PID fact sheet - WordPress.com
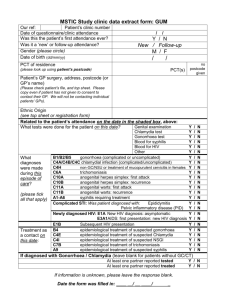
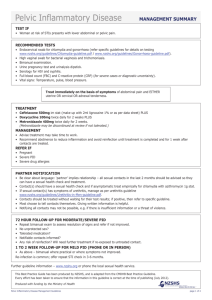
advertisement

PID Definition MO’s Causes Risk factors Complications Assessment Investigation Treatment Syphilis Spread of 1Y lower genital tract infection to upper (inc. endometritis, salpingitis, tubo-ovarian abscess, peritonitis) Non-sexual: mixed pathogens from vaginal flora; anaerobes, facultative bacteria, mycoplasma, ureaplasma, gut coliforms (E coli, H influenzae); PV discharge not usually STD (candida most common cause, bacterial vaginosis) Sexual: Chlamydia - most common cause of cervicitis; most common in hetero; usually asymptomatic in women Intracellular parasite; incubation 1-3/52 or longer More watery discharge, less painful than gonorrhoea; can also cause proctitis / prostatitis Lymphogranuloma venereum (males get vesicles/ulcers on genitals inguinal buboe after 1-4/52 fuse, breakdown, discharge) Gonorrohea – rates increasing; more common in homos / Maoris etc… / overseas sex; 50% have co-existant chlamydia; incr penicillin and quinolone resistance G-ive intracellular diplococci; incubation 3-7/7 Urinary Sx and penile discharge in men; 10-20% of untreated infections become PID; disseminated in 3% Septic arthritis (2x more common in women, occurs in 0.2%, onset 3-17/7 after infection, may be preceded by migratory polyarthritis; 75% poly, 80% asymmetric) Rash (in 2/3; petechiae / painful red papules on digits; may become vesicular / pustular grey necrotic centre, often on haemorrhagic base; usually <20 lesions) Can also cause pharyngeal, anal, conjunctivitis, tenosynovitis, meningitis, myocarditis, pericarditits Trichomonas Gardnerella; often polymicrobial Direct; haematogenous (TB, mumps); iatrogenic (IUCD, RPOC); >50% have no cause detected for cervicitis Incr with sexual activity; decr with progesterones and pregnancy (esp after 12/40) Infertility (12-50%; 10% after first episode); chronic salpingitis (25%); chronic pain, adhesions, dysparaeunia (20%), ectopic (12-15% higher incidence; incidence 1:120 normally, 1:16 with PID); tubo-ovarian abscess (5% mortality if rupture; occurs in 1/3 hospitalised patients); infertility (risk doubles with each infection; 2 infections = 20%, 3 infections = >50%); Fitz-Hugh-Curtis syndrome (transcoelemic spread of inflammatory peritoneal fluid to subphrenic and subdiaphragmatic spaces) History: 90% pelvic pain (usually bilateral); 75% vaginal discharge; >30% irregular PVB; systemic toxicity Examination: poor sens and spec; low grade fever, adnexal mass Bloods: WBC >10 in 50% Swab: gonorrhoea culture (urethral or endocervical) 97% sens gram stain 50% sens PCR 99% sens and spec chlamydia culture 95% sens, 99% spec; self collected samples and urine samples as good Urine: gonorrhoea PCR 90% sens, 99% spec Chlamydia PCR in males USS: if abscess suspected (ie. Toxic, asymmetrical findings) Laparoscopy: will be +ive in 50% of those diagnosed with PID clinically Commence if: lower abdo tenderness + uterine and bilateral adnexal tenderness + cervical motion tenderness Admit if: toxic; severe pain; unable to tolerate PO meds; pregnancy; pre-pubertal; HIV +; poor likelihood of compliance; IUD or recent instrumentation Sexually acquired: Mild Azithromycin 1g PO single dose / doxycycline 100mg BD + metronidazole 400mg BD for 14/7 If gonorrhoea (always trt if community incidence high + ceftriaxone 250mg IM/IV stat Severe Doxycycline + metronidazole + ceftriaxone (continue for 48hrs after Sx improve) PO Non-sexually acquired: Mild Augmentin + doxycycline Severe As per septicaemia (or treat as severe sexual) Septicaemia Ampicillin 2g IV Q6h + metronidazole 500mg BD + gentamicin 4-6mg/kg OD Puerpueral Mild Augmentin BD 5-7/7 (add roxithromycin 300mg OD / clindamycin 300mg TDS if ongoing >48hrs) Severe As per septicaemia Pregnant / Bfing Roxithromycin instead of doxy If penicillin allergy IV gentamicin + clindamycin Gonorrhoea, no PID Ceftriaxone (covers gonorrhoea) + doxycycline 100mg BD 7/7 or azithromycin 1g single dose Chlamydia, no PID Doxycycline 100mg BD 7/7 or azithromycin 1g single dose (both have 95% cure rate) Remove IUCD or RPOC; consider sexual abuse; trt sexual contacts (partner infected in 40%); counselling; always FU at 72hrs; refer to sexual health clinic; abstain from sex at least 2/52; candida prophylaxis; gonorrhoea and chlamydia = reportable disease Very uncommon (incr in homos); usually detected in latent phase Treponema pallidum: spirochete; STD 1Y syphilis: 2-6/52 after contact 1 firm, nontender, raised red lesion (chancre) on penis, cervix, vagina, anus in 70% men, 50% women; up to 7eral cm diameter; erodes to create shallow based ulcer; regional LN heals in 3-6/52 without trt 2Y syphilis: 2-10/52 after 1Y, in 75% dissemination in skin and mucocutaneous tissues; lasts several weeks latent phase 1. maculopapular / scaly / pustular lesions on soles of feet / palms – discrete red/brown spots <5mm diameter 2. condylomata lata on moist areas (eg. Anogenital / axilla / inner thigh) – broad based, elevated plaques, painless, highly infectious 3. silver/gray superficial erosions on mm's (esp mouth / ext genitalia / oropharynx) ulcerate – these are most infectious 4. fever, malaise, weight loss, LN’s, arthralgia 5. Maybe: asceptic meningitis (1-2%), hepatitis, nephrotic syndrome 3Y syphilis: in 1/3 untreated after >5yrs 1. CV syphilis: aortitis --> dilatation of aortic root and arch --> aortic valve regurg, aneurysms; accounts for 80% 2. Neurosyphilis: may be asymptomatic (1/3); chronic meningovascular disease, tabes dorsalis, general paresis; dementia, psychosis, CN palsy, SC syndrome; in 5-10% 3. Benign 3Y syphilis: gummas in various sites; white/gray rubbery/ single/multiple/small/large nodular lesions due to delayed hypersensitivity; mostly in bone (--> pain, tenderness, swelling, pathological fracture), skin, subC tissue; mm of URT and mouth, testes; rarely causes destructive ulcerative lesions Congenital syphilis: during 1Y/2Y in mother; 25% intrauterine / perinatal death --> infantile (early): first 2yrs; nasal discharge and congestion; desquamating / bullous rash --> sloughing of skin (esp hands, feet, mouth, anus); hepatomegaly, skeletal abnormalities (syphilitic osteochonritis and periostitis – esp nose with saddle nose deformity and lower leg --> new bone growth on ant tibia --> sabre shin) --> tardive (late): later; occur in >50% untreated; Hutchinson triad: notched central incisors (may be screwdriver shaped), interstital keratitis (or choroiditis) with blindness, deafness due to VIII injury (and optic nerve atrophy); skeletal, neurological and facial abnormalities Investigation: identified on MC+S of 95% chancres; VDRL 80% sens (>95% in stage 2 and 3), 1-2% false +ive if +ive, need to confirm with treponeal ab test (80% sens 1Y, 100% later) Mng: penicillin (doxycycline if allergy) Notes from: Dunn, Cameron, TinTin