SHR Story Board June 19 2006
advertisement
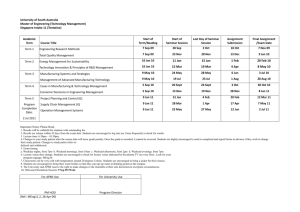
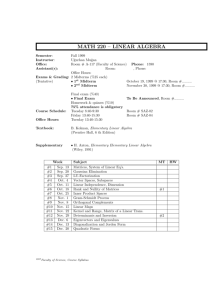
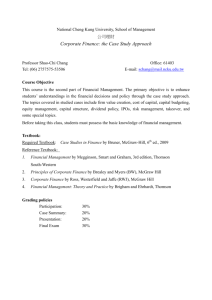
Western Node Collaborative Saskatoon Health Region Medication Reconciliation Background • Saskatoon Health Region: – largest health region in Saskatchewan – provides services to almost 300,000 local residents and thousands of others from across the province who come to Saskatoon for specialized health services. – On any given day, approximately 35% of hospital care in Saskatoon is provided to people living outside the Health Region. – As an academic health sciences centre, the Health Region provides learning opportunities to future health care providers and participates in research that will build knowledge and improve care. SHR Medication Reconciliation Project Structure Advisory Committee Steering Team Jean Morrison (Executive Sponsor), Sandra Blevins, Brenda Thiessen, Janet Harding, Candice Bryden Project Co-Chairs Jackie Mann Barb Evans Team Leads P St. Elizabeth’s Monique Bollefer (Lead) Russom Ockbaghzi Ellen Kachur Yvonne Berscheid Brenda Hantke Bev Weyland RUH Pediatrics Bernie McDonald (Lead) Garth Bruce Val Gerlach Shelley Peacock Margo Elmgren r o Quality Services Candice Bryden Gerry Belton j e c t SPH 6th Medicine Barb Kirkland (Lead) Cheryl Fransoo Carmen Hampton Trina Mucha Susie Hoeppner Donna Strilaef Caroline Westman Joy MacLaughlin Norma Engele Karen Wormsbecker Maureen Preston Holly Mansell Judy Klassen Joanne Kappel T Janice Seeley Marlene Strenger e a m Physician Champion (vacant at present) s RUH 5000 Lilah Weinberger (Lead) Leah Gilmore Doris Smith Eva Lehnert Thiel Noelle Rohatinsky Kathy Bue Renee Kennedy Crystal Richter SCH 4300 Jane Richardson (Lead) Mark Sheridan Audrey Sereda Tess Gieg Nadine Clarke Marie Gifford Shannon Stone Background • Pilot sites for medication reconciliation project include: – Surgery 5000, Royal University Hospital – Pediatrics, Royal University Hospital – Gynecology / PAC, Saskatoon City Hospital – 6th Medicine, St. Paul’s Hospital – St. Elizabeth’s Hospital, Humboldt (rural site) Background • Rationale for improving – Enhanced patient safety • What are you trying to improve? – Clarity and completeness of medication histories and orders from admission to discharge – Reduce medication history and ordering workload Background • Important dates: – Start date: October / November 2005 – Region wide target implementation dates: • Admission: December 2006 • Transfer and discharge: Spring 2007 • Link with SK Health Pharmaceutical Information Program (PIP): June 2007 Background • Why? – – – – Evidence for improving patient safety is compelling Requirement for CCHSA accreditation CEO and Senior Leadership completely endorses Enhances efficiencies; eliminates duplication of workload – Key component of seamless care strategies • Resources: – No dedicated resources – Group of interested, enthusiastic health care professionals agreed to participate Aim • Purpose: Improve patient care by reducing adverse drug events through medication reconciliation • Scope and Boundaries: – Pilot areas selected. Focus on admission process initially. • Improvement Objectives (Admission): – Overall: To reduce adverse drug events and patient harm through the implementation of medication reconciliation on admission throughout SHR. – Pilot Aims: • Reduce # unintentional discrepancies by 75% in 12 months • Reduce # undocumented intentional discrepancies by 75% in 12 months • Increase overall success at reconciling medications by increasing the Medication Reconciliation Success index by 75% in 12 months Goals • Admission to Discharge: – Develop 1 form for admission medication reconciliation for use in SHR. • Form to serve dual purpose of physician’s order form and medication history documentation tool. – Develop 1 process for admission medication reconciliation in SHR. – Utilize PIP to generate on-line admission medication reconciliation form – Modify the current business process to integrate the preadmission data with patient’s acute care medication profile – Develop a new process where automation will generate a patient medication profile on transfer and discharge Changes Tested • Preadmission Medication List Physician Order Form – Focus groups (Pharmacy, Nursing, Physicians) – Satisfaction survey with each PDSA cycle – Changes made to content and design based on feedback • Medication reconciliation process – Focus groups – Satisfaction survey with PDSA cycle #1 • Test effectiveness of and reaction to medication reconciliation form – Survey – Missing information check-list – BPMH Results: Run Charts of Key Measures Pediatrics – Includes OTCs and Herbal Products (n=6) Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 1.20 1.00 0.80 0.60 0.40 0.20 0.00 Nov 2005 Mean 1.0 Mean Number of Undocumented Intentional Discrepancies Month Actual Goal 2.0 Mean Number of Unintentional Discrepancies 0.60 Mean 0.50 0.40 0.30 0.20 0.10 Month Actual Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.00 Goal Month Actual Goal Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 120% 100% 80% 60% 40% 20% 0% Nov 2005 Percentage 3.0 Medication Reconciliation Success Index Results: Run Charts of Key Measures Pediatrics – OTCs and Herbal Products Removed (n=4) 1.0 Mean Number of Undocumented Intentional Discrepancies 0.80 Mean 0.60 0.40 0.20 Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.00 Month Actual Goal 2.0 Mean Number of Unintentional Discrepancies 0.60 0.50 Mean 0.40 0.30 0.20 0.10 Month Actual Goal Month Actual Goal Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 120% 100% 80% 60% 40% 20% 0% Nov 2005 Percentage 3.0 Medication Reconciliation Success Index Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.00 Results: Run Charts of Key Measures 6th Medicine – Includes OTCs and Herbal Products (n=2) Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 3.00 2.50 2.00 1.50 1.00 0.50 0.00 Nov 2005 Mean 1.0 Mean Number of Undocumented Intentional Discrepancies Month Actual Goal 2.0 Mean Number of Unintentional Discrepancies 2.50 Mean 2.00 1.50 1.00 0.50 Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.00 Month Actual Goal Month Actual Goal Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 120% 100% 80% 60% 40% 20% 0% Nov 2005 Percentage 3.0 Medication Reconciliation Success Index Results: Run Charts of Key Measures Gynecology / PAC – includes OTCs and Herbal Products (n=4) 1.0 Mean Number of Undocumented Intentional Discrepancies Mean 2.50 2.00 1.50 1.00 Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.50 0.00 Month Actual Goal 2.0 Mean Number of Unintentional Discrepancies 2.50 Mean 2.00 1.50 1.00 0.50 Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.00 Month Actual Goal 100% 80% 60% 40% Month Actual Goal Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 20% 0% Nov 2005 Percentage 3.0 Medication Reconciliation Success Index Results: Run Charts of Key Measures St. Elizabeth’s Hospital – includes OTCs and Herbal Products (n=1) 1.0 Mean Number of Undocumented Intentional Discrepancies Mean 1.50 1.00 0.50 Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.00 Month Actual Goal 2.0 Mean Number of Unintentional Discrepancies 2.50 Mean 2.00 1.50 1.00 0.50 Month Actual Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.00 Goal Month Actual Goal Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 120% 100% 80% 60% 40% 20% 0% Nov 2005 Percentage 3.0 Medication Reconciliation Success Index Results: Run Charts of Key Measures Surgery 5000 – includes OTCs and Herbal Products (n=11) Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 1.20 1.00 0.80 0.60 0.40 0.20 0.00 Nov 2005 Mean 1.0 Mean Number of Undocumented Intentional Discrepancies Month Actual Goal 2.0 Mean Number of Unintentional Discrepancies 2.50 Mean 2.00 1.50 1.00 0.50 Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 Nov 2005 0.00 Month Actual Goal Month Actual Goal Dec 2006 Nov 2006 Oct 2006 Sep 2006 Aug 2006 Jul 2006 Jun 2006 May 2006 Apr 2006 Mar 2006 Feb 2006 Jan 2006 Dec 2005 120% 100% 80% 60% 40% 20% 0% Nov 2005 Percentage 3.0 Medication Reconciliation Success Index Keys to Success & Lessons Learned • Major Keys to Success – Enthusiastic and committed Advisory, Steering, and Ward team members – 1:1 and small group educational sessions with staff – Increasing number of staff engaged in the process • Barriers – – – – Dedicated resources Staff buy-in on certain pilot areas Process – obtaining a complete and accurate medication history Timelines – balance between Safer Healthcare Now / Quality Improvement Methodology and Accreditation deadline – PDSA cycle turn around time Keys to Success & Lessons Learned • Lessons learned to date about these changes – Large scale change in process required. Not as easy as anticipated. – Preadmission Medication List Physician Order Form appears to be working well. – Medication reconciliation process requires further development. • Further education on “How to Perform a Medication History” required – Education sub-committee formed Next Steps • Changes we are planning on testing to help us achieve our goals: – Effect of a standardized method for providing education – Ability of staff to take a complete and accurate medication history – Use of PIP to generate on-line Preadmission Medication List Physician Order Form – Use of automation to generate a patient medication reconciliation and order form on transfer and discharge Contact Information • Barb Evans – barb.evans@saskatoonhealthregion.ca – Phone: 306-655-2268 • Jackie Mann – jackie.mann@saskatoonhealthregion.ca – Phone: 306-655-7946 • Janice Seeley – janice.seeley@saskatoonhealthregion.ca – Phone: 306-655-6832 Process Map – Pre-Assesssment Clinic