208Kb - Shifting the Balance of Care
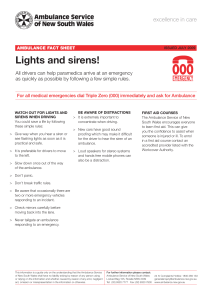
advertisement

Reflecting on the presentations: Share experiences from your own Health Board area / locality / site in relation to the part of the patients’ flow discussed: What works well in your area / locality / site? What and who have been the drivers for this? What could work better? Who needs to be engaged? Where local practice could be improved, consider how to utilise the evidence / learning from the workshop to influence change. IMPROVING UNSCHEDULED PATIENT FLOWS INTO AND OUT OF ACUTE CARE Mr George McLean, General Manager G-MED OOH, Acting Unit Operations Manager A&E and Unscheduled Care Q. “What can the Out of Hours System do to help?” A. “As part of the wider integrated unscheduled care system, there is a lot more we can do” Patient scenario •89yr old female care home resident •Hx Dementia and 3/7 UTI •01.00hrs, found unresponsive but breathing •Call NHS24 – upgraded to 999 •Blue light ambulance / t-fer 20 miles to A&E •Extended wait at A&E overnight (busy) •Admission to acute hospital The Quality Strategy /Ambitions •Person-centred? •Clear communication? •Safe? •Effective? •Collaboration between clinicians, patients and others? •Continuity of care? •Clinical excellence? What can OOH systems do to help? •Utilisation of special notes/ ECS/ePCS/ anticipatory care plans • Professional to professional line •S-BAR handover SAS to OOHs •Transfer protocols A&E to OOHs •Patient review service •Palliative care case management •Primary Care decision support •Collaborative working on frequent admissions •Co-ordination of OOH nursing care •Emergency Medical Practitioners at front door •Utilisation of respite facilities and Community Hospitals SBAR Reporting For good communication about patients between health professionals, use the SBAR tool when calling: SITUATION Patient ID? Date of birth Name Current location & home address Telephone number Own GP / Practice Why has the ambulance service been called and what has happened to the patient? BACKGROUND What is the patient’s past medical history? What are the patient’s circumstances i.e. alone, bedridden, disabled etc. Is the patient receiving palliative care? Are there any discharge letters / care plans. ASSESSMENT What are the vital signs? Pulse A.M.P.L.E Temperature Blood Pressure Respiratory rate (12 lead ECG findings – see below) SpO2 Glasgow Coma Score Blood Glucose Measurement Pain Score What are the other relevant findings on examination? What is the ambulance crew diagnosis and what treatment has been given? RECOMMENDATION What would the Ambulance crew like “Out of Hours” to do? Doctor phone ambulance crew now / doctor phone patient / centre consult / home visit What is the clinical priority time? < 1 hr, < 2hrs, < 4 hrs Ask if there is anything else you should do? Record name and contact number of health professional you are talking to. Remember to document the call Patient scenario •89yr old female care home resident • Daytime service planning? • Anticipatory care plan? • Care staff induction, training and support? •Hx Dementia and 3/7 UTI • Treatment plan? • Review of patient? •01.00hrs, found unresponsive but breathing • Unscheduled care to Planned care? •Call NHS24 – upgraded to 999 • Triage, information available from caller? • Special notes, Hx, DNACPR, ECS, ePCS? • Outcome? Patient scenario •Blue light ambulance / t-fer 25 miles to A&E • What options available to Paramedic? • Could the patient be considered for OOHs? •Extended wait at A&E overnight (busy) • Is this the most appropriate location for care? • Direct admission to ward? •Admission to acute hospital • Was this appropriate/ avoidable? • What alternatives are available? • Patient record sent to GP Discussion and Questions? Thank You • Reflecting on the presentations: • Share experiences from your own Health Board area / locality / site in relation to the part of the patients’ flow discussed: • • • • What works well in your area / locality / site? What and who have been the drivers for this? What could work better? Who needs to be engaged? • Where local practice could be improved, consider how to utilise the evidence / learning from the workshop to influence change.