Eating Disorders in Adolescence
advertisement

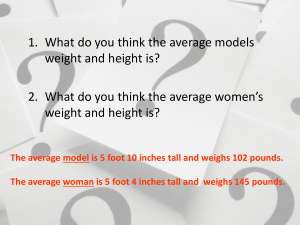
Eating Disorders in Adolescence American Society for Adolescent Psychiatry March 29, 2014 Steven Crawford, M.D. Center for Eating Disorders at Sheppard Pratt S Eating Disorders and Co-morbidity S Depression S Anxiety S Substance Use Disorders S Personality Disorders S Safety Co-morbidity: Depression S 30-50%; 70% lifetime prevalence S Affects motivation, psychological accessibility S Starvation status produces similar affective, cognitive and somatic symptoms S Antidepressants do not work as well S Psychological treatments do not work as well Co-morbidity: Anxiety S Anorexia Nervosa: S 60% S More obsessional; harm-avoidant S Bulimia Nervosa: S 57% S More outgoing but significant stress in socializing S Eating disorder symptoms in both groups tend to bind anxiety. Anxiety tends to get worse with symptom reduction Co-morbidity: Substance Use Disorders S AN: 27%; BN: 55%; BED: 23% S Substance abuse develops at various stages of illness S Amplifies impulsivity and mood instability S Increases nutritional, hepatic, GI, cardiac and neurological consequences Co-morbidity: Personality Disorders S Deficits in sense of self commonly seen in narcissistic and borderline disorders S Difficulties with regulation of self- esteem and affect S Problems with separation and autonomy S Anorexia: obsessive compulsive, avoidant, dependent S Bulimia: borderline, narcissistic Other Than Co-morbidity, Why Screen? S Prevalence S Morbidity and Mortality S Outcomes Prevalence S In the United States: • 10 million women and 10 million men suffer from clinically significant ED at some time in their life • Rate of development of new cases of ED increasing since 1950 • Rise in incidence of anorexia in young women (age 15-19) each decade since 1930 (0.9% of population) • Incidence of bulimia in women (age 10-39) tripled from 1988-1993 (1.5% of population) Morbidity and Mortality S Serious health consequences including heart failure and other severe cardiac conditions, kidney failure, osteoporosis and gastrointestinal disorders. S Binge eating (the most common eating disorder) is associated with obesity, heart disease, gall bladder disease and diabetes. S According to the NIMH, 1 in 10 women with anorexia nervosa dies of starvation, cardiac arrest, or some other medical complication. The risk of death among teenage girls with anorexia is 11 times greater than in disease-free adolescents. Outcome S Significant functional impairment S High rates of suicide S Earlier intervention improves the prognosis A Few Guiding Principles S Individuals with eating disorders come in all sizes and shapes. S Weight is not a good proxy for eating or exercise practices. High weight patients may not be getting enough nutrition and normal weight patients may be engaging in unhealthy practices to maintain a weight lower than one within their own genetic range. S Athletes may be engaging in very unhealthy disordered eating and eating disorder behaviors A Few Guiding Principles S Weight loss is not always a sign of health. An individual could be developing a serious medical problem or could be engaging in life threatening behavior in the pursuit of weight loss S It needs to be taken seriously when parents raise concerns. A single consultation about a child’s eating behavior or weight/shape concerns is a strong predictor of the presence or development of an ED How to Screen S S S Do you make yourself Sick because you feel uncomfortably full? S C S Do you worry you have lost Control over how much you eat? S O S Have you recently lost more than One stone (6.35 kg) in a three-month period? S F S Do you believe yourself to be Fat when others say you are too thin? S F S Would you say Food dominates your life? Additional Screening Questions S Many people have concerns about food. Please tell me about your eating habits. Do you worry about your eating or do you think that others do? S Some people have concerns about their weight. Please tell me how you feel about your body and weight? S Some people have trouble with eating to the point of discomfort or until they are uncomfortable. Please tell me if this has been a problem for you Screening Questions for Parents S Does your child make negative remarks about his or her body? S Have you noticed any changes in food related habits? If so, what? S Are you concerned about your child’s weight, eating or exercise habits? S Does your child eat regular meals with the family? S Does your child have an increased interest in food-related activities, but with decreased intake of food? Frequency of Screening S A national representative of 10,123 adolescents between ages 13 to 18 screened for eating disorders S A majority, 88%, of those that screened positive for eating disorders had some contact with service providers, mental health specialty care, school services, or general medical services S Only a minority, as low as 2%, talked to a professional about their eating/weight problems How Common Is It? • By age 6, girls especially express body image or weight concerns • 40-60% elementary school girls (ages 6-12) are concerned about their weight or becoming too fat • Up to 60% female teens diet regularly • Over 50% teens exercise in order to improve shape or lose weight • Approximately 45% female teens smoke cigarettes to control weight When Does It Become Disordered Eating? S Nutritional adequacy of diet S Impact of feeding/eating disturbance on weight, growth, and physical development S Impact of feeding/eating disturbance on social and emotional development/function S Impact of feeding/eating disturbance on interaction with caregiver on family function Eating Disorders: DSM-5 S Anorexia Nervosa S Bulimia Nervosa S Binge-Eating Disorder S ARFID S Pica S Rumination Disorder Anorexia Nervosa S Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health. S Intense fear of weight gain or persistent behavior that interferes with weight gain S Body Image Disturbance with undue influence of body weight/shape on self-evaluation Emotional and Behavioral Signs of Anorexia Nervosa • • • • • Refusal to eat Denial of hunger Excessive exercise Eating only a few certain "safe" foods, usually those low in fat and calories Adopting rigid meal or eating rituals, such as cutting food into tiny pieces or spitting food out after chewing Physical Signs of Anorexia Nervosa S Emaciation S Brittle nails S Hyperactivity S Hair loss on scalp S Bradycardia S Lanugo hair S Hypotension S Brittle hair S Dry skin S Edema S Yellow skin, especially S Cyanotic and cold hands palms and feet Growth Chart Bulimia Nervosa S Recurrent episodes of binge eating S Recurrent inappropriate compensatory behavior designed to prevent weight gain S Binge-Purge episodes occur once per week for 3 months S Self-evaluation is unduly influenced by body shape and weight S No evidence of Anorexia Nervosa Behavioral Signs S Frequent use of bathroom after meals S Unexplained disappearance of food from kitchen S Ongoing observed consumption of large quantities of food without associated weight gain S Evidence of emesis on toilet Physical Signs of Bulimia Nervosa S Calluses on the back of the hand S Salivary gland hypertrophy S Erosion of dental enamel S Mouth ulcers S Periodontal disease S Hematemesis S Dental caries S Edema S Petechiae S Abdominal bloating S Perioral irritation Binge Eating Disorder S Recurrent episodes of binge eating S Binges are associated with 3 or more of the following: S Eating rapidly S Eating until uncomfortably full S Eating large amounts when not hungry S Eating alone due to embarrassed with how much one eats S Feeling disgust, guilt or depressed after overeating S Marked distress during binge eating S Binge episodes occur once per week for three months S Binge is not associated with recurrent use of inappropriate compensatory behavior Binge Eating Disorder Epidemiology S Lifetime prevalence rate in women of 3.5% S Lifetime prevalence rate in men of 2.0% S Prevalence is as high as 30% in individuals seeking bariatric surgery ARFID S Apparent lack of interest in eating or food, avoidance based on sensory characteristics of food; concern about aversive consequences of eating and this concern results in significant weight loss or failure to achieve expected weight gain or faltering growth in children; significant nutritional deficiency; marked interference with psychosocial functioning S The disturbance is not explained by lack of available food or by a culturally sanctioned practice. S No body image disturbance. S No concurrent medical condition or mental disorder responsible for eating disturbance. Classification Other Specified Feeding or Eating Disorder Anorexia Nervosa Binge-Eating Disorder O Bulimia Nervosa Unspecified Feeding or Eating Disorder Etiologic Factors S Psychological S Personality S Sociocultural S Genetic S Family S Biologic Psychological S Separation-Individuation S Retreat from puberty/Avoidance of maturational challenges S Phobic avoidance disorder S Issues of control S Low self-esteem Sociocultural S Kids watch up to 5 hrs of TV/day S Up to 6-7 hours of total media exposure (TV, Internet, etc) daily S Body image is significantly more negative after viewing thin media images S Facebook and social media Family S No longer believed to be an “anorexogenic” or a “psychosomatic” family S There are believed to be family dynamics that develop in presence of eating disorder that serve as maintenance mechanisms S Correlation with a parenting style marked by high concern Personality Traits S Perfectionism S Harm-avoidant Genetic S Eating disorders run in families S Twin concordance studies is greater for monozygotic compared to dizygotic twins S Anorexia nervosa: 31-76% S Bulimia nervosa: 28-83% S Molecular genetic studies point to the serotonin 2A receptor gene Biologic S 1950: Starvation Study, Keys et al 36 young healthy, psychologically stable men were restricted to 50% of their normal intake leading to 25% weight loss. Effects of Starvation: Emotional and Social Changes S Physical S Emotional S Social S Cognitive S Attitudes and Behaviors toward Food Multidetermined Nature of Eating Disorders Eating Disorders Treatment S Only one-third of people with AN in the community receive mental health care S Only 6% of people with BN receive mental health care S 80% of individuals with severe eating disorders do not receive intensity or duration of care warranted by their symptoms Eating Disorder Treatment S Due to ambivalence regarding recovery, outside support/decision making may be necessary regardless of age S Engage families and decrease sense of guilt/blame Eating Disorder Treatment S Symptom Management S Medical Management S Therapy Symptom Management S Nutritional Rehabilitation: normalize eating pattern with weight gain of 0.2kg/day S Nutritional Stabilization: normalize eating pattern with decreased focus on weight S Increased tolerance of sensation of fullness S Increased tolerance of body image dissatisfaction S Always assess for psychiatric risk, including suicidal ideation Medical Management S Collaboration between psychiatrist, non-physicians and primary care physicians S Regular consistent weigh-ins S Ongoing laboratory/vital signs monitoring S Annual bone densities S Regular dental exams Therapy S Cognitive-Behavioral Therapy S Interpersonal Psychotherapy S Dialectical Behavioral Therapy S Family Therapy Indication for Hospitalization S Severe malnutrition (wt less than or equal to 75% IBW) S Dehydration S Electrolyte disturbances S Cardiac dysrhythmias Indication for Hospitalization S Physiologic instability S Bradycardia (heart rate < 50) S Hypotension ( BP < 80/50) S Hypothermia (body temperature < 96) S Orthostatic changes in pulse or blood pressure S Acute complications of purging S hemetemesis Indication for Hospitalization S Acute psychiatric emergencies S Suicidal ideation S psychosis S Co-morbidity interfering with treatment of eating disorder S Depression S Obsessive-compulsive disorder S Severe family dysfunction Family Based Treatment S Highly focused, staged treatment S Emphasis on behavioral recovery rather than insight and understanding S This approach might indirectly improve family functioning S Supports gradual increased independence from therapy Principles of Family Based Treatment S Agnostic view of cause of illness S Initial focus on symptoms S Parents are responsible for weight restoration S Non-authoritarian therapeutic stance S Separation of child and illness (Externalization) Collaborative Care Model S Janet Treasure et al Janet Treasure PhD, FRCP, FRCPsych Series of workshops designed to educate carers on the key skills that clinicians have in treating eating disorders so that there is more continuity in care between the treatment setting and at home. Collaborative Care Model S Address universal needs of carers: S Connection with other carers S Support S Skills training Collaborative Care Skills S Motivational Interviewing S Trans-theoretical model of change S Self-Care S Behavior Analysis Pharmacotherapy: Anorexia Nervosa S SSRI’s S Not for treatment of Anorexia Nervosa S Primarily beneficial in the treatment of co-morbid diagnoses Pharmacotherapy: Anorexia Nervosa S Olanzapine S 3 open label trial S Benefit in weight gain and cognition as well as improved body image S Quetiapine S 2 open trials S Improved results in psychopathology testing, not significant for weight gain S Risperdone/Aripriprazole S Positive case reports Treating the Adolescent With Bulimia Nervosa S CBT is most studied S Effectiveness well established in BN S Preliminary studies suggest effectiveness in AN S Focus is on changing eating behaviors and attitudes that maintain eating disorder S IPT and DBT have been demonstrated to be effective Pharmacotherapy: Bulimia Nervosa S Fluoxetine S Considered the gold standard of pharmacotherapy for BN S Dosing at 60mg significantly more effective than 20mg S Anxiolytics S May be beneficial in affect modulation S Potential for behavioral disinhibition and worsening of binge- purge cycle Conclusions S AN and BN are serious mental illnesses with significant medical and psychiatric morbidity and mortality, regardless of the individual’s weight S Full resolution of symptoms is an essential goal of treatment. This includes: S Nutritional rehabilitation S Weight restoration and stabilization S Resumption of menses (where appropriate) S Cessation of binge eating and/or purging behaviors Conclusions S Family treatment should be recommended for virtually all adolescents with AN S CBT or IPT should be recommended for virtually all patients with BN S Medications should be used as an adjunct, but there are no clearly efficacious agents for AN S SSRI’s, higher doses, can be effective for BN Conclusions S Treatment of co-morbid conditions and medical complications is essential S Early recognition and timely intervention, based on a developmentally appropriate, evidence based bio-psychosocial multidisciplinary approach, should be the standard of care in every community