Soft Tissue Palpation and Manual Therapy
advertisement
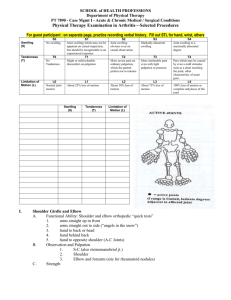
Manual Therapy for Athletes Bryan Bourcier DPT, ATC, COMT, CSCS Outline • • • • • • Manual Therapy basics Contraindications Indications Spine Mobilizations for Athletes Upper extremity Peripheral Mobilization Lower extremity Peripheral Mobilizations Manual Therapy Basics • Grading Mobilizations • Comparable Sign • Resistance vs Pain – R1 vs R2 – P1 vs P2 • Grades of Mobilizations – – – – – I – Small amplitude short of resistance II – large amplitude short of resistance III – Large amplitude midway between R1 and R2 IV - Small amplitude midway between R1 and R2 V- At R2 High velocity low amplitude • +, ++, -, -- variations • IV++ and III++ Contraindications (Red/Yellow • • • • • • • • • Fracture (red) Hypermobility / empty end feel (Yellow) Pregnancy (yellow) Cord Compression (Red) Cancer (Red) Patient comfort (yellow) Open wounds (yellow) Fusions (Red and Yellow) Manipulation into spasm (Red) • Treatment Options for Low Back Pain in Athletes – Ryan C. Petering, MD and Charles Webb, DO • Despite the high prevalence of low back pain and the significant burden to the athletes, there are few clearly superior treatment modalities. Superficial heat and spinal manipulation therapy are the most strongly supported evidence-based therapies. Nonsteroidal anti-inflammatory medications and skeletal muscle relaxants have benefit in the initial management of low back pain; however, both have considerable side effects that must be considered. Indications • • • • • Stiffness Pain management Scar tissue management “locking” or “Pinching” (Spine) Evidence – When combined with exercise, speed up recovery – Not better if used without exercise Common Cervical Spinal Mobilizations for Athletes • Suboccipital Release – Concussions • Traction • MET • Soft tissue What are we treating Concussion Whiplash •neck pain and stiffness, •headache, •dizziness •fatigue •jaw pain •activity intolerance •postural weakness •visual disturbances •tinnitus •increased symptoms with fatigue •neck pain and stiffness, •headache, •shoulder and arm pain •dizziness •fatigue •activity intolerance •jaw pain •postural weakness •visual disturbances •tinnitus •back pain •increased symptoms with fatigue Subocciptial release • Long sustained pressure on suboccipitals. – Can be done unitlaterally – Make sure knees are bent – If too painful, try traction first. Common Cervical Spinal Mobilizations for Athletes • Suboccipital Release – Concussions • Traction – Manual Vs Mechanical • MET – when and when not • Soft tissue – positional release and first rib Common Thoracic Spinal Mobilizations for Athletes • CT junction • Pistol • Screw C-T Junction Have the patient lay on their stomach while placing their arms above their head. Once you have the level that you want have the athlete look to the opposite side hand. Gently apply pressure on the junction while applying pressure on the patient’s head and rotating. Pistol Make and fist while extending your index finger and thumb. Place your fist over the level that you want to manipulate. The area where your fingers meet your palm should lay over the spine. Index finger and thumb should be over transverse processes. Have the patient put their hands on their neck, with elbows together and knees bent. Have the patient exhale and while exhaling push the athlete over your hand as a fulcrum. Screw Have the patient lay on their stomach. Once you have the level that you want, place one hand one the level above and the other hand on the level below. The palm of your hands should be on the level. Then apply pressure down while turning your hands inward. Common Lumbar Spinal Mobilizations for Athletes • Rotational Mobilization – Grade I-III – Manipulation • • • • • Chicago Roll Shotgun SI / IS MET Leg Pull A/P Rotational Have the athlete lay on their side facing you. Straighten the bottom leg and push it to the opposite side of the table. Bend the top leg and bring it towards you. Have the patient interlock their arm with yours. Place your other arm on the bottom part of their back and over their SI joint. Rotate their top shoulder down to the table and pull their hips towards you with the other arm. Chicago Roll Have the patient lay on the side of the table nearest you. Bring their legs together and to the side of the table. Put one hand under their back shoulder and the other hand on the ASIS. Rotate their shoulder up and towards you while applying pressure on the ASIS. Shotgun Have the patient lay on their back with their knees bent and feet together. Then have them squeeze your forearm. Upper extremity Mobilizations • Shoulder – “Fish Flop” (Shoulder pain control) • Elbow – Radial Head • Wrist – Distal Radial ulnar distraction Lower Extremity • Hip – Lateral glides (FAI) – AP and PA • Knee – Extension with ER and IR (post op and Hamstrings) • Ankle – Lateral malleolus glides (Ankle Sprains) Soft Tissue Palpation and Manual Therapy Craig Shannon, MPT, OCS, ATC TherapyONE Overview • • • • Palpation of Structures Palpation of Movement Joint Mobilization Soft Tissue Mobilization • Multiple Methods • Improving your sense of touch Palpation of Structures • Palpation of Surface Anatomy • Know your surface anatomy • Know where structures are in relation to the Spinal Levels Palpation of Movement • Spinal Movement • Joint Movement • Soft Tissue Movement Palpation of Spinal Movement • AROM of all planes of motion • Feeling for Symmetry • Feeling for Segmental Restriction or Hypermobility • Passive mobility testing • Checking the “R’s” • Endfeels Palpation of Joint Movement • AROM • Feeling for • • • • Crepitus Endfeels Muscle Guarding Symmetry • Special Testing Soft Tissue Palpation • What is the Nature of the Injury? • History and Symptom Patterns • Mechanism of Injury • • • • Acute Trauma Chronic Postural Repetitive • • • • Tear Adhesion Crush Myofascitis • Type of Injury • Tissues Involved • Muscle • Joint Capsule • Nerve Soft Tissue Palpation • 4 Keys to Soft Tissue Palpation • Tissue Texture • Tissue Tension • Tissue Movement • Tissue Function Tissue Texture • Inflammatory Phase • 1st 24-72 hours • Typically swelling is fluid like and easily moveable • Usually undefined borders • Sub-Acute Phase • • • • 2-14 days Increased tension in tissues – Hypertense Feels Stringy Borders become more well defined and palpable Tissue Texture • Early Chronic • 2 weeks – 3 months • Tissues healing through Fibrosis • Texture transitions from Stringy to Lumpy • Chronic • 3 months + • Tissues become Leathery and Tough • Altered vascularity and more scar-like Tissue Tension • Difficult to be objective • Must rely on the Contralateral side to compare • If ROM restricted – tissue tension considered Abnormal • Must be specific of what structure is involved • Palpate tissues at rest and with ROM • Compare surrounding tissue tension • Clinician will need to develop a Feel for what is Normal Tissue Movement • How do the tissues move with each other • • • • Skin and superficial fascia Fascia and Muscle Muscle and Joint Capsule Nerves and Fascia/Muscle • Need to learn to palpate to the proper level • Peeling Onions • Palpate with and without movement Tissue Function • What about the tissues is dysfunctional? • Weak • Restricted • Neurogenic issues (paresthesias) • The rest of your examination should help tease this out Joint Mobilization • What Bryan Said! Soft Tissue Mobilization • Massage • Cross-Friction Massage • Tool Assisted STM • • • • ASTM Graston SASTM Knife and Spoon • Active Release Techniques (ART) • Myofascial Release Soft Tissue Mobilization Basics • Need to develop your sense of touch • Like putting in golf, shooting a 3, juggling a soccer ball • Know your Anatomy…Specifically • What is your targeted tissue or tissues • Don’t “Press and Guess” • What is the goal of your treatment? • • • • • Relaxation Decrease pain Decrease swelling Restore tissue mobility Restore joint or muscle ROM Improving Palpation Skills • Need to know what Normal is before you can Identify Abnormal • Use a Soft Contact to help Identify structures and tissues • Chiropractic Tricks to improving a sensitive sense of touch • Hair in a phone book trick • Nose on a Quarter trick • Practice and Patience • You won’t find anything if the tissues are too swollen • Save the “digging” for treatment Thank You