliance with the mandatory training programme. Infection Prevention Control Annual Report 2014/15 Page 37 of 62 Section Five: Hand Hygiene Effective and timely hand decontamination is acknowledged as the most important way of preventing and controlling infections. The IPC team continued its concerted efforts to ensure that hand hygiene compliance remained a high priority. Training on the importance of hand hygiene, being ‘bare below the elbow’ and the WHO ‘5 moments for hand hygiene’, was provided locally to new clinical staff on induction and was reinforced by members of the IPC team at all IPC training events, during clinical visits and whilst auditing. Hand Washing Assessments In 2012 a local peer assessment of hand washing technique was introduced and has continued since for all new staff within one week of commencement of employment, with ongoing yearly assessment for existing staff. Assessments were undertaken by trained, competent assessors within the area or department. Failed assessments were reported to the ward manager/team leader and repeated within the week. In the event of a second failed assessment it would be reported to the IPC team. Reassuringly, there were no such reports. A ‘Healthy Hands’ educational leaflet was given to the member of staff at the time of the assessment and the assessment record was retained by the service manager and a copy given to the staff member. Hand washing assessments are included in clinical areas’ reports to the IPC Meeting. A number of hand hygiene ‘train the assessor’ sessions were delivered by the IPC team ad hoc when identified that it was required. The support was important to the clinical staff in their role as an assessor, as it is it vital to ensure that all assessments are consistent and subject to the same protocol and standard. Hand Hygiene Observational Audit The IPC Link Staff continued to undertake monthly hand hygiene observational audits in all four community hospitals wards and ensured the compliance scores were displayed on the IPC notice boards. If compliance fell below 95%, weekly audits were required until 95% compliance was achieved. Hand hygiene verification observations were undertaken by the IPC team to ensure compliance was reported correctly and assisted poorly performing areas by reinforcing hand hygiene messages with ad hoc training. The observations identified the staff group to enable feedback to be specific to the group who were not complying and to assist IPC to focus training where required. This year, agency staff were included as a separate category in the hand hygiene audit and this has enabled ward managers to discuss poor compliance direct with the agency. Results of the audits were monitored by the CSMs and reported to the IPC Meeting and the Quality and Safety Committee. Hand hygiene audit results undertaken by the link staff are recorded in Table 9. Those undertaken by IPC nurses are shown in Table 10. Infection Prevention Control Annual Report 2014/15 Page 38 of 62 Table 9: Community Hospital Hand Hygiene Audits undertaken by Link Staff 2014/15 Apr 14 May 14 June 14 July 14 Aug 14 Sept 14 100%/ 86% Oct 14 Nov 14 Dec 14 Jan 15 Feb 15 Mar 15 Bishops 100% 100% 100% 100% 100% *** *** *** *** *** Castle Bridgnorth 77%/ 90% 80%* ** 100 90 100% Female 76%* 100% 100% 100% 100% Bridgnorth 77%/ 90% 60%* ** 100 90 96% Male 76%* Ludlow **** **** **** **** **** **** **** **** **** 100% 100% Dinham Ludlow **** **** **** **** **** **** 100% 100% **** **** 100% Stretton Whitchurch Not 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% Team 1 done Whitchurch 100%/ 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% Team 2 97% *Redone until 100% **A gap in Sept was when both infection control nurses were off for long term sickness and leave. This has been addressed and senior staff will undertake if the situation arises again. ***Data not available – both link staff left and have not yet been replaced. ****Data not available *** 96% 96% 100% 100% 100% 100% Table 10: Community Hospital Hand Hygiene Audits undertaken by IPC nurse 2014/15 Apr 14 Bishops Castle Bridgnorth Female Bridgnorth Male Ludlow Dinham Ludlow Stretton Whitchurch Team 1 Whitchurch Team 2 May 14 June 14 July 14 71% Aug 14 Sept 14 89% Oct 14 Nov 14 Dec 14 Jan 15 Feb 15 100% 80% 60% 86% 100% 100% 80% 80% 100% 100% 100% 100% N/A 100% 100% N/A 100% 100% 100% Mar 15 100% 88% 90% 100% 100% 100% 90% Performing regular observational hand hygiene audits within community based services has proved a significant challenge; however the IPC Link Staff have used the hand washing assessment to ensure staff are compliant with the hand washing technique. Bare Below the Elbows SCHT’s uniform policy and dress code promotes the bare below the elbow protocol in that to ensure effective hand hygiene while working clinically, all staff MUST be ‘bare below the elbow’. This message continues to be reinforced through IPC mandatory and bespoke training and is monitored during IPC audits. Infection Prevention Control Annual Report 2014/15 Page 39 of 62 Section Six: 2014/15 Infection Prevention and Control Team Audit Programme As in previous years audit continued to be an important activity that assists the monitoring and improvement of practice. In total 82 audits were undertaken in the community hospitals and 25 in community services. The objectives of the audits were to inform services of their level of compliance to national IPC standards, local policies and procedures and allow improvements to be made based upon the findings. It also identified target areas for training. A rolling programme of IPC audit was developed and implemented in clinical and non-clinical areas, using the adapted DH/IPS audit tools. A baseline audit was undertaken when new services were developed or relocated. The results were used to determine the frequency services will be re-audited. See Appendices 1 and 2 for the audit programme and compliance scores for community hospital audits and community services audits. Overall Score and Compliance Rating For the purpose of these audits the aim is for a 100% compliance score. A SIP is generated for scores of less than 100%. Reporting and Monitoring At the time of audit the IPC nurse verbally reported any areas of concern and of good practice to the member of staff accompanying them and or the person in charge at the time of the audit. A written summary report and detailed recommendations in the form of a SIP was developed by the IPC nurse within two weeks and shared with the relevant clinical area and manager for action. Support from the IPC team was offered to implement changes required to improve practice. Services were requested to return the completed SIP within two weeks to the IPC nurse, detailing the actions taken and a timescale for completing any outstanding actions. Progress was monitored locally and reported to the IPC meeting. Summary of audit findings and actions taken: The compliance scores remain variable, confirming that further work must continue to improve and sustain IPC standards. However, it should be recognised that some areas did achieve 100% compliance and generally improvements made in all areas on subsequent visits have been noted. Staff have been receptive to discussion and comment, and the SIP completed and findings addressed. The standard most frequent to be found non-compliant was the hand washbasins which had a buildup of limescale and or were not in a good state of repair. A separate audit covering these was undertaken and a report submitted to the December IPC Meeting and all noncompliant areas added to the risk register. An in-depth analysis of the community hospitals’ Prevention of HCAI audit findings is shown in Appendix 4. Self-audits/checklists IPC have encouraged the use of the audit/checklist by ward staff as an aide memoire when commencing isolation and on urinary catheter insertion etc. The intention is that any issues identified are addressed immediately to ensure safety for the individual patient and other patients and staff. For example if there is no single patient use blood pressure cuff in source Infection Prevention Control Annual Report 2014/15 Page 40 of 62 isolation one is provided there and then. See Appendix 5 for details of self-audits undertaken by ward staff. Self-audits/checklists undertaken: Hand Hygiene Observations Urinary Catheter Isolation Practices - at time of isolation Vascular Access Device - at time of insertion Enteral Feeding Infection Prevention Control Annual Report 2014/15 Page 41 of 62 Section Seven: Looking Forward to 2015/16 An Overview of Infection Prevention and Control Programme 2015/16 This section gives an oversight of the work planned to prevent and control infections in 2015/16 and to achieve external targets and comply with the Code of Practice on the prevention and control of infections. It is designed to reflect SCHT’s Quality Strategy for 2015-2018 to deliver care that is clinically effective; care that is safe; and care that provides a positive experience for patients as possible. The programme is also developed to deliver the objectives in the newly agreed LHE IPC 2015-2018 Strategy which will provide a system wide innovative vision for infection prevention and control for the next three years. The key aims in 2015/16 will be to build on the work that has been done in previous years to prevent HCAIs, and improve the lives of the people who come into contact with SCHT services. Patient safety is at the heart of IPC, and to ensure our work is sustainable, SCHT promotes that every member of staff takes responsibility for IPC in order that that no person is harmed by a preventable infection. Our focus will be to: Strengthen governance around estates, decontamination and water quality Achieve zero tolerance for MRSA bacteraemia Achieve local reduction target for CDIs Support wards to achieve a compliance rate of over 95% for MRSA screening Manage and control antibiotic-resistant bacterial infections Review IPC, clinical and estates polices in line with review dates, revised national guidance and as a result of incidents and RCA/PIR Deliver IPC team 2015/16 Audit Programme. See Appendix 6 Continue to review the audit programme regularly to ensure that the audit is meaningful and helpful in generating best practice Enhance local monitoring and self-checklists of IPC practice using adapted tools Continue to promote the Check to Protect IPC peer assessment and competencies Challenge existing assurance mechanisms and validate self-assessment and provide local support to areas of poor performance Continue to develop and support the role of the IPC Link Staff by planning an annual IPC study day Develop and review IPC patient/public information leaflets in line with review dates or revised national guidance Deliver IPC training on Core Mandatory Training and Induction days Deliver bespoke IPC training as need identified Support SCHT to deliver the Safe Care Shropshire Project in relation to CAUTIs Maintain high standards of hand hygiene Improve the monitoring of hand hygiene compliance Support SCHT to comply with European Directive 2010/32/EU sharps safety devices In collaboration with SCHT Medicines Management, continue to monitor antibiotic prescribing in community hospitals and implement the national 5-year strategy for antimicrobial resistance In collaboration with SaTH, review the possibility of a commercial surveillance system that facilitates more effective identification / prevention of infections Undertake SSI surveillance following hand surgery at Bridgnorth Day Surgery Unit Washable computer keyboards to be implemented in higher risk clinical areas Continue to provide telephone support to all SCHT Staff Infection Prevention Control Annual Report 2014/15 Page 42 of 62 Timely review and follow up microbiology laboratory reports 2015/16 Local Infection Prevention and Control Objectives as agreed with Commissioners 2015/16 Infection Targets The local infection targets agreed for 2015/16 are: MRSA bacteraemia – Zero tolerance Post 72 hrs Clostridium difficile infection – no more than two cases diagnosed on the third day or later of an admission to one of the four community hospitals (where the day of admission is day one) 2015/16 IPC Key Performance Indicator (KPI) In line with SaTH, SCHT continue to undertake MRSA screening for all relevant elective and emergency admissions. MRSA screening – Threshold of 97% (increased from 95%) of all admissions to community hospitals Other KPI’s Compliance with Trust hand hygiene policy - Threshold of 95% Compliance with IPC checklists (adapted from the high impact interventions) Threshold of 95% Compliance with national environmental and equipment cleaning standards (Publicly Available Specification (PAS) 5748:2011) /and local cleaning protocols.Threshold of 95% Infection Prevention Control Annual Report 2014/15 Page 43 of 62 Section Eight: Glossary of Terms AER Automated Endoscopy Reprocessor. A specialised machine for washing and disinfecting endoscopes APCS Advanced Primary Care Services Bacteraemia A bloodstream infection ENT Ear Nose and Throat Care Quality Commission (CQC) The CQC is the independent regulator of health and social care in England. It regulates health and adult social care provided by the NHS, local authorities, private companies and voluntary organisations. CAUTI Catheter Associated Urinary Tract Infection CCGs SCCCG and TWCCG Clinical Commissioning Group. The two commissioning organisations in Shropshire and Telford & Wrekin are Shropshire Clinical Commissioning Group and Telford and Wrekin Clinical Commissioning Group. CDI Clostridium difficile infection. Clostridium difficile is a bacterium which lives harmlessly in the intestines of many people. Clostridium difficile infection most commonly occurs in people who have recently had a course of antibiotics. Symptoms can range from mild diarrhoea to a lifethreatening inflammation of the bowel. CHEG Community Hospital Environment Group CQC Care Quality Commission CPE Carbapenemase-producing Enterobacteriaceae. Enterobacteriaceae are a large family of bacteria that usually live harmlessly in the gut of all humans and animals. They are also some of the most common causes of opportunistic urinary tract infections, intra-abdominal and bloodstream infections. They include species such as Escherichia coli, Klebsiella spp. and Enterobacter spp. Carbapenems are a group of antibiotics normally reserved for serious infections caused by drugresistant Gram-negative bacteria (including Enterobacteriaceae). Carbapenemases are enzymes that destroy carbapenem antibiotics, conferring resistance. CSM Clinical Services Manager CSSD Central Sterile Services Department D&V Diarrhoea and vomiting DH Department of Health Director of Infection Prevention & Control DIPC E.coli Escherichia coli. E. coli is the name of a type of bacteria that lives in the intestines of humans and animals ESBL Extended-Spectrum Beta-Lactamases are enzymes that can be produced by bacteria making them resistant to many of the commonly prescribed antibiotics Glycopeptide-Resistant Enterococci/Vancomycin Resistant Enterococci. Enterococci are bacteria that are commonly found in the bowels/gut of most humans. There are many different species of GRE/VRE Infection Prevention Control Annual Report 2014/15 Page 44 of 62 HCAI enterococci but only a few that have the potential to cause infections in humans and have become resistant to a group of antibiotics known as Glycopeptides; these include Vancomycin. Patients who have already taken many antibiotics are more at risk of acquiring GRE/VRE due to the more bacteria is exposed to antibiotics, the more likely they are to develop ‘resistance’ to that antibiotic. Healthcare Associated Infection HEPA filter High Efficiency Particulate Air filter IPC Infection Prevention and Control IPS Infection Prevention Society MIU Minor Injuries Unit MRSA Meticillin Resistant Staphylococcus aureus. Any strain of Staphylococcus aureus that has developed resistance to some antibiotics, thus making it more difficult to treat. MSSA Meticillin Sensitive Staphylococcus aureus. Staphylococcus aureus is a bacterium that commonly colonises human skin and mucosa (e.g. inside the nose) without causing any problems. It most commonly causes skin and wound infections. OD Organisational Development OHS Occupational Health Service PEAT Patient Environment Action Team PHE Public Health England PII Period of Increased Incidence PIR Post Infection Review PLACE Patient Led Assessment of the Care Environment PPE Personal Protective Equipment e.g. gloves, aprons and goggles RCA Root Cause Analysis SaTH Shrewsbury and Telford Hospital NHS Trust SCHT Shropshire Community Health NHS Trust SIGHT Suspect, Isolate, Gloves and Aprons, Hand washing, Test for Toxins SI Serious Incident SIP Service Improvement Plan SSSFT Shropshire and South Staffordshire NHS Foundation Trust TDA Trust Development Authority TOR Terms of Reference WHO World Health Organisation Infection Prevention Control Annual Report 2014/15 Page 45 of 62 Appendix 1: 2014/15 Community Hospital Audit Programme undertaken by the IPC team Bishops Castle Community Hospital 2014/15 Audit Programme Area Audit Tool Quarter 1 Apr-14 May-14 Jun-14 Quarter 2 Jul-14 Aug-14 Sep-14 Quarter 3 Oct-14 Nov-14 Dec-14 HCAI Prevention 81% 81% 95% Hand Hygiene Observations Previous quarter HCAI SIP Verification HCAI Prevention 71% 89% 100% Quarter 4 Jan-15 Feb-15 Mar-15 80% Bishops Castle Physio Dept Key: Verified Verified Verified Verified 95% Unable to assess due to patient group Audit completed for this quarter Infection Prevention Control Annual Report 2014/15 Page 46 of 62 Bridgnorth Community Hospital 2014/15 Audit Programme Area Audit Tool Quarter 1 Apr-14 May-14 HCAI Prevention Bridgnorth Male Ward Jun-14 80% Aug-14 Quarter 3 Sep-14 Verified 09/05/2014 60% Hand Hygiene Observations 80% Verified 09/05/2014 Quarter 4 Dec-14 Feb-15 Mar-15 94% 100% 100% 96% 96% Verified 16/10/2014 Verified 22/01/15 83% 100% Verified 28/07/2014 Jan-15 83% 84% 30% / 80% Nov-14 86% Verified 28/07/2014 85% Oct-14 85% 79% HCAI Prevention Previous quarter HCAI SIP Verification Jul-14 82% Hand Hygiene Observations Bridgnorth Female Ward Isolation Previous quarter HCAI SIP Verification Quarter 2 86% 100% Verified 16/10/2014 100% Verified 22/01/15 Invasive Procedures 14/01/2015 Endoscopy/Cystoscopy 22/01/2015 98% Day Surgery HCAI Prevention 99% 91% MIU/OPD Colorectal ENT Clinic Nasendoscope Physio Dept HCAI Prevention X-ray HCAI Prevention Occupational HCAI Prevention Therapy Key: 70% 100% Building work Building work 95% 62% 98% 90% Unable to assess due to patient group Audit completed for this period Infection Prevention Control Annual Report 2014/15 Page 47 of 62 Ludlow Community Hospital 2014/15 Audit Programme Area Audit Tool Quarter 1 Apr-14 May-14 HCAI Prevention Ludlow Dinham Hand Hygiene Observations Ward Previous quarter HCAI SIP Verification HCAI Prevention Hand Hygiene Observations Ludlow Previous quarter HCAI SIP Stretton Ward Verification Quarter 2 Jun-14 Quarter 3 Jul-14 Aug-14 Sep-14 Oct-14 Quarter 4 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15 90% 92% 93% 88% 100% N/A 100% 88% Verified Verified Verified Verified 92% 89% 92% 100% N/A 90% Verified Verified Verified Isolation 85% MIU/OPD HCAI Prevention MIU Colo-Rectal ENT Clinic Nasendoscope Physio OPD HCAI Prevention Physio In-Pt HCAI Prevention Continence Services HCAI Prevention 92% X-Ray HCAI Prevention 93% 93% Verified 100% (Ward) 89% 89% 92% 94% 91% 86% N/A: Not applicable to undertake HHOTs with insufficient patient and staff numbers during refurbishment Key: Unable to assess due to patient group Audit completed for this quarter N/A: Not applicable to undertake HHOTs with insufficient patient and staff numbers during refurbishment Infection Prevention Control Annual Report 2014/15 Page 48 of 62 Whitchurch Community Hospital 2014/15 Audit Programme Area Audit Tool Quarter 1 Apr-14 Whitchurch Team 1 Jun-14 Jul-14 Quarter 4 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15 99% 89% 98% 91% Hand Hygiene Observations 100% 100% 100% 100% Verified Verified Verified Verified HCAI Prevention 94% 92% 94% 93% Hand Hygiene Observations 100% 100% 100% 90% Previous quarter HCAI SIP Verification Verified Verified MIU/OPD HCAI Prevention 86% ENT Clinic Nasendoscope 77% Physio Dept HCAI Prevention X-Ray HCAI Prevention Key: Quarter 3 HCAI Prevention Previous quarter HCAI SIP Verification Whitchurch Team 2 May-14 Quarter 2 Verified Verified 79% 81% Unable to assess due to patient group Audit completed for this quarter Infection Prevention Control Annual Report 2014/15 Page 49 of 62 Appendix 2: 2014/15 Community Services Audit Programme Community Services 2014/15 Audit Programme Service Location Audit Tool Quarter 1 Apr-14 May-14 Quarter 2 Jun-14 Jul-14 Aug14 Quarter 3 Sep-14 Oct-14 Nov-14 Quarter 4 Dec-14 Jan-15 Limeswalk Invasive Procedures 95% Bridge School HCAI Prevention 95% Monkmoor Centre HCAI Prevention Ludlow CH HCAI Prevention Whitchurch CH HCAI Prevention Portico House HCAI Prevention Burlington Place HCAI Prevention Oswestry Health Centre Decon of Nasendoscopes 100% Gateway Craven Arms HCAI Prevention 90% Rapid Response, Halesfield HCAI Prevention Oswestry Health Centre HCAI Prevention Minor Injuries Oswestry Health Centre HCAI Prevention Occupational Health Gains Park Shrewsbury HCAI Prevention APCS Children's Services Continence Service Community Substance Misuse Team ENT Clinics Integrated Community Teams Feb-15 Mar-15 80% 92% 100% 84% 90% 82% 90% 100% 94% Infection Prevention Control Annual Report 2014/15 Page 50 of 62 Physiotherapy Clinics Market Drayton HCAI Prevention Newport HCAI Prevention Wem HCAI Prevention 88% HCAI Prevention 80% Hummingbird Centre Newport Linden Hall Podiatry Prison Wheelchair and Posture Services Neuro Rehabilitation Team 82% HCAI Prevention Market Drayton HCAI Prevention Shawbury HCAI Prevention Wellington HCAI Prevention Woodside HCAI Prevention HMP Stoke Heath Shropshire Rehabilitation Centre Lancaster Road Shropshire Rehabilitation Centre Lancaster Road 81% HCAI Prevention HCAI Prevention HCAI Prevention 93% 83% 89% 92% 90% SIP Verified 51% 79% SIP Verified 85% Infection Prevention Control Annual Report 2014/15 Page 51 of 62 Appendix 3: 2014/15 Community Hospital Cleanliness Audit Scores Bishops Castle Cleanliness Audits 2014-15 110 105 100 95 90 85 80 Nursing 75 Domestics 70 Estates 65 60 55 50 % Bridgnorth Cleanliness Audits 2014-15 110 105 100 95 90 85 80 Nursing 75 Domestics 70 Estates 65 60 55 50 Infection Prevention Control Annual Report 2014/15 Page 52 of 62 % Ludlow Cleanliness Audits 2014-15 - Dinham Ward 110 105 100 95 90 85 80 Nursing 75 Domestics 70 Estates 65 60 55 50 % Ludlow Cleanliness Audits 2014-15 - Stretton Ward 110 105 100 95 90 85 80 Nursing 75 Domestics 70 Estates 65 60 55 50 Infection Prevention Control Annual Report 2014/15 Page 53 of 62 % Whitchurch Cleanliness Audits 2014-15 - Team 1 110 105 100 95 90 85 80 Nursing 75 Domestics 70 Estates 65 60 55 50 % Whitchurch Cleanliness Audits 2014-15 - Team 2 110 105 100 95 90 85 80 Nursing 75 Domestics 70 Estates 65 60 55 50 Infection Prevention Control Annual Report 2014/15 Page 54 of 62 Appendix 4: Analysis of HCAI Audits in Community Hospitals HCAI audits undertaken in Community Hospitals April 2014 – March 2015 A total of 42 Prevention of HCAI audits were undertaken in the four community hospitals. Table 1 below shows the number of instances each question was answered “no” in these audits and where they occurred. As discussed on page 42 the question most frequently answered “no” was regarding hand washbasins being clean and in a good state of repair Those which always answered yes are shown in Table 2. Table 1 – number of times each question answered “no” and where they occurred Total answered Question ‘No’ 2 x Bishops Castle Ward 4 x Bridgnorth Female Ward 4 x Bridgnorth Male Ward 1 x Bridgnorth Physio 1 x Bridgnorth MIU 1 x Bridgnorth Occupational Therapy 1 x Bridgnorth x-ray 2 x Ludlow Dinham Are hand washbasins accessible, in a good state of 4 x Ludlow Stretton 30 repair visibly clean and free from mould, limescale 1 x Ludlow MIU and extraneous items? 1 x Ludlow Outpatients Physio 1 x Ludlow in-patient physio 1 x Ludlow x-ray 1 x Ludlow Continence Unit 1 x Whitchurch X-Ray 2 x Whitchurch Team 1 1 x Whitchurch Team 2 1 x Whitchurch Physio 3 x Bishops Castle 4 x Bridgnorth Female Ward Is all furniture visibly clean, intact and made of 4 x Bridgnorth Male Ward 15 impervious material? 2 x Whitchurch Team 1 1 x Whitchurch Team 2 1 x Whitchurch MIU 1 x Bishops Castle 2 x Bridgnorth Female Ward 2 x Bridgnorth Male Ward Are SENDS available and staff have been trained 1 x Ludlow Dinham 11 how to use? 2 x Ludlow Stretton 1 x Whitchurch MIU 1 x Whitchurch Team 1 1 x Whitchurch Team 2 1 x Bishops Castle Are toilets visibly clean, in a good state of repair 3 x Bridgnorth Female 9 and free from extraneous items? 3 x Bridgnorth Male 2 x Whitchurch Team 2 2 x Bridgnorth Female 8 Is the sluice free from extraneous items? 2 x Ludlow Stretton Infection Prevention Control Annual Report 2014/15 Page 55 of 62 8 Are bathrooms/showers and equipment visibly clean and the area free from extraneous items? 8 Are examination trolleys/couches/plinths/chairs visibly clean and in a good state of repair? 2 x Ludlow Dinham 1 x Whitchurch Team 1 1 x Whitchurch MIU 1 x Bishops Castle 2 x Bridgnorth Female Ward 2 x Bridgnorth Male Ward 1 x Ludlow Dinham 1 x Whitchurch Team 2 1 x Whitchurch Team 1 1 x Bishops Castle 2 x Bridgnorth 2 x Bridgnorth Male 1 x Whitchurch X-Ray 1 x Whitchurch MIU 1 x Whitchurch Physio Table 2 - Questions which were ALWAYS answered “yes” Question Are hand hygiene products available and in date, including alcohol hand gel, liquid soap and paper towels and detergent hand wipes? Is alcohol hand gel available for use in the patients' bed space Are hand wipes available for patients? Is personal protective equipment available, accessible and stored appropriately? Is there a range of sizes of sterile and non-sterile powder free gloves available? Are waste bins enclosed, lidded and foot pedal operated? Are staff aware of the procedure for managing an inoculation contamination injury? Is there a mechanism to ensure that toilet cleaning can be carried out as needed? Are the commodes in good condition? Are all sterile products stored above floor level? Are sterile products sealed, in date and undamaged? Can staff describe the symbol used to indicate single use items? Is there a designated deep sink for washing used equipment? Are bedpans and urinals clean, in good condition and stored correctly to minimise contamination? Is the macerator in working order and clean? Is the cleaner’s cupboard visibly clean, tidy and free from extraneous items? Is the storage area/trolley visibly clean and free from extraneous items? Is used linen placed in linen bags at the point of use and not carried by staff There are no extraneous items in the ward kitchen Is there a hand washbasin with the appropriate products available? Infection Prevention Control Annual Report 2014/15 Page 56 of 62 Are green aprons used for handling/serving food? Are fridge temperatures recorded on a daily basis and within appropriate ranges? Are cleaning/disinfectant products available and easily accessible for decontamination? Is the pulse oximeter visibly clean? Are all stethoscopes visibly clean? Are bladder scanners visibly clean? Is blood glucose monitoring equipment visibly clean? Are monitoring leads/straps decontaminated between patients? Are tourniquets single-use? Is the resuscitation trolley/equipment in date, clean, free from dust and in a good state of repair? Is the suction machine visibly clean and dry? Are manual handling slings/sheets single patient use or laundered after use? Are PAT (Patient Assisted Transfer) slides visibly clean and stored appropriately? Are aids such as walking sticks, zimmer frames, helping hands visibly clean and stored in a suitable area? Are examination trolleys/couches/chairs visibly clean and in a good state of repair? Are reusable patient wash bowls visibly clean and in a good condition? Infection Prevention Control Annual Report 2014/15 Page 57 of 62 Appendix 5: 2014/15 Community Hospital Self-Audit Scores Bishops Castle Community Hospital 2014/15 Self Audits Area Audit Tool Quarter 1 Apr-14 Hand Hygiene Observations Bishops Castle 100% Quarter 2 May-14 Jun-14 100% 100% Jul-14 100% Aug-14 Sep-14 100% 100% 86% 100% 100% Quarter 3 Oct-14 Nov-14 Dec-14 Quarter 4 Jan-15 Feb-15 96% 100% Mar-15 Urinary Catheter Isolation Practices - at time of isolation 88% 97% Vascular Access Device - at time of insertion Enteral Feeding Key: Key 100% Unable to assess due to patient group Audit completed for this quarter Unable to audit due to patient group Infection Prevention Control Annual Report 2014/15 Page 58 of 62 Bridgnorth Community Hospital 2014/15 Self Audits Area Audit Tool Quarter 1 Apr-14 Hand Hygiene Observations Quarter 2 May-14 Jun-14 Jul-14 Quarter 3 Aug-14 Sep-14 77% 76% 90% Bridgnorth Urinary Catheter - Male Isolation Practices - at time of isolation Oct-14 100% Quarter 4 Nov-14 Dec-14 Feb-15 100% Mar-15 96% 100% 87% 73% 100% Jan-15 3 x100% 100% 100% 100% Vascular Access Device - at time of insertion Enteral Feeding 88% Apr-14 Hand Hygiene Observations Bridgnorth Urinary Catheter - Female Isolation Practices - at time of isolation May-14 Jun-14 90% Jul-14 Aug-14 Sep-14 77% 76% Oct-14 100% Nov-14 Dec-14 97% 90% Feb-15 100% 96% 90% Mar-15 96% 100% 100% 86% 98% Jan-15 100% 2 x 98% 100% 100% 100% Vascular Access Device - at time of insertion Enteral Feeding Key Key: Unable duetotopatient patientgroup group Unableto to assess audit due Audit completed for this quarter Infection Prevention Control Annual Report 2014/15 Page 59 of 62 Ludlow Community Hospital 2014/15 Self Audits Area Audit Tool Quarter 1 Apr-14 May-14 Jun-14 Quarter 2 Jul-14 Quarter 3 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Quarter 4 Jan-15 Feb-15 Mar-15 Hand Hygiene Observations Urinary Catheter Ludlow Dinham 97% Isolation Practices - at time of isolation 94% 92% 95% 87% 100% 100% Vascular Access Device - at time of insertion Enteral Feeding 100% 88% 100% Apr-14 May-14 Jun-14 Jul-14 Aug-14 Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15 Hand Hygiene Observations Ludlow Stretton Urinary Catheter Isolation Practices - at time of isolation Vascular Access Device - at time of insertion 100% 95% 2 x 100% 96% 100% Enteral Feeding Key Key: Unableto to assess audit due Unable duetotopatient patientgroup group Audit completed for this quarter Infection Prevention Control Annual Report 2014/15 Page 60 of 62 Whitchurch Community Hospital 2014/15 Self Audits Area Audit Tool Quarter 1 Apr-14 Hand Hygiene Observations 100% Quarter 2 May-14 Jun-14 100% 100% Jul-14 100% Quarter 3 Aug-14 Sep-14 100% 100% Oct-14 Nov-14 Dec-14 100% Urinary Catheter Quarter 4 100% 94% Whitchurch - Team 1 Isolation Practices - at time of isolation 100% 98% 100% 100% 100% 100% 100% Jan-15 Feb-15 Mar-15 100% 100% 100% 100% 100% 100% 98% 98% 100% 100% 100% 96% 100% 98% 100% Vascular Access Device - at time of insertion Enteral Feeding 88% Apr-14 Hand Hygiene Observations Urinary Catheter Whitchurch - Team 2 Isolation Practices - at time of isolation 100% May-14 Jun-14 100% 100% 100% Jul-14 100% Aug-14 Sep-14 100% 100% Oct-14 100% 97% 95% Nov-14 Dec-14 100% Jan-15 100% 100% 98% 100% 100% 100% 100% Feb-15 Mar-15 100% 100% 100% 100% 100% 100% 100% Vascular Access Device - at time of insertion Enteral Feeding Key: 100% 100% Unable to assess due to patient group Infection Prevention Control Annual Report 2014/15 Page 61 of 62 Appendix 6: Infection Prevention and Control Team 2014/15 Audit Programme INFECTION PREVENTION AND CONTROL TEAM 2015/16 AUDIT PROGRAMME Location Quarterly Audits Bishops Castle Community Hospital Ward Bridgnorth Community Hospital Male and Female Wards Ludlow Community Hospital Dinham and Stretton Wards Whitchurch Community Hospital Team One and Team Two Quarterly Alternate Audits and Verification of Service Improvement Plan Quarterly Alternate Audits and Verification of Service Improvement Plan Quarterly Alternate Audits and Verification of Service Improvement Plan Quarterly Alternate Audits and Verification of Service Improvement Plan Service Annual Audits Advanced Primary Care Services Children’s Services Continence Service DAART Integrated Community Teams Minor Injuries Unit Physiotherapy Podiatry Prison School Nurses Marysville Rheumatology, Hollinswood Oswestry Health Centre Euston House Severndale School Phoenix School Bridgnorth, Northgate Radbrook RJAH, Oswestry RSH, Shrewsbury Bridgnorth, Northgate Broseley/Much Wenlock Oswestry Bridgnorth Community Hospital Ludlow Community Hospital Whitchurch Community Hospital Oswestry Health Centre Broseley Princess House Bayston Hill Clive Hadley Marden Market Drayton Pontesbury Princess House South Hermitage HMP Stoke Heath (to include the Dental clinic) 1 in Shrewsbury 1 in Telford and Wrekin The audit programme is subject to amendments as need identified Infection Prevention Control Annual Report 2014/15 Page 62 of 62