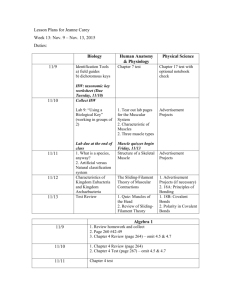
Kine 1020: Exam Review Why is Strength Important?
advertisement

Kine 1020: Exam Review Why is Strength Important? Performance-Related Sport o Greater power, speed and balance o Reduce demands on cardiovascular system Job/Occupational Requirements o Reduced risk of injury o Productivity Health-Related Lower risk of functional limitations o Avoid injuries/infirmity o Predictor of advanced age disability o Reduces chronic low back pain Lower Risk of Chronic Diseases o Improved blood sugar control o Retard/prevents osteoporosis o Increase metabolic rate Psychological Heath o Improved self-­­image o Emergencies Emergencies HEALTH-RELATED Maintaining or improving muscular strength later in life reduces the percentage of functional limitations by over 50% for both men and women. Peopleawith greater muscle strength during midlife are at a lower risk of becoming disabled because of their greater reserve of strength rega rdless of chronic conditions that may develop. Decreasing Muscle Strength With Aging Sarcopenia is the loss of muscle mass and strength due to aging process o ~1-2% muscle mass per year past 50 yrs of age – loss of strength varies and may be greater Prevalence o Impacts 10-25% of the population under 70 yrs of age and ~40% above 80 yrs of age o By 80 yrs a loss of 30-40% of the muscle fibers (hypoplasia of muscles containing Type II muscle fibers) Concerns o Risk of functional limitations Sarcopenia is a result of Programmed Cell Death – Apoptosis Characterized by: DNA fragmentation; and Nuclear condensation leading to formation of apoptotic bodies (these are engulfed by macrophages but do not induce an inflammatory response) Potential Causes of Sarcopenia I) Activation of apopotic pathways – caspases (enzymes that breakdown and degrade proteins and DNA) II) Loss of hormonal adaptations (decrease in testosterone and growth hormone) III) Loss of neurological influences (selective loss of type II motor units resulting in cluster of Type I muscle fibers with age) Activation of proteolytic pathways – proteases (enzymes that breakdown and degrade proteins) by: I. Caspase-dependent a) Ionic Imbalance (accumulation of intracellular calcium) b) Oxidative stress (accumulation of reactive oxygen species (ROS) which are considered damaging) c) Mitochondrial dysfunction (a decline in ATP levels, increase in oxygen free radicals – membrane leakage) II. a) Mitocohondial dysfunction – apoptosis-inducing factor (AIF) – results in DNA fragmentation Inpact of Training (strength and endurance) on Apoptotic Pathways in the Elderly Improved calcium handling – therefore not as much accumulation Increased Bcl-2/Bax ration (therefore less cytoch-c leakage) Decreased Apaf-1 Reduced AIF Muscles Diseases: Definitions and Types Any disorder or disease that affects the human muscle system: a) Primary Muscle Disease – the pathology originates with the muscle (internal membranes/metabolic) disorders; [examples – McArdle’s Disease; Forbe’s Disease] b) Secondary Muscle Disease – the pathology originates in other systems: Nerve – neuromuscular disease/disorder [Parkinson’s Disease; muscular dystrophy] Bone/joint – musculoskeletal disease/disorder Inflammatory System – inflammatory muscle diseases/disorders [Dermatomyositis] Immune System – autoimmune muscle diseases/disorders [Multiple Sclerosis; Myositis; Muscle Rheumatism] Muscle Diseases: Symptoms/Indicators 1) Muscle atrophy (decrease size) and accompanying muscle weakness 2) Pain – defects in cardiovascular system, inflammatory system 3) Tetany – involuntary contractions (spasms) because of changing calcium levels – generally larger muscles of arm and legs; 4) Twitching – single motor unit firing due to loss of nerve cells – typically close to surface of the skin 5) Muscular hypertrophy and accompanying increase in stiffness (myotonia congenital); increase size due to more fat in muscle – form of muscular dystrophy 6) Biochemical parameters Reduced muscle glycogen; mitochondrial oxidative potential; Increased myoglobin, acid maltase; CK… Muscle weakness failure to develop an expected force which can be attributed any one of the processes requires for force generation. This is associated with all types and examples of muscle diseases/disorders Classifications: a) Upper motor neuron disease Muscle weakness typical of upper motor neuron disease includes: I) CV-stroke producing weakness of one side of the body. The arm is typically flexed, the leg is extended, and the limbs have increased tone. Some movement may be preserved, although the use of the hand is particularly limited. II) With upper motor neuron disease the muscle bulk is usually well preserved (different than lower motor neuron) III) Other causes of upper motor neuron disorders include tumors and spinal cord injury b) Lower motor neuron disease – flaccid muscle weakness 1. Spinal Cord – muscle wasting is prominent shrinkage and eventual death of neurons denervation of muscle. I) II) III) IV) Motor neurons lying in the spinal cord most common amyotrophic lateral sclerosis and Lou Gehrig disease Generally between 50 and 70 years of age and have upper and lower motor neuron weakness – paralysis progresses rapidly, and death within three years. Infant amyotrophic lateral sclerosis is fatal within one year No cause is yet known for any of these diseases, and no cure is available 2. Peripheral Nerves Diseases (peripheral neuropathies or polyneuropathies) Symptoms usually begin in the hands and feet and progress toward the body – also associated with sensory disturbances I) Peripheral neuropathies – degeneration of the axons (core of nerve fibres). Axons can regenerate but only at a rate of one to two millimetres per day. Thus, after injury to a nerve at the elbow the hand will not recover for six to nine months. Damage to blood vessels (physical and/or chemical) tend to cause axonal types of neuropathy. II) Myelin Sheath – peripheral neuropathy caused by degeneration of the myelin sheaths (covering of axons) – demyelinating neuropathies Symptoms are similar to axonal neuropathies but since the axons remain intact, the muscles rarely atrophy. Recovery from demyelinating neuropathies can be rapid Other causes of peripheral neuropathy include diabetes mellitus nerve trauma, inherited factors, and chronic renal failure c) N-M junction disease I) These diseases are associated with weakness and fatigability with exercise. II) Diseases of the neuromuscular junction typically involve the generation of an end-plate potential that is too low to propagate an action potential in the muscle fibre. III) Diseases of neuromuscular transmission may be acquired or inherited and may be the result of autoimmune disorders, such as myasthenia gravis congenital disorders; toxins such as those present in botulism Muscle weakness Etiology Muscle contraction results from a chain of events that begins with a: I) Nerve impulse traveling in the upper motor neuron from the cerebral cortex in the brain to the spinal cord II) The nerve impulse then travels in the lower motor neuron from the spinal cord to the neuromuscular junction; III) Where the neurotransmitter acetylcholine is released. Acetylcholine diffuses across the neuromuscular junction, stimulating acetylcholine receptors to depolarize the muscle membrane IV) The result is the contraction of the muscle fibre (actin/myosin) Contraction depends on the integrity of each of these parts; disease or disorder in any part causes muscle weakness. Muscle Diseases: Muscular Dystrophies The muscular dystrophies are a group of hereditary disorders (n=9) characterized by progressive muscular atrophy and weakness. In most varieties the muscles of the limb girdles – the pelvic and shoulder muscles – are involved. There is a progressive loss of muscle size and strength which is caused by loss of muscle proteins later changing to muscle fiber death and tissue death Assessments include: I) Measurement of the activity of creatine kinase in the blood II) Analysis of a muscle biopsy (structural), and III) Recordings from an electromyography frequently establish that the muscle weakness is due to primary degeneration of the muscles Nine Types of Muscular Dystrophy Steinert’s Disease or Myotonic Muscular Dystrophy: It is the type of muscular dystrophy which is most common in adults, as its name tells, in this disorder the muscles remain in spasms or become stiffened after slight use or exercise, and lower temperatures increase these symptoms. This type affects both males and females Duchenne Muscular Dystrophy: It is the type which is most common in children and it only affects males between 2-6 years of age, decrease in the mass of muscle is progressive and in most cases the children are wheelchair ridden by the start of their teens years Usually do not survive more than 20 years Becker Muscular Dystrophy: This type similar to Duchenne but the symptoms are milder and can appear till 25 years of age. Usually the affected people can live and enjoy life and are also able to walk but they have some heart problems and is present only in males. Emery-Dreifuss: It is the type which affects from childhood to teen years and is present only in the males It affects the muscles of pectoral region to upper arms and lower parts of legs And along with that patients have extreme heart problems that are usually fatal Limb-Girdle: It is the type which affects from teenage years to adulthood and is present in both males and females As the name indicates, in this type the problem starts from hip (pelvic girdle) region and then reaches to the shoulders (pectoral girdle) and later legs and arms are also affected The sufferers are unable to walk and most patients live past mid adulthood Fascioscapulohumeral Muscular Dystrophy: As the name indicates in this type of muscular dystrophy the muscles of face, scapula (shoulder blade) and humerus (shoulder joint and elbow joint) are affected It affects both males and females but about half of the sufferers are able to walk throughout their life And almost all the patients live a normal life span Oculophyrangeal Muscular Dystrophy: It is the type of muscular dystrophy which affects primarily the muscles of eyes and throat which occur around 40s to onward ages Symptoms include the weakness of eyes and facial muscles which could later cause swallowing problems This type predisposes the patients to pneumonia and choking Muscle Diseases: Myasthenia Gravis Myasthenia gravis is an acquired autoimmune disorder that involved a failure in the transmission of nerve impulses to the muscles and is characterized by persistent muscular weakness and a tendency of muscles to be easily fatigued. Symptoms include: Weakness is particularly of the face, limbs, and neck Double vision Difficulty swallowing and breathing Excessive muscle fatigue during exercise with partial recovery after rest Disease can be controlled by: 1) Treatment with high doses of corticosteroids (which depress the immune response) 2) Anticholinesterase medications (which stimulate the transmission of nerve impulses) Muscle Diseases: Myotonic Diseases Myotonia is a difficulty in relaxing (slow relazation) a muscle after contraction (i.e., relaxing the hand after a handshake). Causes: Continuing electrical activity of the sarcolemma (the membrane of striated muscle fibres) – multiple firing of the nerve is most common form Problem lies in abnormal ion channels or ion pumps in the sarcolemma Delayed disengagement of the thick and thin filaments of myosin and actin Physical inactivity and cold enhance the condition. Muscle Diseases and Disorders: Fibromyalgia Fibromyalgia is a common syndrome in which a person has long-term, body-wide pain and tenderness in the joints, muscles, tendons, and other soft tissues. Fibromyalgia has also been linked to fatigue; sleep problems, headaches, depression, and anxiety Causes and Incidence: The cause is unknown. Possible causes include: I) Physical or emotional trauma II) Abnormal pain response – EEG areas in the brain that are responsible for pain may react differently in fibromyalgia patients III) Sleep disturbances IV) Infection, such as a virus, although none has been identified Fibromyalgia is most common among women aged 20 to 50 Symptoms: Pain is the main symptom of fibromyalgia – ranging from mild to severe. I) Painful areas are called tender points. Tender points are found in the soft tissue on the back of the neck, shoulders, chest, lower back, hips, shins, elbows, and knees. The pain then spreads out from these areas. II) Pain may feel like a deep ache, or a shooting, burning pain III) Joints are not affected, although the pain may feel like it is coming from the joints Tend to wake up with body aches and stiffness Pain can improve during the day or stay all day Pain may get worse with activity, cold or damp weather, anxiety, and stress Fatigue, depressed mood, and sleep problems are seen in almost all patients with fibromyalgia – difficulty falling and staying asleep; constant feeling of tiredness Assessment: To be diagnosed with fibromyalgia, you must have had at least 3 months of widespread pain, and pain and tenderness in at least 11 of 18 areas, including: arms (elbows), buttocks, chest, knees, lower back, neck, rib cage, shoulders, thighs Treatment: The goal of treatment is to help relieve pain and other symptoms, and to help a person cope with the symptoms The first phase of treatments may involve one or more of the following: I) Physical therapy II) Exercise and fitness program III) Stress-relief methods, including light massage and relaxation techniques Skeletal Muscle: Adaptations, Strength Training and Conditioning Outline Muscular Adaptations Acute – injury and damage Chronic – fibre transitions, hypertrophy Timing Principles of Strength Training Program Design Characteristics Strength/Resistance Training and Muscular Adaptations Acute changes – are associated with Skeletal Muscle Fatigue a) The inability to maintain the required power output which is related to a decline in both force and velocity. b) A condition in which there is a loss in the capacity for developing force and/or velocity of muscle resulting from muscle activity under a demand/load which is reversible by rest c) The inability to maintain the required power output which is related to a decline in force, velocity and power, which is reversible Acute Changes – Characteristics of Fatigue: Eccentric Contractions Decreased strength/power output Muscle damage (injury) Delayed onset muscle soreness (DOMS) Restricted range of motion (ROM) Increased blood proteins Many mechanisms have attempted to explain the fatigue process Fatigue – possible sites/causes Central 1) 2) 3) 4) Planning of voluntary movement Motor cortex and supraspinal outputs Upper motor neurons Lower motor neurons Peripheral 5) Neuro-muscular (NM) junction and sarcolemma 6) Sarcoplasmic reticulum (Ca2+ movements) 7) Actin-myosin interaction 8) Metabolic supple (all 3 systems) and accumulation Neuro-Muscular (NM) Junction and Sarcolemma: High Intensity Contractile Activity A) Neuromuscular junction: No evidence that N-M blockage (either release or uptake of acetylcholine) is a problems B) Sarcolemma and t-Tubule Systems: Action potential propagation – is changed I) Fatigue is associated with a +10mV change in membrane potential; resting membrane electrical potential goes from -80 to -70mV with heavy exercise II) Fatigue associated with a drop in the amplitude of the action potential (peak of excitation); therefore not sufficient to activate channels in Ttubule system – caused by potassium (K+) leaking out of muscle cell (which is accompanied by Na+ leaking in) III) Na+-K+ pump has been suggested – decrease in ATP or increase in ROS Sarcoplasmic Reticulum (Ca2+ movements) Fatigue with heavy exercise associated with: A reduction in SR calcium concentration as a result of decreased SR Ca2+ ATPase pump (SERCA) and/or because more calcium remains bound in SR (possibly linked/bound to phosphate) I) Reduced SERCA activity due to: Lower [ATP] Inefficient or Leaking – because of action of ROS II) Increased Binding due to: Increased inorganic phosphate which comes from increasing muscle contractions End result less calcium for releaseupon stimulation/excitation and conversely more calcium remains in the cytoplasm with heavy exercise (fatigue) Muscle Weakness and Low Frequency Fatigue (LFF) The Ca2+ release channel (ryanodine receptor – RyR) does not release sufficient calcium – ‘less activation’ Actin-Myosin – Contractile Protein Interactions Fatigue with heavy exercise associated with: I) Increasing inorganic phosphate (pi) Which delays detachment phase of A-M cross-bridges II) Increasing hydrogen ions levels will decrease the pH Heavy exercise from ~7.2 to ~6.8 (more acidity) Myosin ATPase activity is reduced at lower pH Fatigue with heavy exercise associated with: I) Loss of contractile protein(s) ~60% reduction in each of myofibrillar proteins troponin-I, tropomyosin II) Loss of cytoskeletal (structural) proteins ~%0% loss of alpha-actinin (z-line) ~80% loss of desmin (myofibril-linking protein) Cause: Myofibril protein losses a result of increased protease activity – calcium activated neutral protease Calpain (CANP1; CAPN2) Metabolic Supply (3 systems) and Accumulation Fatigue with heavy exercise associated with: A) Phosphagen Sources I) Reduced levels or lower supply of creatine phosphate (CP) or phosphocreatine (Pcr) – can be ~80% depleted B) Anaerobic Glycolysis I) Lower supply – reduced glycofen concentrations II) Build up or accumulation of intracellular muscle lactate (vs lactic acid) C) Aerobic – oxidative phosphorylation I) Accumulation or increased ROS Chronic Impact of Fatigue with Heavy Strength/Resistance Exercise Resistance training Muscle hypertrophy Endurance training Mitochondrial biogenesis Muscular Adaptations to Strength/Resistance Training Muscular Adaptations – remodeling A) Muscle Fibre Transitions B) Muscle Hypertrophy C) Timing of Muscular Adaptations Muscular Adaptations – Remodeling Formation of new muscle fibres is critical to normal muscle function – ‘turnover’ Number and type of muscle fibres genetically determined Replace old fibres with new fibres – remodling Formation of new muscle fibres is called myogenesis; Satellite cell myoblast myotube muscle Activators include myoD and myogenin Inhibitors include myostatin Stimulation of myogenesis with training? Resistance Training Increases myoD and myogenein expression (peak ~36hr) Reduces myostatin Endurance Training Modest impact on regulators of myogenesis Muscular Adaptations – Muscle Fibre Transitions (identified through MHC) Transformations I) MHC – T1/2 is ~30 hrs II) MHC changes after 2-3 workouts III) More oxidative Muscular Adaptations – Hypertrophy Increase in size of muscle (also muscle fibre) with strength/resistance/anaerobic training Increase in muscle fibre size due to more protein (accretion) as a result of increased protein synthesis Therefore hypertrophy resulting from training is a result of protein degradation and protein synthesis Cucles of degration (PD) and synthesis (PS) are critical for hypertrophy (and transitions) PD – peak at end of exercise and slows down in recovery lasting ~24hrs PS – little increase immediately after exercise and reaches peak ~36-48hrs of recovery Factors promoting PS Are there muscle fibre specific adaptations? Muscular Adaptations – Hypertrophy and Muscle Fibre Types Resistance Training Both types increase (Type II>I) 3-6 months: increase in Type II ~35% increase in Type I ~20% Athletes vs untrained: Type II ~132% then UT Type I > ~60% then UT Factors Promoting Protein Synthesis: Intensity and volume of the workload Principles of strength/resistance training Nutrient intake Type Timing Hormonal Environment Intensity and volume of the workload I) Contraction Type – eccentric > concentric: Type I CON(0%); ECC(25%) Type II CON(5%); ECC(40%) *linked to increased protease activity damage: leading to increased organelle disassembly (i.e., sarcomere), protein targeting (E3-ligases) cell ‘clean-up’ II) Tension – greater tension > membrane disruption results in Release of growth factors (calcineurin) and Increase in signaling pathways (kinases; AkT; mTOR) for gene transcription and PS III) Metabolic Stress – greater anaerobic contribution to energy (ATP) production greater growth hormone response Associated with: High tension – restricted or occluded blood flow Moderate loading, high volumes and short rest intervals Nutrient Intake I) Water (cellular hydration is associated with decreased protein degradation and increased protein synthesis Creatine loading – results in cellular hydration II) Carbohydrates – increasing intake insulin Strength athletes – 55%-65% CHO; or 6g/day III) Protein (amino acids – 9 essential increased in diet (intake) or supplementation Diet recommend range of 1.7 to 2.2 g/kg Supplementation – brain-chained amino acids; whey protein Hormonal Environment I) Androgenic – testosterone II) Anabolic – steroids; testosterone esters; growth hormone; testosterone enhancers (banned, unethical substances) Structural Changes 1. Increased number of myofibrils 2. Increased density (amount) of the sodium-potassium pump (Na2+-K+ATPase); sarcoplasmic reticulum; and t-tubule 3. Results in an improved calcium handling (important for power/speed activity) 4. Hyperplasia (increase in muscle fibre number) – human? Strength/Resistance Training: Principles of Program Design Progression (habituation) is a long term goal of all programs No training/workout equals no benefits Ten Success Factors Muscle Action(s) Repetitions Set Volume intensity frequency Exercise Selection Exercise Order Rest Periods/Intervals Repetition Velocity Muscle Actions ECC>CON – both are considered dynamic actions with constant external resistance (i.e., isoinertial) results in variable force production throughout the range of option (ROM) ISOM (isometric) – no movement with constant external resistance ISOK (isokinetic) – variable external resistance – force production across the ROM is constant Repetition Complete movement cycle – ie, moving a weight up and down Set A specified group or number of repetitions Volume Total amount of work performed during a workout Intensity Magnitude of loading (weight lifted) – related to RM (maximum weight lifted in 1 effort) 1RM or 90% of 1RM Frequency Number of training sessions per day or week Exercise Selection A selected group of exercises to be performed in a session or training program Exercise Order Sequence of exercises Rest Periods/Intervals Amount of rest taken between sets, repetitions and/or exercises Repetition Velocity Velocity at which reps are performed Five Basic Principles – generic to all programs: Progressive Overload Specificity Variation Individualization Reversibility Principle of Progressive Overload Refers to gradual increase in physical stress/demand on the whole body and/or segments Without PO muscles accommodate or become ‘stale’ (i.e., accommodation) resulting in minimal benefits PO required for muscular adaptations – ‘training stimulus’ ‘Success’ factors are applied to the concept of progressive overload – ‘needed for success’ Any combination of success variable can be applied – goal of individual program must be identified National Strength and Conditioning Association American College of Sports Medicine Anatomy of the Respiratory System CONDUCTIVE ZONE (no gas exchange): Mouth/nose --? Trachea larynx bronchi --? Bronchioles humidifies, warms and filters are RESPIRATORY ZONE (gas exchange): Bronchioles alveoli Lung Function Tests Routine spirometry tests basic lung function Munute Ventilation (rest) = Breathing Freq (breath/min) * Tidal Volume (L) = 12-15 (breath/min) * 0.5 (L) = 6.0-7.5 L/min Sinoatrial (SA) Node “pacemaker” of the heart P wave activation of the atria QRS Complex activation of the ventricles T Wave recovery wave Why do we need the atria? Walls are thin so blood can easily return into the heart Atria contractions, ‘over’ fill the ventricles so that they are slightly stretched and allow for a better contraction and ejection fraction (Frank-starling Mechanism – elastic recoil). Not possible with the low venous blood pressure alone Ventricle walls are much thicker so that it can generate the blood pressure necessary to distribute blood around the body Normal Resting Values Heart Rate (HR): 50-80 bpm Stroke Volume (SV): 60-80 mL/beat Elite Values Heart Rate: 30-40 bpm Stroke Volume: 90-110 mL/beat Composition of Inhaled Air 21% Oxygen 78% Nitrogen How Does Oxygen Travel in the Blood? Red blood cells contain several hundred hemoglobin molecules which transport oxygen Oxygen binds to heme on the hemoglobin molecule Carries 98.5% of all oxygen molecules Holds up to 4 oxygen molecules Also carries other gasses (CO2, CO, NO, etc.) What Happens With Exercise? 1 L O2= 5 kcal The oxygen intake reaches a steady state to meet the energy demands using aerobic metabolism This process takes time Where does the ‘extra’ energy come come? What is a MET? 1 MET = 3.5 mL O2/kg/min Amount of energy you use at rest Marker of exercise intensity What Happens with Exercise? Fick’s Equation: VO2 = Q x (CaO2 – CvO2) Heart Rate: Vagal (parasympathetic) withdrawal ~100-110 bpm (quick) Sympathetic activation HRmax(slower) Stroke Volume: Frank-Starling mechanism (elastic recoil) Reduced peripheral resistance Age-predicted heart rate maximum = 220-age Usually accurate within 10-15 beats per minute Used to predict exercise intensity much easier than measuring oxygen uptake (VO2) Stroke Volume: Increases with exercise Greater contractility Reduced peripheral resistance (vasodialation) Increased ejection fraction (heart empties more) Elite athletes have higher stroke volumes Exercise and Oxygen Extraction Extraction is related to the diffusion gradient, diffusion area and barriers to diffusion You deliver more oxygen and extract a greater proportion What Limits Maximal Exercise? VO2 = HR x SV (CaO2 – Cv O2) Would we increase VO2max if we could make: 1. The heart beat faster 2. The heart beat more blood per beat 3. Deliver more oxygen Increases Hb in some but not all (increases oxygen delivery) Blood doping definitely works 4. The muscles take up more of the oxygen that is delivered to it More capillaries (increases diffusion area) unlikely Q Limits Maximal Exercise Muscle capacity for blood flow is greater than the heart’s ability to give it Immediate Energy Sources Anaerobic – Alactic System ATP = Adenosine Triphosphate 7.3-11 kcal ATP ADP + Pi + Energy (2-3 sec) PCr + ADP ATP + Cr (6-8 sec) Energy Systems for Exercise Energy Systems Immediate: ATP-PCr (ATP & phosphocreatine) Short Term: Glycolytic (Glycogen-Lactic Acid) Long Term: Oxidative Mole of ATP/min 4 Time to Fatigue 5 to 10 sec 2.5 1 to 2 min 1 Unlimited Time Glycolysis – Anaerobic Glycolysis does not require oxygen (anaerobic) ATP-PCr and glycolysis provide the energy for ~2 min of all-out activity Pyruvate Metabolism Anaerobic Without oxygen present, pyruvate produced by glycolysis becomes lactate lactic acid) Lactate can be transported by blood to liver and used in gluconeogenesis (produce glucose) Too much lactate forms lactic acid and lowers the pH impairing enzyme activity The Oxidative System The oxidative system uses oxygen to generate energy (aerobic) Oxidative production of ATP occurs in the mitochondria Can yield much more energy (ATP then anaerobic systems) The oxidative system is slow to turn on Primary method of energy production during endurance events Anaerobic and Aerobic Energy Production Glycolysis: Breakdown of glucose (anaerobic: 2 ATP) Krebs Cycle: production of ATP, NADH, FADH, (aerobic: 38 ATP) Common Criteria Used to Document Successful VO2max Test Primary Criteria Plateau in VO2 despite increasing work rate Secondary Criteria HR >90% of age predicted max Blood lactate > 8 mmol/L PRE > 17 RER > 1.10 RPE – Rating of Perceived Exertion (Borg Score) 6-20 Respiratory Exchange Ratio Respiratory exchange ratio (RER) measurable RER = VCO2(expired)/VOz(consumed) Indicates type of substrate being metabolized: 0.7 (100% Fat) to 1.0 (100% Carbs) Respiratory Quotient (RQ) theory What Happens During Maximal Exercise? RER goes up with exercise due to increased carbon dioxide production relative to oxygen consumption Related to buffering of lactic acid production How Do We Counteract Too Much Lactic Acid? Bicarbonate (released from kidneys) helps to buffer the acid H+ + HCO3- H2CO3 CO2 + H2O What is Tvent? Ventilatory Threshold: is the point in which the ventilation increases disproportionately to oxygen uptake Why Should I Care About Tvent? At intensities higher than Tvent there is an abrupt increase in blood lactate levels and the individual cannot maintain steady state exercise More trainable than VO2max Occurs at 50-60% of VO2max in untrained endurance individuals Occurs at 80-90% of VO2max in elite, world-class endurance athletes Allows the individual to be capable of maintaining a higher level of steady state during the endurance exercise A better indicator of endurance performance than VO2max as it tells you how much of your VO2max you can use a steady state Cardiorespiratory Fitness Training 1. Frequency of Training Optimal 3-5 days/week No benefits with < 2 days Benefits will plateau at 5 days 2. Intensity of Training Lower intensity will only increase fitness in individuals who are unfit Lower intensity = Longer duration vs Higher intensity = Shorter during Higher intensity prone to injury and over training 3. Time (Duration) of Exercise 20-60 mins of continuous or intermittent aerobic activity in a day Lower intensity exercise (40-65% VO2max) should be conducted over a longer period of time (>30 mins) 4. Type (Mode) of Training Any activity that uses large muscle groups, is rhythmic and aerobic in nature, and can be maintained continuously How Much Can I Improve My VO2max? Studies > 5 months 3-5 days per week 20-25% Improvement There is substantial inter-individual differences Endurance Strategies Carb loading Fat loading PCr Sodium Bicarbonate Inventory of Fuel Supply Carbohydrate Muscle Glycogen 350g (1400 kcal) Liver Glycogen 60g (240 kcal) Plasma glucose 10g (40 kcal) Protein Whole body (24 000 kcal) Fat Muscle 500g (3850 kcal) Adipose tissue 14kg (107 800 kcal) Carb Loading and Performance No benefit for events less than 90 min Extra water weight Bloating Events longer than 90 mins Postpone time to fatigue by 20% Improves time to go a set distance by 2-3% Replenishment of Glycogen Beginning immediately post-exercise (Golden hour) Continue until 500g ingested or a large, high-carbohydrate meal is consumed Moderate to high glycemic index CHO are more effective in regenerating glycogen stores than low GI Glycogen stores replenish at a rate of about 5 to 7% per hour High-fat Diet and Performance >30% fat Many studies use >50% Theory: use more fat and spare glycogen Acute Effects of a High-fat Diet Lower muscle and liver glycogen stores Lower whole-body CHO oxidation Increased rating of perceived exertion Creatine Supplementation Found in dietary meat 90% stored in skeletal muscle (60% as PCr) 70%of people will increase creatine stores with supplementation (20g/day) Aid in high intensity activities <30 sec Power/strength (5-15%) Single (1-5%) and repetitive (5-15%) sprint performance Jumping, cycling, but not running No help for endurance events Sodium Bicarbonate Ingestion Help with buffering acid 0.3-0.5g/kg/BM Improve mean power by 2% in high-intensity races Large variation Risk: GI discomfort Caffeine and Aerobic Exercise Helps with endurance events Improves endurance time trials by 10-15% May also help with power and resistance training (60-180 sec) Banned substance Preventing Heart Problems Physical activity Diet Fat – good and bad Fish Vegetables and fruit Fiber and whole grains Soy B vitamins Moderate alcohol consumption Modifiable Risk Factors for Cardiovascular Disease Tobacco Smoking Physical inactivity Overweight Less than recommended consumption of fruits and vegetables High blood pressure Diabetes Risk Factors You Can’t Control Heredity Race and ethnicity Age and gender Male pattern baldness Lipoprotein Profile Total cholesterol = LDL + HDL Cholesterol + Triglycerides (TG) inside lipoproteins TG can also be carried free in the blood by albumin (protein carrier) Consequences of High Blood Pressure Eye damage Heart attack Kidney failure Stroke Damage to artery walls Signs of a Heart Attack Tight ache, heavy, squeezing pain, or discomfort in the centre of the chest, which may last 30 minutes or more and is not relieved by rest Chest pain that radiates to the shoulder, arm, neck, back, or jaw Anxiety Sweating or cold, clammy skin Nausea and vomiting Shortness of breath Dizziness, fainting, or loss of consciousness So You Have Chest Pain What do the doctors do? EKG or ECG (electrocardiogram) Stress Test Angiography EKG or ECG (electrocardiogram) A simple test that detects and records the electrical activity of your heart Shows the strength and timing of electrical signals as they pass through each part of your heart Certain electrical patterns suggest whether CAD is likely, and can show signs of a previous or current heart attack However, some people with angina have a normal EKG Post Myocardial Infarction Hyperacute phase = immediately after a heart attack Fully evolved phase = a few hours to days after a heart attack Resolution phase = a few weeks after a heart attack Stabilized chronic phase is the last phase and typically has permanent pathological changes compared to a normal ECG tracing Stress Tests Exercise or medicine is given to make your heart work hard and beat fast while doctor measures blood pressure and EKG When your heart is working hard, it needs more blood and oxygen. Arteries narrowed by plaque can’t supply enough oxygen-rich blood to meet your heart’s needs Can show possible signs of CAD, such as: Abnormal changes in heart rate or blood pressure Symptoms such as shortness of breath or chest pain Abnormal changes in your heart rhythm or your heart’s electrical activity (ECG) Angiography Uses dye and x-rays to show the insides of your coronary arteries A long, thin, flexible tube (catheter) is put into a blood vessel in your ar, groin, or neck The tube is then threaded into your coronary arteries, and the dye is released into your bloodstream X-rays are taken while the dye is flowing through the coronary arteries Usually done in a hospital when you are awake The figure shows a stenosis (narrowing) in the left anterior descending coronary artery causing reversible myocardial ischemia in a patient with stable angina Treatment for Angina 1. Lifestyle Changes Better diet Physical activity Lose weight Quit smoking Slow down or take rest breaks if angina comes on with exertion Avoid large meals and rich foods that leave you feeling stuffed if angina comes on after a heavy meal Try to avoid situations that make you upset or stressed if angina comes on with stress 2. Medications Nitrates (most common – nitroglycerin): relax and widen blood vessels. This allows more blood to flow to the heart while reducing its workload Nitroglycerin dissolves under your tongue or between your cheeks and gum. Is used to relieve angina episode Blood pressure and cholesterol medicines Other medicines that: Slow the heart rate Relax blood vessels Reduce strain on the heart (ie. Diuretics) Prevent blood clots from forming Angioplasty Angina (chest pain) can occur when blood flow to the heart is reduced Angioplasty is a procedure in which a balloon is blown up in an artery to push away blockages and widen the opening of the artery to increase blood flow to the heart Coronary Graft Bypass Sometimes if the blockage is too severe, the physician will try to bypass (avoid) the blocked area using the Saphenous vein (leg) or the Internal Mammary Artery During the surgery, multiple blockages can be bypassed Minimally Invasive CABG Uses a smaller incision and accesses the heart from between the ribs. Can be done without stopping the heart The MIDCAB approach is usually reserved for cases requiring one or two bypasses; typically bypassing arteries on the front of the heart, such as the left anterior descending (LAD) coronary artery TECAB surgery: Totally endoscopic coronary artery bypass Only needs a few openings each about the size of a dime The procedure is carried out by a surgical robot (“da Vinci”) A tiny fiber optic video camera is mounted onto a robot arm and is controlled by foot pedals The procedure is performed by a surgeon operating two more mechanical arms using a joystick, or with rings the surgeon can insert his fingers into to a operate the robot’s “fingers” The entire procedure is carried out watching a video monitor Deep Vein Thrombosis Symptoms: Swollen area of the leg Pain or tenderness in the leg, usually in one leg and may be felt only when standing or walking Increased warmth in the area of the leg that is swollen or in pain Red or discolored skin Not Fatal Causes: Stagnant blood (i.e. Immobility – Prolonged sitting, casting, hospitalization, surgery, pregnancy, obesity) Hypercoagulability *coagulation of blood faster than usual) Medications (i.e., birth control, estrogen) Smoking Genetic predisposition Polycythemia (increased number of red blood cells) Cancer Trauma to the vein or leg Treatment: Anti-coagulants (heparin and warfarin) Compression stockings (swelling) Vena cava filter (surgery) Pulmonary Embolism Symptoms: Chest pain when taking a deep breath Shortness of breath Fainting Dizziness Sweating Anxiety Death Some people find out that they have deep vein thrombosis only after the clot has moved from the leg and traveled to the lung (pulmonary embolism) Treatment: Anticoagulants Oxygen May need to have surgery to remove embolism and/or filter blood of clots Stroke HEMORRHAGIC STROKE: 20% of stroke Caused by ruptured blood vessels followed by blood leaking into tissue Usually more serious than ischemic stroke Subarachnoid hemorrhage A bleed into the space between the brain and the skull Develops most often from an aneurysm, a weakened, ballooned area in the wall of an artery Intracerebral hemorrhage A bleed from a blood vessel inside the brain Often caused by high blood pressure and the damage it does to arteries ISCHEMIC STROKE 80% of stokes Caused by blockages in brain blood vessels; potentially treatable with clotbusting drugs Brain tissue dies when blood flow is blocked Embolic Stroke Caused by emboli, blood clots that travel from elsewhere in the body to the brain blood vessels 25% of embolic strokes are related to atrial fibrillation Thrombotic stroke Caused by thrombi, blood clots that form where an artery has been narrowed by atherosclerosis Most often develops when part of a thrombus breaks away and causes a blockages in a “downstream” artery Causes of Cerebral Aneurysms A cerebral aneurysm is a weak or thin spot on a blood vessel in the brain that balloons out and fills with blood More common in women than men Most cerebral aneurysms do not show symptoms until they either become very large or burst Larger aneurysms may press on tissues and nerves Causes: Congenital (Genetic inborn abnormality in an artery wall) Trauma or injury to the head High blood pressure Infection Tumors Atherosclerosis Cigarette smoking Drugs (oral contraceptives or cocaine) Symptoms of an unruptured aneurysm: Pain above and behind the eye Numbness, weakness, or paralysis on one side of the face Dialated pupils Vision changes Symptoms of a ruptured aneurysm (hemorrhage): Sudden and extremely sever headache Nausea and vomiting Stiff neck Loss of consciousness Diagnosing Cerebral Aneurysms Computed Tomography Angiography (CTA) Noninvasive X-ray to review the anatomical structures within the brain to detect blood in or around the brain. Involves the injection of contrast dye and provides the best pictures. Angiogram An invasive procedure where a catheter is inserted into an artery and passed through the blood vessels to the brain. Once the catheter is in place, a contrast dye is injected into the bloodstream and the x-ray images are taken. Magnetic resonance Angiogram (MRA) A noninvasive test, which uses a magnetic field and radio-frequency waves to give a detailed view of the soft tissues of your brain and blood vessels. Can use contrast dye. Treatment for Cerebral Aneurysms Microvascular clipping The most common treatment for an aneurysm Using general anesthesia, an opening is made in the skill, called a craniotomy The brain is gently retracted so that the artery with the aneurysm may be located A small clip is placed across the neck of the aneurysm to block the normal blood flow from entering the aneurysm The slip is made of titanium and remains on the artery permanently Shown to be high effective, and in genera, the aneurysm do not return Occlusion and Bypass Occlusion clamp off (occlude) the entire artery that leads to the aneurysm. This procedure is often performed when the aneurysm has damaged the artery Bypass a small blood vessel is surgically grafted to the brain artery, rerouting the flow of blood away from the section of the damaged artery. Sometimes accompanies the occlusion surgery. Endovascular Therapy (Coiling) Minimally invasive (no pen surgery) Once the individual has been anesthetized, the doctor inserts a hollow plastic tube (a catheter) into an artery (usually in the groin) and threads it, using angiography (x-ray), through the body to the site of the aneurysm Usually a guide wire, detachable coils (spirals of platinum wire) or small latex balloons are passed through the catheter and released into the aneurysm Tiny platinum coils are threaded through the catheter into the aneurysm, blocking blood flow into the aneurysm and preventing rupture (blood clots) This endovascular coiling, or filling, of the aneurysm is called embolization and can be performed under general anesthesia or light sedation Unclear if coiling or clipping is better Stroke Symptoms Sudden weakness or loss of strength Numbness of face, arm, or leg Loss of speech, or difficulty speaking or understanding speech Dimness or loss of vision, particularly double vision in one eye Unexplained dizziness Change in personality Change in patter of headaches Risk Factors for Strokes Age hypertension High red blood cell count Heart disease Blood fats Diabetes mellitus How to Prevent a Stroke Quit smoking Keep blood pressure under control Eat a low saturated-fat, low cholesterol diet Avoid obesity Exercise Get enough vitamin B Common Lung Diseases Asthma Chronic obstructive pulmonary disease (COPD) Bronchitis Emphysema Pulmonary fibrosis Main Types of Lung Disease Pulmonary circulation diseases Clotting, scarring, or inflammation of the blood vessels Less capable of taking up oxygen and releasing carbon dioxide May also affect heart function Ie. Pulmonary embolism, pulmonary arterial hypertension, pulmonary hemorrhage Restrictive Lung Tissue Diseases affect the structure of the lung Ie. Pulmonary fibrosis, sarcoidosis, severe obesity Like “wearing a too-tight vest”, can’t take a deep breath Airway diseases narrowing or blockages of the airways i.e. asthma, bronchitis, emphysema, chronic obstructive pulmonary disease (COPD) like “trying to breathe out through a straw” Restrictive Lung Disease Reduced lung compliance (Stiff lung) Increased work of breathe (increased lung oxygen demand) Reduced tidal volumes (shallow breaths) Increased expiratory flow rates Increased respiratory rate Non-uniform distribution of ventilation (some alveolar units are not exposed to gas) Fibrosis also impairs gas transfer at the alveolar-capillary surface Poor gas exchange Scoliosis A severe lateral curve in the spine deformation in the chest wall limited chest movement --? Reduced lung volumes Pulmonary Fibrosis Can be caused by infections, environmental agents like asbestos and silica, and chronic inflammation Sarcodosis An immune disease that causes lumps of fibrous tissues called granulomas on the skin and organs Exercise in Restrictive Lung Disease Patients Ventilation increased by increased respiratory rate as opposed to tidal volume 4x O2 requirement; Plus reduction in maximal stroke volume greater competition between respiratory and locomotive muscles for a lower total O2 supply The Airways in Asthma ~5% of population Normal airways at rest Usually bronchioles do not contribute to airway resistance because their total x-sectional area is 2000 times that of the trachea Asthma is associated with bronchoconstriction, edema and mucus Common Asthma Triggers Animals Dust Cold weather Chemicals in the air or in food Exercise Mold Pollen Respiratory infections, such as the common cold Strong emotions (stress) Tobacco smoke Asthma Outcomes Airway inflammation Airway remodeling Airway hypersensitivity Reversible airflow obstruction Lower forced expiratory volume Emergency Asthma Symptoms Bluish color to the lips and face Decreased level of alertness Extreme difficulty breathing Rapid pulse Severe anxiety due to shortness of breath Sweating Asthma Treatment Relievers (Quick Acting Bronchodilators) Controllers (Longer Acting Anti-inflammatory/bronchodilators Inhaled Corticosteroids (reducing inflammation) Asthma and Training Asthma prevalence among elite athletes is similar if not higher than in nonathletes Effect of training: No effect on resting lung function Increased cardiorespiratory fitness Quality of life? Alterations in symptoms? Chronic Obstructive Pulmonary Disorder (COPD) COPD = Bronchitis + Emphysema Normally, hypoxia in the muscle causes vasodialation Increased blood flow Increased oxygen supply BUT hypoxia in pulmonary blood vessels Vasoconstriction Pulmonary hypertension Increased afterload on right ventricle Can cause Right Ventricle Heart Failure Impact of COPD 5th leading cause of death Major cause is smoking (environment, infections) Symptoms: Shortness of breath Cough Wheezing Fatigue Weight loss Chest and stomach pain Anxiety Emphysema (smoker’s lung) Irritation lung tissue (airways and alveolar) damage Alveoli loss elastic recoil, and so the individual needs to work to push air out of their lungs How to Exercise Test Small work increments Assess oxygen desaturation Perceived dyspnea, leg discomfort (0-10 scale) Asthma or COPD patients Often have ventilatory limitations to exercise and/or oxygen desaturation Exercise Prescription in COPD Interval training higher work rates are achieved with lower symptom scores Hence, may be more comfortable in patients with severe dynamic hyperinflation Small muscle group training lowers the ventilatory burden of exercise Not limited by the central cardiorespiratory limitations, can achieve significantly higher relative work rates Resistance training (weight lifting) is a way training small muscles Combo of resistance + endurance exercise is advised in clinical rehab O2 should be monitored during initial training sessions and should be >90% Exercise in Cystic Fibrosis Aerobic Exercise is best Need to be careful about dehydration and loss of salt through sweating Drink lots of water High salt solutions (replace salt lost) What are Natural Health Products? Vitamins/minerals Homeopathy Herbal/plant remedies “Traditional” medicine Amino acids/essential fatty acids Probiotics Some personal care products Food any article manufactured, sold or represented for use as a food or drink for human beings, including chewing gum Drug includes any substance or mixture of substances manufactured, sold or represented for use in: The diagnosis, treatment, mitigation or prevention of a disease, disorder or abnormal physical state, or its symptoms, in human beings or animals Restoring, correcting or modifying organic functions in human beings or animals Disinfection in premises in which food is manufactured, prepared or kept Natural Health Product natural health products are naturally occurring substances that are used to restore or maintain good health Risks of Using NHPs Manufacturing problems Unproven claims Not enough information for people to make an informed choice Interaction with prescription drugs or other natural health products Unwanted side effects Case Study: Oscillococcinum Approved in Canada Treatment for colds and the flu Case Study: Horny Goat Weed The leaf of the plan Epimedium sagittatum Approved by Health Canada’s Natural Health Product Directorate with the following recommended use: Traditional Chinese Medicine used to tonify the kidney and fortify the yang, for symptoms such as frequent urination, forgetfulness, withdrawal, and painful cold lower back and knees Common Health Foods/Products Garlic Level III evidence – half to one clove (or equivalent) daily has cholesterol-lowering effect of up to 9% Aged garlic extract Level III evidence – 7.2g has anticlotting, as well as modest reductions in blood pressure effects Ginseng four studies suggesting a benefit on glycaemia if consumed chronically. None for improving circulation. Ginger Level II evidence – ameliorating arthritic knee pain; however less effective than ibuprofen. Chamomile has moderate antioxidant and antimicrobial acitivies, and significant antiplatelet activity in vitro Antiinflammation, antimutagenic and cholesterol-loweing activities from animals studies Human studies are limited, and clinical trials examining the purported sedative properties and chamomile tea are absent Ginkgo of questionable use for memory loss and tinnitus, but has some effect on dementia and intermittent claudication (pain/cramping in legs) St. John’s wort efficacious for mild to moderate depression, but serious concerns exist about its interactions with several conventional drugs Echinacea may be helpful in the treatment or prevention of upper respiratory tract infections, but trial data are not fully convincing Kava an efficacious short-term treatment for anxiety None of these herbal medicines is free of adverse effects. Because the evidence is incomplete, risk-benefit assessments are not completely reliable, and much knowledge is still lacking Health Canada’s Evidence for Homeopathic Medicines: Guidance Document “safety, efficacy, and quality” clinical trials to “traditional use” H1N1 From August 30 to December 29, 2009, a total of 6 951 hospitalized cases and 324 (4.7%) deaths were been reported… Pathogens and Infectious Disease Infections directly contribute to at least ¼ of all death rate. Most common infectious killers are URTIs, HIV/AIDS, and diarrhea TB, malaria and measles also kill many people in developing nations Infectious Diseases Definitions Disease a pathological condition of the body (or parts of the body) characterized by an identifiable group of signs and symptoms Infectious disease a disease caused by an infectious agent such as bacterium, virus, protozoan, or fungus that can be passed on to others Infection occurs when an infectious agent enters the body and begins to reproduce; may or may not lead to disease Host an organism infected by another organism or pathogen Virulence the relative ability of an agent to cause rapid and severe disease in a host Classifications of Agents of Infection Bacteria Viruses Protozoa Fungi Parasitic worms (helminthes) Prions Virus and Bacteria Response to Antibiotics Virus 20-400 Animals, plants, bacteria. Once in a host, viruses usually target specific tissues Unaffected by antibiotics Reproduction Uses host DNA/RNA to Size in nm Typical Host Bacteria 400 to thousands Animals, plants. Can affect whole organism Susceptible to antibiotics. Antibiotics target specific kinds of bacteria. Some bacteria are resistant Reproduces without using Structure reproduce Simple structure consisting of a core reproductive molecules (DNA/RNA), usually about 8 genes, surrounded by a protective protein coat the DNA and RNA of host Complex unicellular structure containing a variety of organelles for different functions (energy production, reproduction, protein synthesis) Hemagglutinin allows virus to enter host’s cells Neuraminidase allowed virus to escape the host’s cells SARS Severe Acute Respiratory Syndrome Spread person to person Water droplet transmission Symptoms: Fever > 38.0 C, cough, shortness of breath or difficulty breathing Examples of Viruses and Bacteria Viruses Influenza viruses Rhinoviruses and adenoviruses Herpes Papilloma virus Hepatitis Retroviruses (contain viral RNA and reverse transcriptase to make copies of viral DNA from viral RNA Bacteria Escherichia coli (Latin for from the colon) Tuberculosis Tetanus Gonorrhea Scarlet fever Diphtheria Prions A protein Bovine spongiform Encephalopathy (BSE) (Mad Cow Disease) Symptoms: abnormal behaviour, loss of coordination, tremors, rigidity, irritability, and progressive dementia Death usually occurs within 3-12 months from the onset of symptoms What Else Spreads Disease? Parasites Malaria is caused by a parasite (protozoa) called Plasmodium, which is transmitted via the bites of infected mosquitoes. How Do You Catch an Infection? Animals and insects People Food Water Infections Pathogens are everywhere Contact is generally from person to person for viruses and via persons, animals, plants, food, soil and water for bacteria Our immune system protects us somewhat from infection Chain of Infection Pathogen Reservoir Portal of exit Means of transmission Portal of entry New host What Determines if You Get a Pathogen? Is the pathogen in the environment around you? What is the amount of pathogen? Is there a point of entry? How strong is you immune system? Stopping an Epidemic Case Study: The West Nile Virus The West Nile Virus is a mosquito-borne virus that can cause encephalitis. First appeared in 1937. “polio-like” condition called sudden limb paralysis Reduced spread by reservoir Lines of Defense Physical and chemical borders Skin Mucus membranes Fluids (tears, saliva) Cilia Coughing, sneezing Lymphatic System Vessels/glands that pick up fluid, protein, lipids, etc. Contain WBCs that trap and destroy and filter pathogens Swollen glands The Inflammatory Response Following injury or infection inflammation occurs: Histamine causes blood vessels to dilate and fluid to accumulate Heat Swelling Redness Macrophages and neutrophils attack the infection Pus (collection of dead white blood cells and debris) Inflammatory Response to Bacteria 1) Damaged tissues release histamines, increasing blood flow 2) Histamine causes capillaries to leak, releasing phagocytes and clotting factors 3) Phagocytes engulf bacteria, dead cells, and debris 4) Platelets move out of the capillary to seal the wound The Immune System Two kinds of responses Innate (natural) Acquired Both recognize the invader based on the invaders antigen ANTIGEN: A marker on the surface of a foreign substance that the immune system recognized as nonself that triggers the immune response. Several cells respond INNATE IMMUNITY Refers to antigen-nonspecific defense mechanisms that a host uses immediately or within several hours after exposure to an antigen. This is the immunity one is born with Neutrophils and macrophages are cells of the immune system designed to recognize a few highly conserved structures present in many different microorganisms ACQUIRED IMMUNITY An antigen-specific defense mechanisms that takes days to become protective and are designed to remove a specific antigen This is the immunity one develops throughout life The downside to the specificity of adaptive immunity is that only a few B-cells and T-cells in the body recognize any one antigen Acquired Cell-Mediated Immunity Lymphocytes (B- and T-cells) B-cells are characterized by the presence of immunoglobulins on their surface, and upon stimulation with antigen, they are transformed into antibody secreting plasma cells T-cells have the dual function of regulating the immune response (helper T cells) and also generating specific cell mediated immunity (killer and suppressor T cells). Phase 1: Viruses invade the body through a break in the skin or another portal of entry. They take over body cells in order to replicate. Macrophages recognize the invaders by the antigens on their surface. They consume the viruses and display their antigen. Helper T cells read this information and rush to respond. Phase 2: Helper T cells trigger the production of killer T cells and B cells Phase 3: Killer T cells and natural killer cells destroy infected body cells. B cells produce antibodies that bind to viruses and mark them for destruction by macrophages Phase 4: When the danger is over, suppressor T cells halt the immune response. Memory B and T cells are reserved so that a quick response can be mounted for future invasions by this virus. Symptoms and Contamination Incubation Viruses or bacteria are multiplying Generally no symptoms but may be contagious Prodromal period Generally feel some symptoms (fever, runny nose, sore throat) Symptoms are related to the immune response Clinical period Immunization Primes the immune system for future pathogens Immune system can then quickly produce antibodies to the organism E.g. Diphtheria, Hep A and B, Influenza, MMR Reproductive and Urinary Tract Infections Vaginal Infections: Trichomoniasis Candidiases Bacterial vaginosis Urinary Tract InfectionsL Urethritis Cystitis Pyelonephritis Cancer Cycle 1) Tumor development begins with a cell gets a genetic mutation 2) Hyperplasia occurs but cells look normal. After a period of time some cells mutate further. 3) Cells continue to reproduce and descendants appear abnormal in shape (dysplasia). After time, a rare mutation that alters cell’s behavior occurs. 4) Affected cells are abnormal in growth and appearance but the tumor is still contained (in situ cancer). 5) If genetic changes allow the tumor to begin invading underlying tissues and to shed cell into lymph or blood. The escaped cells establish new tumors (metastases). These may be lethal. Stages of Cancer Cancer stage is based on the size of the tumor, whether the cancer is invasive or non-invasive, whether lymph nodes are involved, and whether the cancer has spread… Cancer specific Usually stage 0, I, II, III, IV Risk Factors for Breast Cancer Age (55 or older) Family History Age at menarche Age at birth of first child Breast biopsies Estrogen Family History About 5% to 10% of breast cancers are thought to be hereditary, caused by abnormal genes passed from parent to child If you’ve had one first-degree female relative (sister, mother, daughter) diagnosed with breast cancer, your risk is double. If two first-degree relatives have been diagnosed, your risk is 5 times higher than average BRCA1 or BRCA2 gene Abnormal CHEK2 gene Overweight/Obesity and Cancer Overweight and obese women (BMI >25) have a higher risk of being diagnosed with breast cancer compared to women who maintain a health weight, especially after menopause Being overweight also can increase the risk of the breast cancer coming back (recurrence) in women who have had the disease This higher risk may be because fat cells make estrogen and other adipokines that influence the rate at which cancers develop and grow Cancer Prevention and Nutrition Tea, coffee Berries, grapes, wine Fiber, whole grains Spices Vitamins, minerals Antioxidants, polyphenols, isoflavanoids Berries, nuts Cruciferous, vegetables Exercise and Breast Cancer Prevention Research shows a link between exercising regularly at a moderate or intense level for 4 to 7 hours per week and a lower risk of breast cancer Exercise consumes/controls blood sugar and limits blood levels of insulin and IGF1, a hormone that can affect how breast cells grow and behave People who exercise regularly tend to be healthier and are more likely to maintain a health weight and have little or no excess fat compared to people who don’t exercise Exercise Reduces Risk for Other Cancers Colorectal cancer Endometrial cancer Lung cancer Prostate cancer Breast Exam/Detection Mammography (age 40 or earlier) Clinical Breast Exam Regular Breast Self Examination Seven Warning Signs of Cancer Change in bowel habits A sore that doesn’t heal Unusual bleeding or discharge Thickening of lump in breast, testes, or elsewhere Indigestion or difficulty swallowing Obvious change in a wart or mole Nagging cough or hoarseness Reduce Cancer Risk Cancer-Smart Nutrition Tobacco Smoke Health weight Reduce exposure to carcinogens Early Detection Risk Factors for Skin Cancer Fair skin, light eyes, or fair hair A tendency to develop freckles and to burn instead of tan A history of childhood sunburn or intermittent, intense sun exposure A personal or family history of melanoma A large number of nevi, or moles or dysplastic moles Metastasis Attachment: A primary tumor attaches to a blood vessel (or lymph node) Once Cancer cells are attached, they may pass through the lining of the lymph or blood vessel. Cancer cells move into the circulation system and spread to other parts of the body, colonizing other organs. This traveling and reproducing is called metastasizing. The cancer cells may then move through the blood and lymph system to form a secondary tumor, or metastasis, at another site in the body. Treatment Depends on the stage and extent of the disease Chemotherapy Radiation therapy Surgery Other (angiogenesis inhibitors, biological to boost the immune system, targeted cancer therapies and drugs that block growth) Pedometers Measures the # of steps to determine “steps per day” – some also estimate the distance traveled and energy expended Worn on a belt or waistband and responds to vertical movements Studies of the # of steps measured by pedometer versus steps counted on a treadmill show good congruency Pedometers do not capture all PA There are varying qualities of pedometers Purposeful walking, 30 mins = 3000-4000 steps of 200 calc The average office worker takes ~5000 steps/day Pedometers provide motivation by promoting daily walking Steps Necessary for Good Health 10 000 steps/day (60-90 min of moderate PA – 4mph has an approximate energy expenditure of 400-600 kcal (depending on speed, stride length and body weight) another recommendation for health is 2 000 steps beyond your normal daily routine for weight loss, the recommendation is 20 000 steps/day Popular Exercise Class Aerobic Floor Classes Step Aerobics The Ramp Spin Cycle Yoga Pilates Yoga Developed in India ?5000 y ago, “spiritual discipline” Currently a “fad” fitness workout Concentrates on posture, breathing & “focused awareness” Aim to develop both physical & mental conditioning Pilates Developed in Germany >100 y ago Currently a “fad” fitness workout Core stabilization with concurrent dynamic exercise Aim to develop both physical & mental conditioning Exercise Facilities – Things to watch for Time and location restrictions High-pressure sales Misrepresentation in sales presentation Very little privacy Promotional gimmicks “Special Reduced Price” “Free Visits” “Before and After pictures” “Bait and Switch” “Guarantees” “Cancellation” Cost and credentials of Personal Trainers Canadian Community Health Survey Physically inactive decreased from 62 to 56% Obesity increased (13 to 16%) High blood pressure increased (19 to 25%) Diabetes increased by 25% (6.6t to 8.2%) Why Test Athletes? Establish normative standards Determine strengths and limitations Monitor development and training responses Provide information about health status Provide athlete with greater body awareness Effective Testing Relevance to sport Validity and reliability Sport specific Controlled administration Repeated regularly Performance interpretation Objectives Perform needs analysis for soccer and rowing Describe the development of testing protocols Provide overview of performance characteristics Offer views on interpreting performance outcomes Most popular sport in the world 265 million soccer players worldwide Canada 7000 clubs and 55000 teams Players ~850 000 Men ~490 000 Women ~360 000 Testing Protocol Sport characteristic Headers Changes in direction Sprints of 23 seconds 100-200 sprints/hi intensity runs 10-12K traveled Matched Test Jump ability Agility Linear sprint Repeated sprint ability Aerobic fitness Agility The ability to change directions rapidly Variety of tests to assess agility Most common to soccer: Pro-agility, Illinois, and Balsom tests Repeated Sprint Ability Various protocols: 10-12 x 20m with 10 sec rest 15-20 x 35m on a 30 sec cycle Outcomes: Average time Total time Fatigue index Rowing Cycle Catch oar(s) place in the water Drive legs extend and arms flex Finish oar(s) come out of the water Recovery arms extend and legs flex Testing Protocol Anthropometry 100 metre 60 second 2K 6K 60 minute Summary Soccer Field based testing Aerobic ability 10-12K Anaerobic ability 100+ events over 90 minutes Anthropometry-minimal importance Rowing Laboratory based testing Aerobic ability 2K Anaerobic ability – start and finish Anthropometry – extremely important Application of Fitness Assessment in Sport 1) Recognize that you are not the coach 2) 3) 4) 5) 6) Convince coach and/or team officials of importance of fitness testing Determine the fitness components and how to evaluate them Construct appropriate battery of tests Recognize practical limitations Interpretation of Feedback of Results Convince coach and/or team officials of importance of fitness testing Why Physical Fitness? 1) Decreased Work Rate 2) Decreased Concentration 3) Decreased Technical Performance 4) Decreased Tactical Judgment 5) Increased Susceptibility to Injury Uses of Test Results 1) Establish norms to aid in athlete selection 2) Provide baseline data for training 3) Monitor effectiveness of a training program 4) Motivate athlete for training and competition Determine the fitness components and how to evaluate them Knowledge/Experience of Coach Scientific Analysis 1) Time motion analyses 2) Descriptive Match Data 3) Physiological Assessment during competition and in the Lab Construct appropriate battery of tests 1) Laboratory Tests 2) Laboratory-Like Tests 3) Field Tests Interpretation and Feedback of Results 1) Equipment/Facilities 2) Support Personnel 3) Number of Athletes 4) Level of Competition 5) Cost 6) Frequency of Testing Effective Testing Relevance to sport Validity and reliability Sport specific Controlled administration Repeated regularly Performance interpretation Interpretation and Feedback of Results 1) Coach 2) Athlete NHL Entry Draft 1st week of May in Toronto top 110 players ranked by the NHL are invited All teams can come interview them Doctors – heart (ECG), lungs, vision, concussion, medical history Fitness tests – grip strength, push-pull, push-ups, curl-ups, long jump, vertical jump, bench press, Wingate, neurological assessment, VO2max on bike Tennis Fitness Testing Protocol 1. Body Composition - ideal weight, skinfolds 2. Aerobic Fitness – VO2max on Treadmill 3. Anaerobic Fitness – Cunningham-Faulkner Treadmill Run with postexercise lactate 4. Strength and Power – grip strength, leg power (vertical jump), universal (bench press, squat, etc) 5. Muscular Endurance – chin-ups, push-ups, sit-ups 6. Flexibility – overhead goniometer (shoulder, trunk and hip extension), Flexibility Stool (trunk flexion) 7. Visual Acuity – peripheral vision, depth perception, reaction time (forehand and backhand) 8. Hematology – hemoglobin, hematocrit The Female Athlete Triad Low energy availability Amenorrhea Osteoporosis Christy Henrich 1988 – at a meet in Budapest a U.S. judge told Christy Henrich one of the world’s top gymnastics, that she was too fat and needed to lose weight if she hoped to make the Olympic squad Age – 16 years old Height – 147cm (4’10”) Body mass – 42kg (93lbs) BMI – 19.8 kg/m2 Resorted to anorexia and bulimia to control her weight Lowest body mass 22kg (47lbs) BMI – 9.8 kg/m2 Only July 2th, 1994, at the age of 22, she died of multiple organ failure Heidi Guenther Ballet dancer told to lose 5 pounds by her ballet company at 5’5” and 115 lbs Struggled with anorexia Died at the age of 22 weighing 93 lbs when her heart suddenly stopped Definitions – Reproductive Eumenorrhea ovulatory cycle with menses occurring every 24-34 days (10-13 cycles per year) Oligomenorrhea irregular menses occurring more than 35 days and less than 90 days apart Amenorrhea – no senses for at least 90 days Alex DeVinny 2003 State champion in 3200 m at 9 had issues with eating at 17 had not yet began menstruating at 20 died of cardiac arrest as a consequence of anorexia (weight 32kg) Bone Regulation Osteoclasts cells that break down bone Osteoblasts cells that build bone Resting Bone surface resorption reversal bone formation mineralization Importance of Estrogen Suppresses bone resorption Allows skeleton to ‘hear’ physical activity Risk factors for triad Calorie restriction Exercise for prolonged periods of time Involved in sport emphasizing body appearance Pressure to lose weight to improve performance Competitive nature Complete involvement with sport Trains even when injured or sick Traumatic event, injury, poor performance, changing in coaching personnel Other life stressors Symptoms of Triad Menstrual irregularities Fatigue Problems controlling body temperature Problems with sleep Reduced bone mass Frequent injuries Bona Fide Occupational Requirement (BFOR) Physically demanding occupations in which failure to perform the job or ineffective job performance can result in loss of life or property 1) The standing must be for a purpose rationally connected to job performance 2) The standard must have been adopted by the employer in good faith and belief that it was necessary for the fulfillment of the work-related purpose 3) The employer must show that the standard is reasonably necessary to accomplish the work-related purpose (demonstrate that it is impossible to accommodate the worker without imposing undue hardship on the employer) Workers’ Compensation Ontario’s Workplace Safety and Insurance Board (WSIB) decides whether or not a worker receives compensation, and decides what the worker gets compensation for. Depending on the injury or illness, a worker can receive: 85% of lost wages Health care costs Transportation costs to medical treatment Payment for pain and suffering Return to work plan