Neurological Emergencies
advertisement

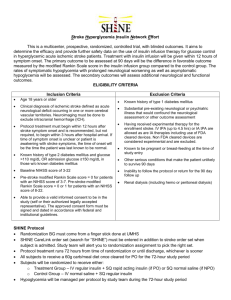
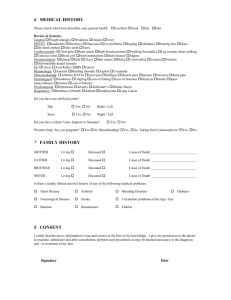
NEUROLOGICAL EMERGENCIES Amy Gutman MD prehospitalmd@gmail.com OVERVIEW In the next 2 hours: Anatomy & Physiology Focused Assessment & Examination Differential Diagnosis Management & Critical Thinking What we will not cover in the next 2 hours: Trauma patients with neurological findings Psychiatric emergencies TERMINOLOGY Neurology (Greek): “ Vεῦρον” (neuron), “λογία” (study); medical specialty studying diagnosis & treatment of nervous system disorders Neuron: Single nerve cell Neurotransmitter: Chemicals allowing impulses to travel between neurons Ipsi / Unilateral: Same-sided, one sided Contralateral: Opposite-sided Paralysis: Complete loss of function Paresis: Limited function Anesthesia: Complete loss of sensation Paresthesias: Abnormal sensation Lesion: Focus for neurological abnormality ANATOMY & PHYSIOLOGY - CNS Neurons & Neurotransmitters Protective Structures Brain Spinal Cord NEURONS & NEUROTRANSMITTERS Billions of neurons allow body functions via neurotransmitters Neurotransmitters are excitatory or inhibitory Excitatory: acetylcholine, norepinephrine Inhibitory: dopamine, serotonin, GABA Each neurotransmitter directly or indirectly influences specific type(s) of neuron NEURONS & NEUROTRANSMITTERS Nerve impulse travels from n euron through axon to terminal & synaptic knob Synaptic knob communicates with dendrite of neighbor neuron via neurovesicles that store & release neurotransmitters into synapse If stimulated in a “lock & key” manner, the next neuron picks up & continues the impulse Seizures: continuous release / stimulation of impulses = spasm Botulism: neurotransmitters bound so no impulses = flaccidity CNS PHARMACOLOGY Depressants Increase GABA (inhibitory neurotransmitter), decreasing nervous system activity Barbiturates, Benzodiazepines If combined other depressants can be fatal Abrupt discontinuation leads to withdrawal & seizures Stimulants Increase norepinephrine, dopamine to increase nervous system & catecholamine response Dexromethorphan, methylphenidate, cocaine CNS PROTECTIVE STRUCTURE - SKULL CNS PROTECTIVE STRUCTURES – VERTEBRAE (SPINE) CNS PROTECTIVE STRUCTURES MENINGES CNS - BRAIN Frontal Lobe Thinking, planning Executive functions Motor execution Parietal Lobe Somatosensory perception Integration of visual & somatospatial information Temporal Lobe Language function Auditory perception Memory Emotion Occipital Lobe Visual perception & processing CNS - BRAIN CNS – VASCULAR SUPPLY CNS – SPINAL NERVES & DERMATOMES CERVICAL DERMATOMES “C 3 4 5 keeps the diaphragm alive” ROOT C3 C4 C5 C6 C7 C8 T1 MOTOR Diaphragm, Trap Diaphragm Bicep & deltoid Bicep Tricep Finger flexors Hand intrinsics SENSORY Lower neck Clavicle Below clavicle Thumb, forearm Index, middle fingers Pinky Medial Arm CRANIAL NERVES 1 2 3 4 5 6 7 8 9 10 11 12 Olfactory Optic Oculomotor Trochlear Trigeminal Abducens Facial Vestibulocochlear Glossopharyngeal Vagus Spinal Accessory Hypoglossal "On Old Olympus's Towering Tops, A FineVested German Viewed Some Hops" "Oh, Oh, Oh, To Touch And Feel, A Good Velvet, Spot in Heaven" Motor (M), sensory (S), or both (B) "Some Say Money Matters But My Brother Says Big Brains Matter Most" ANATOMY & PHYSIOLOGY - PNS Autonomic Nervous System Sympathetic: “Fight or Flight” Parasympathetic: “Feed or breed”, “Rest & Repair” Clinically: “Point & Shoot” Peripheral Nerves 43 pairs of nerves originate from CNS to form PNS 12 pairs of cranial nerves from brain 31 pairs of spinal nerves from spinal cord ANATOMY & PHYSIOLOGY - PNS PREHOSPITAL ASSESSMENT THE BIG PICTURE Altered Mental Status Focal Neurological Complaints “Sick” vs “Not Sick” CHIEF COMPLAINT Exact quotes – words are clues “The room is spinning” vs “I feel like I’m spinning” “My vision is blurred” vs “I have double vision” Obtain from pt, witnesses, family while beginning assessment & management CC, HPI & exam should focus on neurological aspects, without overlooking non-neurological processes causing AMS or deficits HISTORY OF PRESENT ILLNESS Allergies Medications PMH Sz, trauma, HA, HTN, DM, infections, tumors Cardiac, renal, hepatic, neuro, psychiatric diseases Last oral intake Events leading up to event Environmental clues Indoors or outdoors? Any unusual odors? Suicide notes? Provokes / Progression / Palliation Quality Region/radiation Severity Time of onset Family/Social history NEUROLOGICAL EXAM - ASSESSMENT Level of consciousness Memory & amnesia AVPU / GCS Focal neurological exam Af fect/mood Speech Behavior & posture Cognition Mood, Thought, Perception, Judgment, Memory & Attention Grooming & personal hygiene GLASGOW COMA SCALE (3-15) Eye 4 3 2 1 Opening = Spontaneous = To Voice = To Pain = None Verbal 5 = Oriented 4 = 3 = 2 = 1= Confused Inappropriate words Inappropriate sounds None Motor 6 = Obeys commands 5 = Localizes pain 4 = Withdraws to pain 3 = Decorticate 2 = Decerebrate 1 = None The number is less important than the category & what you do with it! NEUROLOGICAL EXAM - SPEECH Speech and language “Hear them talk, watch them talk, & look at their eyes; that’s 90% of the brain” (Henry, 2004) Normal speech inflected, clear, fluent, articulate, varies in volume Language Dysphonia: Inability to make laryngeal sounds Dysprosody: Inflection, pronunciation, pitch or rhythm (cerebellum) Dysarthria: Difficulty making individual sounds (motor integration) Aphasia: absence of speech Dysphasia: word finding difficulty (cortex) Expressive aphasia: understands but cannot speak (frontal Broca’s) Receptive aphasia: words clear, content scrambled (parietal Wernicke’s) Apraxia: difficulty in both forming & phonating VITAL SIGNS BP: Hypotension Hypertension Cushing’s Triad: Hypertension Bradycardia Bradypnea Respirations Hyperventilation Hypoventilation Cheyne-Stokes: crescendodecrescendo then apnea Ataxic: irregular rate & depth Apneustic: inspiratory pause Temperature: Infection Hemorrhage Seizure (cause or effect) Heat stroke Metabolic PHYSICAL EXAM Head Skull: trauma; infants – bulging membranes Mouth: odors, bites to lateral tongue Neck Meningismus Skin Trauma, rash, IVDA, temperature Lungs, Cardiac, Abdomen Systemic illnesses and secondary effects of CNS insults Extremities Trauma, deformity, pulses NEUROLOGICAL EXAM - EYES Pupil size, symmetry, reactivity Miosis Mydriasis Extraocular movements Resting eye position Deviation Nystagmus / direction Conjugate movement NEUROLOGICAL EXAM – MOTOR & SENSORY Cranial ner ves Reflexes Cerebellar Gait Finger pointing Psychiatric Posturing Any asymmetr y Seizure activity Look at eyes Test glucose & you have the Miami / LA Stroke Scale DIFFERENTIAL DIAGNOSIS / NEUROLOGICAL EMERGENCIES THE BIG PICTURE Altered Mental Status Focal Neurological Complaints “Sick” vs “Not Sick” CAUSES OF AMS AEIOU TIPS A E I O U T I P S Alcohol / Drugs / Toxins Endocrine, Exocrine, Electrolyte Insulin Opiates, OD Uremia Trauma, Temperature Infection Psychiatric disorder Seizure , Stroke, Shock, Space occupying lesion AMS PEARLS History often initially more important than exam What is MOST important question with a neuro deficit or AMS? Physical Exam Keys Odors Respiration Eyes Trauma? IVDA? Serial GCS If <8, INTUBATE! ALCOHOL / DRUGS / TOXINS Drunk + ground = head & C spine injur y until proven otherwise Multiple toxidromes & drug reactions cause AMS or focal deficits Common: Organophosphates CO Sympathomimetics / withdrawal Opiates / Withdrawal Hypoglycemic agents Cardiac agents Psych Meds (TCAs, SSRIs) Another day, another lecture! TEMPERATURE Hypothermia: AMS / coma <32.0 C Hyperthermia: AMS / coma >42.0C Environmental Sepsis Drug reaction Neuroleptic malignant syndrome EXOCRINE / ENDOCRINE / ELECTROLY TE Most Common Hypo / hyperglycemia Hypo / hyperkalemia Hyponatremia Thyroid storm Cause vs effect AMS Seizures Syncope Often related to arrhythmias STROKE –EPIDEMIOLOGY Disability af fects 75% sur vivor s #1 cause adult disability in the US & Europe #3 cause death worldwide after CAD & cancer 10% deaths worldwide US Management costs $43 billion annually Incidence increases exponentially >30 yr s Etiology varies by age 95% of strokes occur in people >45 yo 75% of strokes occur in people >65 yo Rule of two thirds 2/3 all strokes ischemic 2/3 of those thrombotic STROKE - GENDER DIFFERENCES Men 1 .25 x more likely to suf fer strokes than women However, 60% of deaths from stroke occur in women Since women live longer than men, they are older on average when they have their strokes & therefore more of ten killed Some risk factors for stroke apply only to women: Pregnancy Childbirth Menopause HRT STROKE - RISK FACTORS Advanced age Previous stroke or TIA Diabetes High cholesterol Cigarette smoking Atrial fibrillation HRT Migraines Thrombophilia Patent foramen ovale HTN Most important & modifiable STROKE - MIMICS Seizure Infection Hypoglycemia Syncope Brain abscess or tumor Drug Overdose Head Trauma Vascular Lesions HTN Encephalopathy Migraine STROKE PATHOPHYSIOLOGY - ISCHEMIC Thrombotic Slow, progressive onset Causes: Atherosclerosis (#1 cause) Infective Inflammatory (vasculitis) Hypercoaguable states Embolic Abrupt onset Maximal deficit may improve over time as embolus breaks Causes Mural thrombus (#1 ) Aortic plaques Endocarditis Long bone injuries Dysbarism STROKE SYNDROMES - TIA / RIND Altered neuro status that resolves completely <24hrs (TIA) or <72hrs (RIND) 30% will have a major stroke event within 3 years Treat as CVA STROKE PATHOPHYSIOLOGY – HEMORRHAGIC Spontaneous rupture leads to subarachnoid hemorrhage HTN Congenital abnormality (AV malformation, berry aneurysm) Blood dyscrasia / anticoagulants Infection Neoplasm Classic Presentation: 35-65 yo M with h/o HTN with undiagnosed berr y aneur ysm Abrupt onset of “worst headache of life” Nuchal rigidity, photophobia, vomiting, retinal hemorrhages Atypical: hemorrhagic transformation of embolic stroke STROKE PATHOPHYSIOLOGY SYSTEMIC HYPOPERFUSION Reduction of blood flow to all parts of the body Causes: Pump failure: cardiac arrest, arrhythmias Reduced cardiac output: MI, PE, hemorrhage, shock Hypoxemia Entire brain affected, especially penumbra / "watershed" STROKE SYNDROMES – CEREBRAL BLOOD FLOW Anterior Circulation: 80% cerebral blood flow Originates from carotids Supplies fronto-parietal, anterior temporal, optic nerve Posterior Circulation: 20% cerebral blood flow Originates from vertebrobasilar arteries Supplies thalamus, brainstem, occipital cortex, cerebellum, upper cord, ears Circle of Willis: Connects ant & post circulations STROKE - SYMPTOMS Generally Unilateral Stroke site on opposite side than clinical ssx LOC, HA, & vomiting more common in hemorrhagic than ischemic (higher ICP) Cerebral Cortex: Occipital: Temporal: Parietal: Frontal: Visual field defect Memory deficits Hemineglect , aphasia Disorganized thinking, confusion, hypersexuality SYMPTOMS Brainstem / Cranial Nerves: Altered smell, taste, hearing, or vision Ptosis, diplopia, pupil reactivity Decreased gag, tongue movement, facial sensation & muscle weakness Balance problems & nystagmus Altered breathing & pulse Cerebellum Altered coordination Vertigo or disequilibrium TIME IS BRAIN From the time a patient first experiences ssx there is a 3* hr window to administer tPA That window includes: Recognition of symptoms Call to 911 & activation of EMS EMS response, assessment, management & transport ED assessment & CT scan to rule out hemorrhagic stroke Stroke team activation & screening for TPA 11% increase in measureable (+) symptom improvement TPA only given to 1-2% of stroke patients *Debatable & Changing STROKE MANAGEMENT – THROMBOLYTIC CHECKLIST Answer to ALL must be YES: Answer to ALL MUST be NO: >18yo Acute ischemic stroke causing a measurable nonimproving neurologic deficit NO clinical suspicion for SAH Time of onset to treatment is <180 mins CT proven hemorrhage Active internal bleeding <21 days B leeding diasthesis: Plts<100,000 Heparin <48 hrs w/high PTT Warfarin use with high PT P rior surger y or ischemic CVA <3 mos M ajor surger y <14 days AMI, arterial stick/LP <7 days P rior ICH, AVM, tumor, aneur ysm or seizure + stroke SBP >185mmHg or DBP >110Hg No septic emboli STROKE - MANAGEMENT ABCs + Glucose Protect penumbra Keep SBP >90mmHg Keep CPP >60mmHg Hypothermia Oxygenate HOB 30 degrees (reverse T-berg if C spine in question) Frequent repeat neuro checks!! Reassess GCS! *CPP = MAP - ICP SEIZURES - EPIDEMIOLOGY 1 – 2% general population Primary / Idiopathic Onset ages 10-20 Often “outgrow” their medications Secondary precipitated by “something” Intracranial: trauma, mass, abcess, infarction Trauma, mass, abscess, infarct Extracranial: toxins, metabolic, HTN, eclampsia SEIZURE – CLASSIFICATION Grand Mal: Aura, tonic-clonic, LOC, apnea, incontinence, post-ictal Petit Mal Absence Myoclonic Simple Partial Seizures Involve one body area Can progress to generalized seizure Complex Partial Seizures Characterized by auras Typically 1–2 minutes in length Loss of contact with surroundings ECLAMPSIA Any pregnant patient who seizes, regardless of prior history Of ten secondary to undertreated / undiagnosed pre -eclampsia Medical emergency for both mother & child Management: IV, O2, Monitor Left lateral recumbent position Rapid Transport Magnesium sulfate MAGNESIUM SULFATE Pregnancy -induced HTN, pre-eclampsia, eclampsia Decreases CNS activity & release of ACH Vasodilator (decreases systemic BP, improves placental blood flow) Side Ef fects Muscle weakness Respiratory depression Hypotension & slowed cardiac conduction/AV blocks Antidote Calcium gluconate SEIZURE - MANAGEMENT ABCs + C spine + Glucose + Pregnancy IV, O2, Monitor HPI Timeframe? Prior history? Pregnancy? DM? Trauma? Infection? Serial neuro exams SEIZURE - STATUS EPILEPTICUS Seizure >5 mins OR 2 seizures between which there is incomplete recovery of consciousness Management: ABCs IV, O2, Monitor Benzodiazepines Treat other causes: Glucose Magnesium Pyridoxine (B6) SYNCOPE Acute & temporary loss of consciousness Pre-syncope: No LOC Pt often states “I thought I was going to pass out” Syncope is a symptom, not a diagnosis DDX: Cardiovascular: a rrhythmias, valve stenosis, hypotension Noncardiovascular: m etabolic, neurological, psychiatric Idiopathic Pearls: Extended unconsciousness is NOT syncope All drunks have head & C spine injuries if unconscious + fall SYNCOPE MANAGEMENT ABCs & support ventilations Maintain airway IV, O2, Monitor, Glucose Look for other causative / contributive factors Heat stroke MI CVA CHI Dehydration SEIZURE VS SYNCOPE INFECTIOUS - MENINGITIS US Incidence 1.5 per 100,000 Rare in young pts (Hflu & pneumovax vaccines)* CDC: median age 39 years; in 1986, it was 15 months Mortality/Morbidity Depends on pathogen, age, general physical state & severity of acute illness Pneumococcal mortality 21%, morbidity 15% Mortality 90% if severe neurologic impairment at time of presentation even with immediate medical treatment *PLEASE immunize your kids! INFECTIOUS - MENINGITIS Bacterial Rapid onset of symptoms Fever, HA, photophobia, meningismus, AMS Etiology varies by age / exposure / PMH Neisseria meningitis associated with diffuse, purpuric rash Aseptic/ Viral/ Lymphocytic Gradual onset over 1-7 days Less virulent Atypical PMH / HPI critical as onset insidious TB(#1) Fungal: coccidiomycosis / crytococcus INFECTIOUS - ENCEPHALITIS Brain inflammation Cases self-limited unless virulent strain/immunocompromised Presents similarly to meningitis Viral / tick-borne etiology most common West Nile Herpes Simplex (HSV) Varicella Zoster (VZV) Arboviruses Eastern Equine viruses St. Louis Encephalitis INFECTIOUS – CORNYBACTERIUM DIPTHERIA Acutely ill patient + fever in a dPT deficient patient Bleeding membranous pharyngitis Exotoxin causes multi-organ system failure Myocarditis/AV Block Nephritis Hepatitis Neuritis with bulbar / peripheral paralysis Ptosis, strabismus, loss of DTRs Management ABCs, intubation, volume resuscitation IN ED: PCN, emycin, horse serum antitoxin, pressors INFECTIOUS – CLOSTRIDIUM BOTULINUM Triad: diplopia, ophthalmoplegia, ptosis Descending neurologial deficits causing respiratory paralysis Normal mentation / sensation Infant FTT / “floppy baby” Raw honey contains C. botulinum Management: ABCs, intubation In ED: trivalent serum antitoxin INFECTIOUS – CLOSTRIDIUM TETANI Trismus, Tetany, Twitching, Tightness Risus sardonicus Sympathetic overstimulation Tachycardia, hyperpyrexia, diaphoresis Management: ABCs, intubation In ED: Human Tetanus Immunoglobulin (HTIG), dT toxoid, metronidazole INFECTIOUS – GUILLAIN-BARRE SYNDROME Most common acute polyneuropathy 2/3s have preceding URI or gastroenteritis Generalized paresthesias then ascending paralysis Miller-Fischer variant: ataxia, areflexia, and ophthalmoplegia 1976 swine flu tainted vaccine caused 25 deaths from GBS & the foundation for current anti-vaccine sentiment Management: ABCs, intubation INFLAMMATORY BELL’S PALSY Facial nerve paralysis af fecting entire unilateral face In supranuclear lesions like a cortical stroke (UMN defect), the upper 1/3 of the face spared while lower 2/3 paralyzed Orbicularis, frontalis & corrugator muscles innervated bilaterally, which explains facial paralysis pattern Eye closure on af fected side impaired Bell Phenomenon: on attempting to close eye, the eye on the affected side rolls upward & inward Ramsay -Hunt: zoster vesicles along ear canal, pinna, mouth HEADACHE Migraine (w/ wo aura)* Cluster Traumatic Inflammatory History: Worst HA? Onset? Fever / AMS? Trauma? Prior history? Management: IV, O2, antiemetics Cool, dark environment Abortive therapy Believe it or not, narcotics actually make headaches worse physiologically *Pet peeve HEADACHE - MIGRAINE Though to be related to neurogenic inflammation & abnormalities of serotonergic transmission* HA either preceded by a visual aura or motor disturbance N/V, photophobia, sound sensitivity Provocation factors: Menstruation Sleep/food deprivation Physical activity Foods Contraceptive estrogens *i.e. neurologists really have no freakin’ clue why they occur HEADACHES - OTHER Cluster: Resemble CVAs Unilateral & persistent Thought to be a form of seizures by some neurologists Temporal Arteritis Temporal artery inflammation (branch of external carotid) Unilateral HA with temporal artery tenderness & decreased vision in middle-aged white females Rapid initiation of steroids will save patients vision Be concerned with any HA plus fever, confusion, nausea, vomiting or rash PERIPHERAL VERTIGO Common Causes: Labrynthitis Cerumen Impaction OM / OE URI Meniere’s Disease: tinnitus, hearing loss, vertigo History: Acute onset of severe dizziness, N/V Positional worsening of symptoms Often recent URI or prior vertiginous episodes Exam: Fatigable horizontal nystagmus URI SSX CENTRAL VERTIGO 10-15% cases of ver tigo Causes: Brainstem ischemia or infarction Cerebellar hemorrhage Vertebralbasilar insufficiency MS Brainstem /cerebellar lesions SSX: Disequilibrium N/V Nonfatigable nystagmus Focal findings: Ptosis Facial palsy Dysarthria Cerebellar findings Ataxia Vertigo Management IV, O2, Monitor Antiemetics Cannot be differentiated from a posterior circulation CVA in the field Always treat as if a CVA “WEAK & DIZZY” Underlying disease with extensive differential diagnosis Often the presenting symptom of CVA, MI, sepsis Pay attention to “weak & dizzy” with: Nystagmus Nausea/vomiting Focal neuro deficits AMS Management: I, O2, Monitor, Glucose, EKG OTHER NEUROLOGICAL DISORDERS Alzheimer’s Dementia Most frequent cause of dementia in the elderly Brain atrophy due to cerebral cortex neuron death Muscular Dystrophy Characterized by progressive ascending muscle weakness Multiple Sclerosis Unpredictable Resulting from deterioration of myelin sheath Dystonias Often related to psychiatric medications OTHER NEUROLOGICAL DISORDERS Parkinson’s Disease Tremor, rigidity, bradykinesia, postural instability Amytrophic Lateral Sclerosis Myoclonus Spina Bifida Poliomyelitis Chronic Alcoholism Wernicke’s Syndrome Korsakoff’s Psychosis GENERAL NEUROLOGICAL EMERGENCIES MANAGEMENT PRINCIPLES ABC + Glucose Ensure patent airway maintaining C-spine Limited airway protection may lead to vomiting / aspiration IV, O2, Monitor Serial examinations Rapid recognition of underlying neurological emergencies “Sick” vs “Not Sick” Pre-notification Time is brain! SUMMARY Anatomy and Physiology Pathophysiology General Assessment Findings Differential Diagnosis Management of Nervous System Emergencies QUESTIONS? P R E H OSP ITALMD@ G MA IL.C OM