Neurological Pathophysiology Chap 20
advertisement

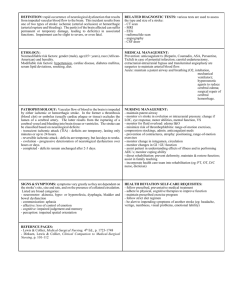
Neurological Pathophysiology 1 Edema in the CNS Increase in tissue mass that results from the excess movement of body fluid from the vascular compartment or its abnormal retention in the tissue. Why is this a special problem in the brain and spinal cord? Enclosed space Lack of lymphatics Lack of anastomoses in venous drainage 2 Vasogenic edema Occurs when the blood-brain barrier is upset – Inflammation due to infection – Toxic agents that damage capillary endothelium – Abnormal capillaries associated with malignant neoplasm Leakage of proteins fluid into interstitium → swelling Plasma filtrate accumulation alters ionic balance and impairs function 3 Cytotoxic edema Intracellular phenomenon Hypoxia – Cardiac arrest – Near drowning – Strangulation – Focal edema due to blockage of an end artery Toxic substances that: – Impair sodium/potassium pump – Impair production of ATP 4 In practice, swelling often caused by both Treatment is different If swelling is due to cytotoxicity, can give I.V. bolus of a hypertonic solution such as mannitol to draw water into the vasculature and out of the brain If the cause is vasogenic would this help? No! would draw fluid into interstitial space and increase swelling!! 5 Increased intracranial pressure (IICP) Normal intracranial pressure is 5-15 mm Hg May be due to: – Tumor growth – Edema – Excess cerebrospinal fluid – Hemorrhage 6 Contents of cranium Tissue of the Central Nervous System Cerebrospinal Fluid (CSF) Blood An increase in any one of these increases intracranial pressure. Clinical hallmarks of IICP: – Headache – Vomiting – Papilledema – swelling of the optic discs 7 Since the brain is encased in the cranium, the only way pressure can be relieved is by decreasing cranial contents. • Most readily displaced is CSF • If ICP still high, cerebral blood volume is altered: •Stage 1 – vasoconstriction and external compression of the venous system •Compensating, so few symptoms 8 If ICP continues to increase, may exceed brain’s ability to adjust. • Stage 2: •IICP (gradually rising) causes a decrease of oxygenation of neural tissue •Systemic vasoconstriction occurs to increase blood pressure to get blood to brain •Clinical manifestations transient: episodes of confusion, restlessness, drowsiness, and slight pupillary and breathing changes 9 When ICP begins to = arterial pressure, there is a lack of compensation- beginning decompensation Stage 3 •Hypoxia and hypercapnia → cytotoxic edema •Decreasing levels of arousal •Widened pulse pressure •May begin Cheynes-Stokes respirations •Bradycardia – due to increased pressure in carotid arteries •Pupils small and sluggish •Surgical or medical intervention needed 10 When all compensatory mechanisms have been exhausted: •Stage 4: •Dramatic rise in ICP in a short time •Autoregulation is lost, and get vasodilation, further increasing intracranial volume •↓ cerebral perfusion = severe hypoxia and acidosis •Brain contents shift (herniate) from area of high pressure to areas of lower pressure ↓ blood flow 11 •Small hemorrhages develop •Ipsilateral pupil dilation and fixation, progressing to bilateral fixed and dilated pupils •When mean systolic arterial pressure equal ICP, cerebral blood flow ceases 12 Treatment Remove the cause of the IICP Mechanical hyperventilation to medicated and comatose patient Reduce blood pressure through diuretics, which slows production of CSF and decreases bloodbrain volume Drugs, us. Barbiturates to slow brain metabolism and ↓ effects of hypoxia Emergency craniotomy to relieve pressure 13 14 Brain Trauma Highest risk: – 15 to 30 years of age – Infants 6 mo. to two years – Young school age children – Elderly persons Male: female = 3:1 15 Most likely causes of head injury: • Transportation accidents • Falls • Sports related events • Violence 16 Two major categories of head trauma: closed (blunt) trauma open (penetrating) trauma 17 Open (penetrating) trauma Break in dura results in exposure of brain tissues to environment. Results in focal (localized) injury May be due to skull fracture or wound – intracerebral hematoma Traumatic pneumocephalus - injury to a nasal sinus that allows air into brain or ventricles - cerebrospinal rhinorrhea 18 19 Blunt Head Trauma More common than open trauma. Involves head hitting hard surface or rapidly moving object strikes head Dura is intact – no brain tissue exposed May cause focal or diffuse axonal injury (DAI) 20 Serious injury decrease due to : Seat belt use Improved management 21 Mild cerebral concussion 75- 90 % of all head injuries Not severe Diffuse axonal injury – no visible signs on brain May see transient dizziness, paralysis, unconsciousness, unequal pupils and shock. Reactive period: vomiting, Temp 99 -100o, rapid pulse, headache, and cerebral irritation lasting 12 -24 hours. 22 Contusions (bruise) : impacts which lead to hemorrhage and possibly hematoma Coup (strike) – head strikes against object shearing forces cause small tears in blood vessels (subdural vessels) edema severity = force smaller area = greater force 23 Contrecoup (rebound) – brain hits opposite side of skull shearing forces and damage opposite to site of impact 24 25 Extradural (Epidural) Hematomas 1-2% of major head injuries Most common in 20-40 year olds Often caused by temporal skull fracture or injury Artery is often the source of bleeding Get herniation (shift) of temporal lobe of brain through tentorial notch 26 27 Subdural hematomas 10 - 20 % of persons with traumatic brain injury Develop rapidly (within hours) Typically on top of skull Often due to tearing of veins or dural sinuses Acts as an expanding mass → IICP→ herniation of brain 28 Intracerebral hematomas 2-3% of head injuries Single or multiple Usually frontal and temporal lobes May occur in deep white matter Small blood vessels injured by shearing forces Acts as expanding mass, compresses tissue, and causes edema May appear 3- 10 days after head injury 29 Clinical manifestations of contusions Loss of consciousness, loss of reflexes Transient cessation of breathing Brief bradycardia Decreased blood pressure As hematoma enlarges: headache, vomiting, drowsiness, confusion, seizure, hemiparesis 30 Treatment Contusions: – Control intracranial pressure Drugs can relieve fluid pressures; may alter Na+ conc. in brain fluids – Manage symptoms hematomas: – Surgical ligation 31 Cerebrovascular Disease Most frequent of all neurological problems Due to blood vessel pathology: – Lesions on walls of vessels leading to brain – Occlusions of vessel lumen by thrombus or embolus – Vessel rupture – Alterations of blood quality 32 CV disease leads to two types of brain abnormalities : Ischemia (with or without infarct) Hemorrhage 33 Cerebrovascular Accident (Stroke) Clinical expression of cerebrovascular disease: a sudden, nonconvulsive focal neurological deficit Incidence: third leading cause of death in U.S. – half a million people a year – one third will die from it 34 Incidence Highest risk > 65 years of age But about 1/3 (28%) are < 65 years old Tends to run in families More often seen in females More often seen in Blacks, perhaps due to increased incidence of hypertension 35 Three types : Global hypoperfusion – shock Ischemia – thrombotic and embolic Hemorrhagic 36 Risk Factors Arterial hypertension Heart disease – Myocardial infarction or endocarditis – Atrial fibrillation Elevated plasma cholesterol Diabetes mellitus Oral contraceptives Smoking Polycythemia and thrombocythemia 37 Occlusive strokes Occurs with blockage of blood vessel by a thrombus or embolus May be temporary or permanent Thrombotic stroke: – 3 clinical types: TIAs Stroke-in-evolution Completed stroke 38 Transient Ischemic Attacks Last for only a few minutes, always less than 24 hours All neurological deficits resolve Symptom of developing thrombosis 39 Causes: Thrombus formation – Atherosclerosis – Arteritis – Hypertension Vasospasm Other: – Hypotension – Anemia – Polycythemia 40 Symptoms depend on location Ophthalmic branch of internal carotid artery – amaurosis fugax – fleeting blindness Anterior or middle cerebral arteries – contralateral monoparesis, hemiparesis, localized, tingling numbness in one arm, loss of right or left visual field or aphasia 41 Treatment Without Tx 80% have a recurrence in symptoms, and 1/3 go on to have a full stroke within 5 years Give anticoagulants prophylactically , usually ½ to 1 aspirin / day 42 Stroke-in-evolution Can have abrupt onset, but develop in a step-by-step fashion over minutes to hours, occasionally, from days to weeks Characteristic of thrombotic stroke or slow hemorrhage 43 Thrombotic CVA Involves permanent damage to brain due to ischemia, hypoxia and necrosis of neurons Most common form of CVA Causes: – Atherosclerosis assoc. with hypertension – Diabetes mellitus, and vascular disease – Trauma 44 May take years to develop, often asymptomatic until major narrowing of arterial lumen Anything that lowers systemic B.P. will exacerbate symptoms (60 % during sleep) Area affected depends on artery and presence of anastomoses Area affected initially is greater than damage due to edema Infarcted tissue undergoes liquifaction necrosis 45 Embolic stroke Second most common CVA Fragments that break from a thrombus outside the brain, or occasionally air, fat, clumps of bacteria, or tumors 46 Common causes Atrial fibrillation Myocardial infarction Endocarditis Rheumatic heart disease and other defects 47 Impact is the same for thrombotic stroke Rapid onset of symptoms Often have a second stroke 48 Hemorrhagic Stroke Third most common, but most lethal Bleeding into cerebrum or subarachnoid space 49 Causes: Ruptured aneurysms Vascular malformations Hypertension Bleeding into tumors Bleeding disorders Head trauma 50 Often a history of physical or emotional exertion immediately prior to event Causes infarction by interrupting blood flow to region downstream from hemorrhage Further damage by hematoma or IICP Onset less rapid than embolic CVA, evolving over an hour or two 51 Usually chronic hypertension, and B.P. may continue to rise About half report severe headache In about 70 % hematoma expands, destroying vital brain centers, shifts of brain tissue, and death 52 Degenerative Disorders Progressive neurodisorders Long-lasting Permanent effects Many present as syndromes No cure, but much research 53 Alzheimer Disease (Dementia of Alzheimer Type) 54 Dementia is a loss of ordered neural function Discrimination and attending to stimuli Storing new memories and retrieving old Planning and delay of gratification Abstraction and problem solving Judgement and reasoning Orientation in time and space Language processing Appropriate use of objects Planning and execution of voluntary movements 55 Course : slow progression (5years or more) At first affects only short term memory, but gradually extends to long term Many experience restlessness Many patients retain insight, which leads to anxiety and depression Personality may be lost Ultimately, mute and paralyzed Death comes from infection 56 Onset may be as young as 50, and incidence increases with age: – 6 % of people over 65 years have AD – Almost half over 85 have AD Diagnosis is by ruling out all other causes –specific diagnosis only by biopsy or autopsy 57 Pathology restricted to cerebral cortex, hippocampus, amygdala, and another basal nucleus called nucleus of Meynert Nucleus of Meynert produces Acetylcholine – loss results in impaired neural function 58 Pathology Pyramidal cells die; loss of white matter Gyri shrink and and ventricles and sulci expand – walnut like appearance Neurofibrillary tangles Neuritic (senile) plaques : filaments, microglia, astrocytes around core of amyloid Amyloid angiopathy 59 http://www.ahaf.org/alzdis/about/plaques_tanglesBorder.jpg 60 61 www.infoaging.org/ d-alz-8-r-tangles.html http://homepage.psy.utexas.edu/homepage/class/Psy332/Salinas/Disorders%20/62 Disorders.html About 10 % of cases are familial, usually early onset Gene on chromosome 21 – carries gene for amyloid protein Almost all people with Down syndrome who live beyond 45 years develop AD Also linked to mutations on chromosomes 14 and 19 Prions have been isolated 63 Treatment So far resistant May revolve around amyloid protein See high levels of aluminum – chelating agents temporarily arrest or reverse some symptoms THA(tetrahydroaminoacridine) used experimentally – liver toxicity Arthritics have lower incidence of AD Therapy centers on problems of failing cognitive skills 64 Parkinson Disease – movement disorder Described over 180 years ago by James Parkinson Combination of slowed, reduced movements and restless tremoring Paralysis agitans Slowly degenerative CNS disorder affecting 80,000 adults in North America 65 Parkinson Disease Degenerative disease of the basal ganglia involving the failure of dopamine-secreting neurons (substantia nigra) Can be primary or secondary Secondary caused by trauma, infection, neoplasm, atherosclerosis, toxins and drug intoxication 66 67 Primary Parkinson Disease Begins after the age of 40, with peak age of onset between 58 – 62 Course of 10- 20 years – slowly progressive More prevalent in males (slightly to 2X) 68 Substantia nigra – two nuclei in midbrain Outflow pathway from basal nuclei to cortex via thalamus Damage impairs flow of motor programs Expressed as difficulty initiating movements, general lack and slowing of movement (bradykinesia) 69 Loss of feedback loop impairs flow of programs and expresses as resting tremor Most disabling symptoms are muscle rigidity and bradykinesia Muscle strength is more or less normal Poor balance Face becomes immobile and inexpressive Autonomic function is decreased: – orthostatic hypotension, excess sweating, constipation, etc. 70 Some patients suffer dementia similar to Alzheimer Disease Not fatal, but shortens life expectancy 71 Treatment Active exercise and good nutrition Strategies to overcome bradykinesia Only when symptoms are severe are drugs given – levodopa Side effects: cardiac arrhythmias, gastrointestinal hemorrhage, psychiatric problems, unpredictable involuntary movement disorders 72 Possible therapies Foreign or autograft of tissue still experimental Lesions in the subthalamic nucleus, thalamus or internal segment of globus pallidus promising Stem cell research? 73 Multiple Sclerosis Focal, chronic, progressive, usually exacerbating and remitting demyelination of CNS tracts. Lesions can occur in a wide variety of locations and give rise to complex symptoms Areas of demyelination are called plaques, and can occur anywhere oligodendrocytes provide myelin sheath 74 Onset Onset is between 20 and 40 years, rarely before 15 or after 50 Females: Males 2:1 75 Clinical presentation depends on site of lesion Involvement of optic nerve produces monocular visual disturbances – first symptom in ¼ of patients Half of people with optic neuritis are diagnosed with MS 76 Common symptoms: Double vision Tingling in the back and anterior thigh upon neck flexion – Lhermitte’s sign Symptoms worsen when patient becomes heated – Uhthoff’s sign 77 Diagnosis CSF obtained by lumbar puncture shows slight increase in protein; on electrophoresis shows specific banding pattern – antibodies within CSF suggest immune reaction Changes in velocities of visual and auditory pathways Plaques visible on MRI 78 Cause Myelin undergoes breakdown and phagocytic destruction – antibodies may play a role Decreased signal conduction due to edema and demyelination that exposes potassium channels that short-circuit signal (edema resolves and have partial remyelination) 79 Epidemiology hints at interaction between a viral illness in the teen years and a genetic predisposition Growing up in northern temperate climates increases rise Non Asian heritage increases risk 80 Course Pattern of exacerbation and remission Stresses can trigger exacerbation: infection, medication, stress, fatigue Course is unstable and unpredictable 10 % undergo severe, rapid progressive deterioration Some have died with 7 months of first symptom due to acute brain inflammation and infection 81 A significant number never severely incapacitated Some experience only a single episode Death is usually attributable to complications of MS (infections due to decreased function) 82 Symptoms Increased urinary frequency Lesions in frontal or temporal lobes can cause emotional outbursts Depression and euphoria can be problems Unpredictable progression taxes ability to cope Occasionally, plaques can cause paraplegia or quadriplegia 83 Therapies Only corticosteroids and ACTH appear to have effects – reduce the duration of exacrerbation, but have no impact on long term outcome Interferon β Maintaining a healthy lifestyle and outlook 84 Acute encephalopathies: Reye’s Syndrome First recognized in 1963 Characterized by encephalopathy and fatty changes in several organs, esp. liver Incidence has declined in past 20 years due to awareness of ingestion of aspirin during illness and development of Reye’s syndrome. 85 Reye’s syndrome Typically develops in a healthy child of 6 mo. to 15 years recovering from varicella, influenza B, upper respiratory tract infection, or gastroenteritis. Stage I: vomiting, lethargy, drowsiness Stage II: disorientation, delirium, aggressiveness and combativeness, central neurological hyperventilation, shallow breathing, hyperactive reflexes, stupor 86 Reye’s syndrome Stage III: Insensitivity to pain, coma, hyperventilation, rigidity Stage IV: deepening coma, loss of ocular reflexes; large, fixed pupils; divergent eye movements Stage V: seizures, loss of deep tendon reflex, flaccidity, respiratory arrest Mortality is 10 or more Formerly 40 to as high as 80% In a few cases death is due to liver failure 87 Reye’s syndrome Cause: – May have a genetic predisposition – May be due in part to exhaustion of glycogen stores and use of fatty acids -Mitochondrial injury Treatment: – Aggressive intensive care – Treatment for brain edema and IICP – Fluids I.V. and control of blood electrolytes – Prevent hyperthermia 88 Seizure disorders Seizure is and abnormal discharge of electrical activity within the brain. It is a rapidly evolving disturbance of brain function that may produce impaired consciousness, abnormalities of sensation or mental function or convulsive movements. Convulsions are episodes of widespread and intense motor activity 89 Epilepsy A recurrent disorder of cerebral function marked by sudden, brief attacks of altered consciousness, motor activity or sensory phenomenon. Convulsive seizures are the most common form Some, but not all, recurrent seizures are due to epilepsy 90 Epilepsy Second most common neurological disorder Incidence increases with age, with 30% initially occurring before 4 years and 75 -80 % before 20 years. Causes: brain tumor, scar tissue, neurological disease, great majority of cases are idiopathic. 91 Signs and symptoms vary: petit mal – almost imperceptible alterations in consciousness grand mal – generalized tonic-clonic seizures – dramatic loss of consciousness, falling, generalized tonic-clonic convulsions of all extremities, incontinence, and amnesia for the event. 92 Some attacks are proceeded by a prodrome – a set of symptoms that warn of a seizure As the seizure begins, the patient may experience an aura – mental, sensory or motor phenomena Others have no warning 93 Phases of a grand mal seizure 1. Tonic phase ( 10 -20 seconds) – muscle contraction Epileptic cry – respiration stops 2. 3. Clonic phase – (1/2 -2 minutes) muscle spasms; respiration is ineffective; autonomic nervous system active Terminal phase (about 5 minutes) –limp and quiet, EEG flat lines 94 5-8 % are at risk of status epilepticus – a series of GTCS without regaining consciousness – medical emergency Seizure activity lasts more than 30 minutes – Acidosis – Elevated pCO2 – Hypoglycemia – Fall in blood pressure Can lead to severe brain damage or death 95 Epileptogenic focus Group of brain neurons susceptible to activation Plasma membranes may be more permeable to ion movement Firing of these neurons may be greater in frequency and amplitude Electrical activity can spread to other hemisphere and then to the spinal cord 96 Treatment Treat any underlying metabolic disorders, or tumors Most cases can be controlled through routine use of antiepileptic medications – usually only one drug to minimize side effects Surgical intervention if drugs ineffective Supportive therapy – patients learn to cope effectively with stress, eat well, and get sufficient rest and avoid triggers. 97 Eliciting stimuli: Hypoglycemia Fatigue Emotional or physical stress Fever Hyperventilation Environmental stimuli 98 Patients are normal between attacks Can participate in sports, drive a car (if no seizures for 6 mo – 1 year) Should not drink alcohol 99