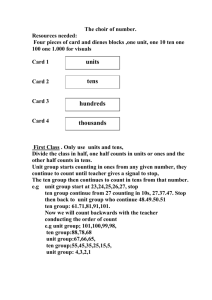
8.0 The Gate Control Theory of Pain
advertisement

5th of January 2010 Industrial Medicine University of Aalborg Foreword This report is composed by group 306 during the course of the P3-project on the 3rd semester on MEDIS at the University of Aalborg. The report was compiled from the 9th of November 2009 to the 5th of January 2010. The main subject was Touch inhibits pain and in this context we decided to concentrate on the Gate Control theory and electrical stimulation with its function as pain relieving. The target group of this project is our fellow students on MEDIS and also our teachers plus others with a scientific interest in the field. The supervision during the project was attended by Jens Ellrich and Dejan Ristic. Our group expresses our thanks to both supervisors. Group 306, the University of Aalborg 1 5th of January 2010 Industrial Medicine University of Aalborg Table of contents Foreword .............................................................................................................................................. 1 Reader’s guidance ................................................................................................................................ 4 1.0 Introduction .................................................................................................................................... 5 2.0 Epidemiology of chronic pain ........................................................................................................ 5 3.0 The neural processing .................................................................................................................... 7 3.1 The Synapse ............................................................................................................................... 7 3.2 Neurotransmitter’s receptors ...................................................................................................... 8 4.0 Somatic sensation and nociception ................................................................................................ 9 4.1 Tactile receptors ......................................................................................................................... 9 4.2 Tactile pathway .......................................................................................................................... 9 4.5 Physiology of nociception and pain ......................................................................................... 10 4.6 Spinal cord ............................................................................................................................... 11 4.7 Neospinothalamic tract ............................................................................................................ 12 4.8 Paleospinothalamic tract .......................................................................................................... 12 4.9 Pain control system .................................................................................................................. 13 5.0 Psychological pain model ............................................................................................................ 14 6.0 Treatment of chronic pain ............................................................................................................ 15 6.1 Opioid analgesics ..................................................................................................................... 15 6.2 Non-opioid analgesics .............................................................................................................. 15 6.3 Non-drug treatments ................................................................................................................ 16 6.4 Statistics of treatment in Europe .............................................................................................. 16 7.0 Thesis statement ........................................................................................................................... 16 8.0 The Gate Control Theory of Pain ................................................................................................. 17 8.1 Reconsideration of the theory .................................................................................................. 19 9.0 Electrical stimulation and the relief of pain ................................................................................. 21 9.1 Principles of TENS .................................................................................................................. 22 9.2 Physical principles ................................................................................................................... 22 9.3 Mechanisms of action .............................................................................................................. 23 9.4 Explanation of TENS by GCT ................................................................................................. 24 9.5 The adverse effects of TENS ................................................................................................... 24 9.6 The clinical use of TENS ......................................................................................................... 24 10.0 Discussion .................................................................................................................................. 25 11.0 Conclusion ................................................................................................................................. 28 12.0 Putting into perspective .............................................................................................................. 29 2 5th of January 2010 Industrial Medicine University of Aalborg 13.0 Explanations of words ................................................................................................................ 30 14.0 List of references ........................................................................................................................ 33 3 5th of January 2010 Industrial Medicine University of Aalborg Reader’s guidance As guidance to the reader, the structure of the report will be outlined. The composition follows the model showed in Figure 1. The first part of the report is an introduction to the problem, where the epidemiology and statistics of chronic pain are outlined. In the second part of the report, called the analysis of the problem, the somatic sensation, physiology of pain and the treatment of pain are outlined. The next part of the report narrows the main problem to a specific issue that is discussed subsequently. This part concentrates on the Gate Control Theory in association to transcutaneous electrical nerve stimulation and its function as pain relieving. Afterwards, the main problems are discussed and later a conclusion is made against a background of Figure 1: Illustrate the structure of the report. See text for more details. the theory and discussion. Finally, the issues are put into perspective. On going through the report you find different phrases consisting of several words. These phrases will, after first appearance, be abbreviated with the letters mentioned in the parentheses immediately after the words. For instance the phrase Gate Control Theory will be abbreviated GCT. The different chapters are numbered after the following principle; 2.0; 2.1; 2.1.1. Figures and tables in the report are numbered in chronological order. The figures and tables with no reference are made by the group itself. Words, that are indicated with an * in the end of the word, are listed in the paragraph called 13.0 Explanation of words. This is a list with explanations of selected words from the report that are found necessary to explain furthermore. The words are arranged alphabetically in the list. The reference system is the Harvard-system and in the list of references is all the necessary information about the concerned source. In the list of references the sources are arranged alphabetically after the main author’s last name. 4 5th of January 2010 Industrial Medicine University of Aalborg 1.0 Introduction Pain is known by everybody as an unpleasant feeling. It is experienced on a daily basis when you bump into a table, get a vaccine, have overstretched a muscle, when you have a headache after too much alcohol etc. These everyday pain experiences can make a person feel uncomfortable, but is normally considered as something harmless. Pain can also be more severe and this kind of pain is nearly known by everyone. This can be when a woman is in labor, it could be people who are seriously hurt in a car crash or when we see a football player on TV who gets a bad injury in a match. In other words; pain can be felt to different extents, be caused by different reasons and is experienced in different ways. The reaction to pain is also different from one person to another. Some yells, some cries and some cannot say a word. One reaction that is often seen, both in many different kinds of pain and in different types of people, is the same; the fact that we touch the area where the pain originates – but why do we react by touching an area that already hurts? This reaction is widely seen among everybody, which indicates that the explanation could be a general matter of the physiology of pain. Furthermore, many would say that the reaction helps them to inhibit the pain. So why do touch inhibits pain? A theory, that could explain this phenomenon, is the Gate Control Theory of pain, which clarifies some possible reasons. This pain theory has also led to different methods of pain treatment, which could help solve the problems of chronic pain. Before it is possible to look at this subject, some basic theory and statistics is necessary to understand the gate control theory and to find out the dimensions of chronic pain as a problem. At first we will have a look at some of the statistics on chronic pain in Denmark and in Europe. After this a larger theory part will occur, containing theoretical parts about; synapses, somatic sensation, physiology of pain and treatment of chronic pain. All this will finally lead to a thesis statement. 2.0 Epidemiology of chronic pain Pain can be defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage [IASP-pain.org, 2009]. Furthermore, chronic pain can be defined as pain lasting longer than 6 months [Lindskog, 2004]. When pain becomes chronic it becomes a problem, both for the person who is in pain and the society. The prevalence of chronic pain in Denmark is 5 5th of January 2010 Industrial Medicine University of Aalborg about 16% [painineurope.com, 2009] and the incidence is positive with approximately 6000-7000 further patients each year [Eriksen & Sjøgren, 2006]. The patients with chronic pain are seen to be very affected of their state. A minor group of the patients is treated by specialized pain centers. Within this group only 14 % are working and 50 % were forced to take early retirement. Furthermore, nearly 50 % of this group are suffering from anxiety and depressive conditions, which reduce their quality of life [Eriksen & Sjøgren, 2006]. Those who have the greatest risk of getting chronic pain are women, people with a short education, elderly persons and people who find their own health condition poor. These persons are as well the persons who are often attending the general practitioner, which can have an influence on these statistics [Eriksen & Sjøgren, 2006]. People with chronic pain are using the healthcare system twice as much as people without pain, which represent a heavy burden on the society. The expenses for healthcare are consisting of diagnostics and treatments, but also the reduced ability to work and the loss of working days are great expenses to the society. The loss of working days in Denmark is estimated to about 1 million days each year [Eriksen & Sjøgren, 2006]. Chronic pain is frequently localized in the musculoskeletal system. These conditions cost the society in Denmark 13-15 billion each year, covering treatment, social benefits, pension etc [Uldall, 2008]. Chronic pain is not only a problem in Denmark. In 2003 Pain in Europe – A report was carried out by NFO WorldGroup and published. This is the largest survey so far with data from 46,394 persons distributed among 16 countries in Europe, including Denmark. The results showed that 19% of the adults in Europe suffer from chronic pain and that one third finds their pain severe, defined by a pain scale from 1 to 10. The report also focused on the causes of chronic pain and showed that arthritis/osteoarthritis is responsible for 34% and therefore is the most frequent cause. Other frequent causes are herniated/deteriorating discs, traumatic injury, rheumatoid arthritis and migraine headaches [Fricker, 2003]. Pain in Europe – A report shows that quality of life is highly affected by chronic pain. In the survey 27% said that they were less able or unable to maintain relationships with friends and family, while 19% were no longer able to have sexual relations. People with chronic pain also feel socially isolated. This problem is most acute in Denmark where 50% feel unable to discuss their pain with other people. Also lowered self-esteem, employee termination, depression, sleeping problems etc. are a big part of these persons everyday life. These facts show that it is a big problem. The fact that 6 5th of January 2010 Industrial Medicine University of Aalborg one fifth will have to live with these problems for more than 20 years makes it even worse and more important to resolve [Fricker, 2003]. Before looking specifically at pain and its physiology, it is important to look more generally at the mechanisms behind touch and nociception. In this context it is necessary to understand the neural processes involved. The following chapters include a discussion of the synapses of the nervous system, the somatic sensation and the pathways for different sensations from receptor to brain. 3.0 The neural processing 3.1 The Synapse The synapse is the place where the axon terminal part of a neuron passes information on to another neuron or an effector, which can be a gland or a muscle. It consists of two parts, a presynaptic side and a postsynaptic side, with a space between called the synaptic cleft. The direction of transmission is from the presynaptic to the postsynaptic side [Tortora, 2005]. The chemical synapse is an electrical-to-chemical-to-electrical transformation. The presynaptic axon terminal contains small membrane-enclosed spheres, called synaptic vesicles, which stores neurotransmitters. Neurotransmitters are the chemicals used to communicate with the postsynaptic cell. When the electrical transmission arrives to the terminal axon the transmission becomes chemical in shape of the neurotransmitters. An important part of the release of neurotransmitters is that voltage-gated calcium channels opens, when action potentials cause depolarization of the terminal membrane. The elevation in Ca2+ in the presynaptic cell causes a release of neurotransmitters from the synaptic vesicles by exocytosis. The neurotransmitters fuse to the postsynaptic side where receptors convert the intercellular chemical signal, the neurotransmitters, into an intracellular signal, which could be a change in the membrane potential or a chemical change. At the same time some of the neurotransmitters become a subject of enzymatic degradation, others are re-uptaken by the presynaptic cell and some diffuse away from the cleft [Bear et al, 2007; Stanfield & Germann, 2008]. 7 5th of January 2010 Industrial Medicine University of Aalborg 3.2 Neurotransmitter’s receptors The neurotransmitter’s receptors are an important part of the transmission. The receptors are found in over 100 different sorts, but mainly they can be classified in two types: transmitter-gated ion channels and G-protein-coupled receptors. Transmitter-gated ion channels consist of 4-5 subunits that come together and form a pore in the membrane. Normally the pore is closed, but when neurotransmitters bind to a specific side on the channel the subunits make a slight twist and the pore opens. If the channel is permeable to Na+, the effect will, as a rule, be a depolarization of the postsynaptic cell from the resting membrane potential. Because this brings the membrane potential toward threshold for generating action potentials, the effect is said to be excitatory. When this presynaptic release of neurotransmitters causes a postsynaptic membrane depolarization, it is called an excitatory postsynaptic potential (EPSP). Activation of ACh-gated and glutamate-gated ion channels cause EPSPs [Bear et al., 2007]. The opposite happens when the channels are permeable to Cl-. The effect is a hyperpolarization of the postsynaptic cell compared to the resting membrane potential, which brings it away from the threshold for an action potential. Therefore, a transient hyperpolarization of the postsynaptic membrane potential is caused by the presynaptic release of neurotransmitters. This is called an inhibitory postsynaptic potential (IPSP). IPSP is caused by synaptic activation of glycine-gated and GABA-gated ion channels [Bear et al., 2007]. The other type of receptors, G-protein-coupled receptors, often manages more slowly, longerlasting and more diverse postsynaptic actions. Broadly, there are three steps for these actions to happen: 1. Neurotransmitters bind to receptor proteins enclosed in the postsynaptic membrane. 2. The receptor proteins activate G-proteins that freely can move along the intracellular face of the postsynaptic membrane. 3. The now activated G-proteins activate effector proteins. The effector proteins can be G-protein-gated ion channels in the membrane, which react by opening or closing. It can also be enzymes synthesizing molecules called second messengers. These diffuse in the cytosol, where they can activate additional enzymes that regulate ion channel functions and alter cellular metabolism [Bear et al., 2007]. 8 5th of January 2010 Industrial Medicine University of Aalborg With the knowledge of the principles of the synapse, it is now possible to look into the physiology of somatic sensation and nociception. 4.0 Somatic sensation and nociception In order to understand the Gate Control Theory, which will be discussed later, it is important to know the principles of somatic sensation and nociception. Both touch and pain are perceived through sensory signals. Firstly, the receptors detect the stimulus and the sensory signal is then transmitted through two major pathways. These are the dorsal column-medial lemniscus system and the anterolateral system. Somatic sensation includes tactile sensation and proprioception. The last mentioned is not relevant in this report and therefore will not be discussed. The following will concentrate on the tactile sensation, which provide sensory information about the body and the environment, including touch, pressure, itch and vibration [Seeley, 2008]. The discussion of tactile sensation will lead to a review of nociception including the anterolateral system. 4.1 Tactile receptors There are at least eight major types of sensory receptors. The receptors primarily responsible for light touch are Merkel’s discs and hair follicle receptors, whereas the main function of the Ruffini end organs and the Pacinian corpuscles are to sense respectively continuous touch or pressure, vibration and deep cutaneous pressure. The so-called Meissner’s corpuscles have the unique function of two-point discrimination. Furthermore, receptors called free nerve endings exist, which are able to sense pain, itch, tickling, temperatures and joint movement [Guyton & Hall, 2006; Seeley, 2008]. 4.2 Tactile pathway The sensory receptors throughout the body enter the spinal cord by the dorsal roots of the spinal nerves. The dorsal column-medial lemniscus pathways are involved in the signalling of tactile stimulation and as the name implies, carries Figure 2: Illustrate the dorsal-columnsignals upward to the medulla of the brain - primarily in the medial lemniscal system. See text for details [Seeley et al, 2008]. 9 5th of January 2010 Industrial Medicine University of Aalborg dorsal columns of the spinal cord as shown in Figure 2. Many primary neuron axons of the system enter the cord and ascend the entire length of the spinal cord, without crossing to its opposite side, and synapse with secondary neurons located in the medulla oblongata. They continue upward through the brain stem to the thalamus by way of the medial lemniscus [Guyton & Hall, 2006; Seeley, 2008]. The functions of the dorsal column-medial lemniscal system are shown in Table 1. Table 1: Type of sensation for the dorsal column-medial lemniscal system [Guyton & Hall, 2006]. Dorsal column-medial lemniscal system Touch sensations requiring a high degree of localization of the stimulus Touch sensation requiring transmission of fine gradations of intensity Physic sensations, such as vibratory sensations Sensations that signal movement against the skin Position sensations having to do with fine degrees Pressure sensations having to do with fine degrees of judgment of pressure intensity As mentioned, the anterolateral system transmits pain among other senses and we will now go into the physiology of pain and the specific anterolateral pathways for pain transmission. 4.5 Physiology of nociception and pain Nociception is defined as the neural processes of encoding and processing noxious stimuli [IASPpain.org]. Pain occurs whenever any tissue is being damaged or at risk of being damaged, and it causes the individual to remove the body from the pain stimulus. The body’s reactions to pain protect us against harmful damages. If the pain sensation lacks or is poorly developed even daily activities could cause life-threatening injuries [McCance & Huether, 2006]. There are two major types of pain: fast pain and slow pain. Fast pain is felt within about 0.1 second after a pain stimulus is applied, whereas slow pain begins after 1 second or more and then increases slowly [Guyton & Hall, 2006]. The transduction of painful stimuli occurs in the free nerve endings of unmyelinated C fibres and lightly myelinated Aδ fibres. Pain can be evoked by mechanical, thermal and chemical pain stimuli. Nociceptors that respond to all three types of pain stimuli are called polymodal nociceptors. Some nociceptors show selectivity in their response to different stimuli and are called mechanical 10 5th of January 2010 Industrial Medicine University of Aalborg nociceptors, thermal nociceptors or chemical nociceptors [Bear et al., 2007]. In general, fast pain is evoked by the mechanical and thermal types of stimuli, whereas slow pain can be evoked by all three types. Bradykinin, serotonin, histamine, potassium ions, acids, acetylcholine, and proteolytic enzymes are some of the chemicals that excite the chemical type of pain. In addition, prostaglandins and substance P increase the sensitivity of pain endings but do not directly excite these [Guyton & Hall, 2006]. The nociceptors are all free nerve endings. They are widespread in the superficial layers of the skin as well as in certain internal tissues. The free nerve endings bring information to the CNS at different rates, because of the differences in their action potential conduction velocities [Bear et al., 2007]. The fast pain signals are transmitted in the peripheral nerves to the spinal cord by small type Aδ fibres at velocities between 6 and 30 m/sec. The slow pain is transmitted to the spinal cord by type C fibres at velocities between 0.5 and 2 m/sec. The pain signals take two pathways to the brain: the neospinothalamic tract and the paleospinothalamic tract. Both are a part of the anterolateral system and the so-called lateral spinothalamic tracts [Guyton & Hall, 2006]. But before discussing the two pathways, it is important to understand the anatomy of the spinal cord. 4.6 Spinal cord The spinal cord consists of a peripheral white portion and a central gray portion. The white part contains myelinated axons that form the nerve tracts, and the gray part contains neuron cell bodies, dendrites and axons. An anterior and a posterior sulci partly divide the cord into two halves, where the white matter in each half is divided into three columns that again are subdivided into tracts, or so-called pathways. Ascending or descending axons are grouped together within these tracts and carry action potentials essentially with the same type of information. The central gray matter is structured into horns; the dorsal, ventral, and lateral horns. They are divided into laminaes which are defined by their cellular structure rather than their location, but have an approximately fixed location. As an example fast Aδ fibres terminate mainly in lamina I and the slow C fibres terminate in laminae II and III. Furthermore the lamina II is the Substantia Gelatinosa which is important to know in a later chapter [McCance & Huether, 2006]. The two halves of the cord are connected by gray and white commissures which contain axons that cross from one side of the spinal cord to the other side [Seeley et al., 2008]. 11 5th of January 2010 Industrial Medicine University of Aalborg On the ventral and dorsal surface of the spinal cord are so-called rootlets running along. 6-8 rootlets combine to form each root which on the ventral side are called the ventral roots and on the dorsal side are called the dorsal roots. These roots extend to the lateral side of the spinal cord and join to form a spinal nerve. Furthermore, each dorsal root contains a dorsal root ganglion which is a collection of cell bodies of the sensory neurons that make the dorsal roots of the spinal nerves. A peripheral nerve has its free nerve endings remote and its cell body in the dorsal root ganglion. It does not synapse with the second-order neuron before it reaches, in most cases, the posterior horn of the spinal cord [Seeley et al., 2008]. After the synapse with the second-order neuron it continues through the lateral spinothalamic tracts to the brain, which will be described in the following paragraphs. See Figure 3 for an illustration. 4.7 Neospinothalamic tract The neospinothalamic pathway transmits pain mainly from the fast type Aδ fibres. These terminate mainly in lamina I of the dorsal horns and there they excite second-order neurons of the neospinothalamic tract. These second-order neurons give rise to Figure 3: Illustrate the Spinothalamic tract of the Anterolateral System [Seeley et al, 2008]. long fibres that cross immediately to the opposite side of the cord through the anterior commisure and then turn upward, passing to the brain in the anterolateral columns. A few fibres of the neospinothalamic tract terminate in the reticular areas of the brain stem, but most pass all the way to the thalamus without interruption, terminating in the ventrobasal complex*. A few fibres also terminate in the posterior nuclear group of the thalamus, and from these thalamic areas the signals are transmitted to other basal areas of the brain as well as to the somatosensory cortex. It is believed that glutamate (an amino acid) is the neurotransmitter secreted in the spinal cord at the type Aδ pain nerve fibre endings [Guyton & Hall, 2006]. 4.8 Paleospinothalamic tract The paleospinothalamic pathway transmits pain mainly from the peripheral slow type C pain fibres; although it does transmit some signals from type Aδ fibres as well. The peripheral fibres terminate in the spinal cord almost entirely in the laminae II and III of the dorsal horns. Most of the signals 12 5th of January 2010 Industrial Medicine University of Aalborg then pass through one or more additional short fibre neurons within the dorsal horns themselves before entering mainly lamina V. Here the last neurons in the series give rise to long axons that mostly join the fibres from the fast pain pathway. The slow paleospinothalamic pathway terminates widely in the brain stem. Only one tenth to one fourth of the fibres passes all the way to the thalamus. Most fibres terminate in one of three areas: the reticular nuclei of the medulla, pons and mesencephalon*, the tectal area of the mesencephalon* or the periaqueductal gray region surrounding the aqueduct of Sylvius*. From the brain stem pain areas multiple short-fibre neurons relay the pain signals upward into the intralaminar nuclei* and ventrolateral nuclei* of the thalamus and into certain portions of the hypothalamus and other basal regions of the brain. Research experiments suggest that type C pain fibre terminals entering the spinal cord secrete both glutamate and substance P transmitter. The glutamate transmitter acts instantaneously and lasts for only a few milliseconds. Substance P (a neuropeptide) is released much more slowly, building up in concentration over a period of seconds or even minutes [Guyton & Hall, 2006]. The areas of the brain, where the slow type of pain terminates, are; the reticular areas of the brain stem and the intralaminar nuclei of the thalamus, as just mentioned. These areas have an arousal effect on the nervous activity in the brain. This makes the person awake and explains why people in severe pain have difficulty sleeping which is a serious problem in people with chronic pain [Guyton & Hall, 2006]. 4.9 Pain control system It is very different how a person reacts to pain. One reason could be that the brain itself is capable of suppressing input of brain signals to the nervous system by activating a pain control system. This system consists of three major components: The periaqueductal gray and periventricular areas of the mesencephalon* and upper pons, the raphe magnus nucleus* and the nucleus reticularis paragigantocellularis* and a pain inhibitory complex located in the dorsal horns of the spinal cord, which is also called the gate control system. These three components are illustrated in Figure 4. First, neurons from the periaqueductal gray and periventricular areas send signals to the raphe magnus nucleus and the nucleus reticularis paragigantocellularis. From these nuclei, second-order signals Figure 4: Shows the analgesia system of the brain and spinal cord [Guyton & Hall, 2006]. 13 5th of January 2010 Industrial Medicine University of Aalborg are transmitted down the dorsolateral columns in the spinal cord to the pain inhibitory complex. At this point, the analgesia signals can block the pain before it is relayed to the brain. Electrical stimulation either in the periaqueductal gray area or in the raphe magnus nucleus can suppress many strong pain signals entering by way of the dorsal spinal roots, which will be outlined in a later chapter. Several transmitter substances are involved in the analgesia system; especially enkephalin and serotonin. Many nerve fibres from the paraventricular nuclei and from the periaqueductal gray area secrete enkephalin at their endings. With that the endings of many fibres in the raphe magnus nucleus release enkephalin when stimulated. Fibres originating in this area send signals to the dorsal horns of the spinal cord to secrete serotonin at their endings. The serotonin causes the local cord neurons to secrete enkephalin. The enkephalin is believed to cause both presynaptic and postsynaptic inhibition of incoming type C and type Aδ pain fibres where they synapse in the dorsal horns. With that the analgesia system can block pain signals at the initial entry point to the spinal cord [Guyton & Hall, 2006]. It is suggested that not only the physiological factors determine the perception of pain but also psychological aspects. Therefore, it is relevant to look into the psychological factors that can influence the pain signaling. 5.0 Psychological pain model Pain experience is not always only considered as something physical. Many scientists have also found that psychological aspects should be considered when dealing with pain. Professor Ronald Melzack has a theory about pain experience, which includes 7 processes. 1. The stimuli: Can be stimuli of different degree. 2. The receptor system: Consisting of nociception and the gate control mechanism, which receives, modulates and transmits the sensory information. 3. The cognitive processes: Especially conceptions linked to a stimulus, which can be from an earlier experience. Also the degree of attention is meant to have an Figure 5: Shows how the different components interact on each other. See text for more details [Friis-Hasché et al., 2004]. 14 5th of January 2010 Industrial Medicine University of Aalborg influence. 4. Emotion and motivation processes: Especially the degree of anxiety is thought to play a role in the perception. Psychic liability, discomfort, grief, hopelessness, stress, anger and other states of mind affect the perception. 5. Perception: The perceptual sensory system estimates if the stimuli shall be perceived as pain and in what degree. 6. Pain behavior: The reaction when a person experiences pain. 7. External factors: Nature and nurture are also thought to play a role in pain perception [FriisHasché et al., 2004]. These processes show that the perception of pain may not only be explained by physical processes as normally thought. It is clear that pain is a multidimensional experience and Figure 5 shows how the components interact on each other [Friis-Hasché et al., 2004]. The perception of pain is determined by many different factors; physiological, psychological and external factors and for that reason it can be difficult to treat patients in pain. The following chapter outlines the different treatment options for people with chronic pain. 6.0 Treatment of chronic pain Often the treatment of chronic pain is categorized into analgesic drugs and non-drug treatments. Analgesic drugs can furthermore be divided into opioid (narcotic) analgesics and non-opioid analgesics [Werner, 2009]. 6.1 Opioid analgesics Opioids can be either natural chemical substances or produced in a laboratory. Their effect is to bind to specified opioid receptors in the CNS, which trigger reactions that cause a change in the pain transmission in the neural pathways. The most known opioid is morphine, which is a strong opioid. However, a weaker opioid, as kodein, is more often used in the treatment of chronic pain [Sindrup, 2007; Werner, 2009]. 6.2 Non-opioid analgesics The most common non-opioid analgesics are nonsteroidal anti-inflammatory drugs (NSAID´s). NSAID´s reduce pain sensation and inflammation by reducing the production of prostaglandins, 15 5th of January 2010 Industrial Medicine University of Aalborg which functions are among others to stimulate pain receptors and causing blood vessels to dilate. The most common drug is acetylsalicylic acid, also known as aspirin [Sindrup, 2007]. Another often used non-opioid analgesic drug is paracetamol. This has no anti-inflammatory effect and practises its pain reducing effects in the posterior horn of the spinal cord [Sindrup, 2007; Werner, 2009]. 6.3 Non-drug treatments There are many different alternative treatment possibilities. A possibility is to apply cold or warm compresses directly to a painful area. Some also tries transcutaneous electrical nerve stimulation (TENS), which is a gentle electric current applied through electrodes placed on the skin's surface. Another method often used by persons with chronic pain is acupuncture which involves inserting tiny needles into specific areas of the body [Sindrup, 2007]. 6.4 Statistics of treatment in Europe In Europe 69% of the people with chronic pain are treating their condition with either prescription drugs, over the counter drugs or alternative treatments. Prescription drugs are the most often used; with NSAID´s representing 44%, weak opoids 23% and paracetamol 18%. Some do not find a solution to their pain in drug treatment. Two third are using at least one non-drug treatment for their pain – the most popular being massage, physical therapy and acupuncture. Generally, prescription drugs are perceived as more effective than non-prescription drugs and non-drug treatments. 45% find the treatment of prescription drugs "completely or very effective" versus 31% for nonprescription drugs and 38% for non-drug treatments. Still, these results leave numerous of people with a treatment that they do not find effective [Fricker, 2003]. Chronic pain is obviously difficult to treat. Based on the following chapters, it is now possible to give an overview of chronic pain and to outline the main focus of the rest of the report. 7.0 Thesis statement The epidemiology of chronic pain illustrates that one out of five people suffers from the condition and its subsequent problems. Thus, it is clear that chronic pain is a big problem, which becomes even bigger since many patients do not find the available treatments effective. 16 5th of January 2010 Industrial Medicine University of Aalborg After having outlined the basic principles of pain physiology and the treatment options, we find it relevant to explore the treatment options based upon the Gate Control Theory. The main focus will be on the use of transcutaneous electrical nerve stimulation (TENS) in the treatment of chronic pain. We want to explore the effectiveness of TENS and its future function as a treatment option. This leads us to the following thesis statement. “How can the concept touch inhibits pain be explained by the Gate Control theory and how is the theory used to treat chronic pain with transcutaneous electrical nerve stimulation?” 8.0 The Gate Control Theory of Pain In 1965 Ronald Melzack and Patrick D. Wall published a new theory of pain mechanisms. This theory was called the Gate Control Theory of Pain (GCT) Sufka & Price, 2002. The idea of the theory was that pain perception was not only a result of the activation of nociceptors but activation of non-nociceptive inputs also has an influence. This means that non-nociceptive signals can indirectly inhibit the pain signal from the nociceptors and therefore inhibit the pain perception. Melzack and Wall also proposed that the cognitive-modulation had an influence on the pain perception by variables such as past experience, attention and emotional state, which were mentioned in 5.0 Psychological pain model Melzack, 1993. Figure 6: The figure shows an illustration of the Gate Control theory. For more details see text [Sufka & Price, 2002]. 17 5th of January 2010 Industrial Medicine University of Aalborg The Gate Control Theory involves a series of events from receptor to pain perception as shown in Figure 6. When a stimulus is applied to a nociceptor, ongoing action potentials are, via the dorsal root ganglion, sent to a transmission neuron in the dorsal horn of the spinal cord. The action potentials are transmitted via a unipolar neuron where the cell body is located in the dorsal root ganglia. The action potentials are led to the axon terminal in the dorsal horn. From here it synapses with a second-order neuron, which is a transmission neuron (T-cell) that sends the action potentials to the action system e.g. via the lateral spinothalamic tract to a third-order neuron in the Thalamus. The Thalamus then spreads the action potentials to its dedicated regions of the brain Melzack, 1993; Melzack & Wall, 1965. Maybe the most important component of the theory is the Substantia Gelatinosa (SG) neuron. This is an interneuron that is connected with the nociceptive fibres, and it will try to inhibit the nociceptive action potentials at the nociceptive fibres´ presynaptic terminal. However, this will not take place in an event of pure nociceptive stimuli, because the nociceptive action potentials will always inhibit the interneuron. Hence no inhibitory effect will occur in this particular situation Melzack & Wall, 1965. The SG neuron is also connected to another type of sensory fibres. These fibres send action potentials from non-nociceptive receptors activated by touch. These fibres are connected to the SG neuron in a similar way as the nociceptive fibres. Contrary to the nociceptive fibres the nonnociceptive fibres activate the inhibitory effect of the interneuron. This stimulation of the interneuron will result in an inhibitory effect on both the non-nociceptive presynaptic terminal as well as the nociceptive presynaptic terminal. The overall effect of this will contribute to a decrease in the frequency of action potentials from the transmission neuron. Therefore, it will result in a decreased pain perception and in this way the Gate Control theory of Pain can conclude that touch inhibits pain Melzack & Wall, 1965. A criterion, which must be fulfilled for the touch inhibits pain theory, is that the transmission neuron must be a so-called Wide Dynamic Range (NS) neuron. This is a neuron that responds with increasing impulse frequency over a wide range of stimulus intensity. This means that it can respond to action potentials that are high and also low in frequency, from very gentle tactile stimulation to that which is clearly nociceptive e.g. tissue damage Sufka & Price, 2002. If the transmission neuron is a Nociceptive Specific (NS) neuron it will only respond to nociceptive stimuli and touch will not inhibit the pain Sufka & Price, 2002. 18 5th of January 2010 Industrial Medicine University of Aalborg In 1965 Melzack and Wall were aware of different factors that could influence their theory. They called these factors; central control triggers, which are descending fibres that can influence afferent signalling at the earliest synaptic levels of the somatosensory system. It is thought, but still not well documented, that this can alter the gate control system. Central control triggers can be cognitive factors such as attention, emotion and prior experience, e.g. anxiety or excitement may open or close the gate Melzack& Wall, 1965. Melzack and Wall proposed that two mechanisms; the dorsal column-medial lemniscus system and the dorsolateral path*, could activate selective brain processes that have control over the sensory input. These mechanisms are also called the dorsal column pathways and are often activated during sensory stimuli, and might be able to influence the gate control system. However, this is still a field that need more research Sufka & Price, 2002. The original theory has led to a broad dimension of research in the field of pain physiology. Since 1965 many studies have giving results that can now be added or discussed in relation to the original theory. The following chapter deals with the new knowledge. 8.1 Reconsideration of the theory In the article Gate Control Theory Reconsidered by Sufka and Price they believe that five major points in the original theory need to be reconsidered. These tenets are important improvements to the theory from 1965 and have developed parallel to the overall development of the understanding of the human body [Sufka & Price, 2002]. Tenet I The first major tenet of the Gate Control Theory is that primary sensory afferents are modulated in SG by interneurons. This process has shown to be more complex than first assumed but the main principle is still valid. Today’s knowledge of e.g. interneurons and neurotransmitters are described in depth. This has led to new more detailed diagrams of the theory, though the original diagram is still correct and widely used for the understanding of the main principles of the Gate Control Theory [Sufka & Price, 2002]. Tenet II The second tenet deals with the idea that non-nociceptive afferents and nociceptive afferents have a central effect on the SG interneuron and the transmission cell. It is known that stimulation from 19 5th of January 2010 Industrial Medicine University of Aalborg non-nociceptive and nociceptive afferents can result in inhibition during some conditions. The inhibition by stimulation from nociceptive afferents is due to a phenomenon called “diffuse noxious inhibitory control” (DNIC) where pain inhibits pain, which can be explained when two painful stimuli are applied remote from each other, then the strongest stimulus will inhibit the weaker stimulus [Pud et al., 2009]. Furthermore, not all T-cells can receive impulses from both nonnociceptive and nociceptive afferent. As mentioned earlier, only the WDR neuron can receive inputs from both. Additionally, the primary nociceptive afferents have different central effects and some C fibres can induce slow temporal summation*, which is only driven by C fibres inputs. For these several reasons, the original theory needs to be corrected to fulfil today’s knowledge of the central functions of the gate control system [Sufka & Price, 2002]. Tenet III The third tenet is that the original theory suggested that central control triggers could affect the gate control system. This has led to research that have shown different descending control systems which now can be a part of the explanation of the central control triggers [Sufka & Price, 2002]. There are mainly three types of descending mechanisms which inhibit the pain signals; direct inhibition of projection neurons*, activation of inhibitory interneurons*, and inhibition of primary afferents (presynaptic) and excitatory interneurons* [McMahon & Koltzenburg, 2006]. Furthermore, recent studies also suggest that it is likely that in the brain the ascending spinal pathways could trigger different mechanisms of descending modulation. This modulation can either have an inhibitory or facilitating effect on the gate control system. So today it is known that descending pathways can influence the perception of pain [Sufka & Price, 2002]. Tenet IV The fourth tenet also concern the central control triggers, which was partially based on Pavlov and Beecher´s observations* respectively in the year of 1927 and 1959. Today there is no evidence that these observations have a physiological influence on the gate control system. However, it is possible that the affective dimension of pain is modulated during the circumstances in these observations. Therefore it is possible that the perception of pain can be influenced by emotional states, as mentioned earlier, but there is still no evidence that physiological changes exist [Sufka & Price, 2002]. 20 5th of January 2010 Industrial Medicine University of Aalborg Tenet V The fifth tenet of the theory deals with the transmission neuron’s influence on the perception of pain. When a critical level of activity occurs in the T-cells, several brain areas that underlie the various dimensions of pain are activated. Most likely there are two criteria that must be fulfilled. Firstly there is now evidence that spatial and temporal summation* are important factors in the understanding of pain perception. If the impulse activity in T-cells is too low, no pain can be felt but tactile information is perceived. Furthermore, it is possible that the number of activated T-cells and their overall impulse frequencies need to exceed critical levels to evoke pain. For that reason there has to be enough stimulation to reach the threshold of the neuron to make it able to pass on the action potentials and additionally enough T-cells has to be stimulated. Secondly, the inputs from Tcells activate several brain structures simultaneously and these brain structures are thought to be involved in different dimensions of pain such as arousal, motoric orientation and autonomic activation. Therefore, several regions of the brain are involved in the perception of pain when enough T-cells are stimulated, and all these areas are important in the body’s reaction to a painful stimulus [Sufka & Price, 2002]. Today the original theory of the gate control system suggested by Melzack and Wall are still very relevant for the understanding of pain. Since 1965 research have added a great deal of information to the understanding of pain, which today can be added to the original Gate Control Theory, and these additions can answer many of the unanswered questions that Melzack and Wall had in 1965. The Gate Control Theory has set the scene for the possibility of using this knowledge to treat people with pain. 9.0 Electrical stimulation and the relief of pain With the gate control theory new acknowledgment about pain perception was discovered. This new insight helped scientific investigators to understand the reactions that happen when a person is exposed to pain. Touching the painful area is often seen, both in chronic pain like a rheumatic hip or a headache, or in an acute pain like hitting the knee. Why touching helps to inhibit pain was now explained with the Gate Control Theory [Seeley, 2008]. The theory also helped to understand why already used pain relieving methods showed results. The methods became more popular, and experiments that should explore their effects where composed. 21 5th of January 2010 Industrial Medicine University of Aalborg The methods, that developed to reduce the intensity of chronic pain, were massage, acupuncture, exercise and electric stimulation of the dorsal column-medial lemniscal neurons. They are all thought to increase the non-nociceptive stimulation and by this inhibit the pain, as mentioned in 8.0 Gate Control Theory [Seeley, 2008]. One of the methods that have been improved and specified since 1965 is electrical stimulation. Transcutaneous electrical nerve stimulation (TENS) is a sort of electrical stimulation, which has been used as treatment for chronic pain for more than 30 years [Sluka & Walsh, 2003]. TENS can be an option to treat patients with chronic pain but without the side effects which are often seen in drug treatments. TENS can also be a possible way to help persons who do not find any help in medicaments. To consider TENS as a treatment option, it is necessary to have more knowledge about the method and the existing evidence in the topic. 9.1 Principles of TENS Transcutaneous electrical nerve stimulation (TENS) is defined as the use of electrical stimulation to the skin for pain control [Sluka & Walsh, 2003]. TENS is the most often used electrotherapy for producing pain relief by stimulating the dorsal column-medial lemniscal neurons. It is popular because it is non-invasive, easy to use, has few side-effects and it is not very expensive [Johnson, 2008]. Clinically, TENS is used at different frequencies, intensities, and pulse durations of stimulation. TENS can be divided into two groups; Low-frequency TENS (LFTENS) which has a frequency lower than 10 Hz and High-frequency TENS (HFTENS) which has a frequency higher than 50 Hz [Desantana et al., 2008; Johnson, 2008]. Intensity is defined by the response of the patient, depending on whether the sensation is felt as comfortable or tolerable. Pulse duration is the time of each pulse. 9.2 Physical principles The electrical characteristics of TENS are the ability to activate different groups of nerve fibres as this is believed to produce different analgesic results. A standard TENS device causes a number of possible ways that TENS currents could be delivered, so it is important to review the principles of nerve fibre activation. Large diameter nerve fibres have low thresholds of activation to electrical stimuli when compared with small diameter nerve fibres [Johnson, 2008]. 22 5th of January 2010 Industrial Medicine University of Aalborg The current amplitude needed to stimulate a nerve fibre decreases with increasing pulse duration and frequency. Pulse duration of 10-1000µs provide the greatest separation and sensitivity of pulse amplitudes required to activate large diameter afferents, small diameter afferents and motor efferents. However, to activate large diameter fibres without activating smaller diameter nociceptive fibres you would use low-intensity, high-frequency currents with pulse duration between 10-1000µs [Johnson, 2008]. 9.3 Mechanisms of action Stimulation-induced analgesia can be categorized into peripheral, segmental and extrasegmental, according to the anatomical site of action [Johnson, 2008]. Peripheral mechanisms The delivery of electrical currents over a nerve fibre will cause nerve impulses that travel in both directions along the nerve axon, both in the antidomic* and the orthdromic* direction. TENS-induced nerve impulses which are travelling away from the CNS, the antidromic direction, will collide with the afferent impulses arising from the tissue damage and then extinguish the noxious stimulus [Johnson, 2008]. See Figure 7. Figure 7: TENS-induced blockade of peripheral transmission. [Johnson, 2008]. Segmental mechanisms Activity generated in Aβ fibres inhibits ongoing activity in the dorsal horn of the spinal cord. It has been demonstrated that in some types of HFTENS the analgesia effect is located in the spinal cord and it is probably a combination of pre- and postsynaptic inhibition which occurs. Activity in Aδ and C fibres from nociceptors leads to excitation of SG interneurons. TENS-induced activity in Aβ afferents leads to the facilitation of SG interneurons and inhibition of T cells via the release of GABA [Johnson, 2008]. 23 5th of January 2010 Industrial Medicine University of Aalborg Extrasegmental mechanism TENS-induced activity in small diameter muscle afferents has shown to produce extrasegmental analgesia through the activation of brainstems and thereby leading to activation of the descending pain inhibitory pathways [Johnson, 2008]. 9.4 Explanation of TENS by GCT The Gate Control Theory of pain is most commonly used to explain the inhibition of pain by TENS. The way TENS act on the gate control system is by sending stimuli, electrical impulses, which activates the afferent nerve fibers. This activates the SG interneuron, which then inhibit the small and also large diameter fibers before reaching the transmission neuron. In this way the frequency of impulses sent by the transmission neuron is dramatically decreased and the person’s perception of pain will be reduced. 9.5 The adverse effects of TENS One of the advantages of TENS is the relatively small amount of side effects. One problem for TENS can be adherence of electrodes and difficulty attaching electrodes which may lead to skin irritation like skin rash or a burning sensation over the electrode site, when treated. This is commonly due to dermatitis at the site where the skin is in contact with the electrodes, resulting from the components of the electrodes, the electrode gel or the adhesive tape [Johnson, 2008]. Although the side effects of TENS are at a minimum, therapists should be cautious when giving TENS to certain groups of patients. These groups can be patients suffering from epilepsy and women in the first trimester of pregnancy because the effects of TENS on foetal development are still unknown. Furthermore, patients with cardiac pacemakers should be cautious because the electrical field generated by TENS could interfere with the implanted electrical devices [Scherder, 1999]. TENS should not be applied internally in the mouth, or over areas of broken or damaged skin to avoid electrical skin burn [Johnson, 2008]. 9.6 The clinical use of TENS TENS is widely used in pain clinics in the management of various chronic pain conditions. It is used to treat diverse acute and chronic pain conditions, and although clinical studies of its long term efficacy have yielded variable results, it has become popular with both patients and health professionals of different disciplines [Nnoaham & Kumbang, 2009]. 24 5th of January 2010 Industrial Medicine University of Aalborg The most effective indications for TENS therapy are angina pectoris, failed laminectomy syndrome*, labor pain, post-herpetic neuralgia*, diabetic neuropathy and many mononeuropathies. Other applications are pain from radiculopathy*, compression syndromes*, spinal injury pain and, in some cases, referred visceral pain. TENS may also be very effective in certain acute pain conditions such as those arising from trauma. Some forms of postoperative pain can be treated with TENS, particularly after abdominal surgery and Caesarian section [Simpson, 2003]. The ongoing questions about the effectiveness of the use of TENS in humans have been addressed by various randomized placebo controlled trials. Warke et al. investigated the hypoalgesic effects of TENS in patients diagnosed with multiple sclerosis with a concurrent diagnosis of chronic low back pain. Ninety patients were randomly assigned to low-frequency TENS, high-frequency TENS, or shame TENS. Self-applied TENS treatments of 45 minutes twice daily (minimum) for six weeks yielded a significant effect between groups over time for average low back pain. These clinically important results suggest that high-frequency TENS had its greatest effects on pain reduction during the six weeks of treatment. Low-frequency TENS demonstrated positive long-term results at 32 weeks [Warke et al., 2006]. Use of TENS, in combination with other therapies, will allow patients to increase activity level, reduce hospital stay, and improve function. Treatment with TENS has shown to increase joint function in patients with arthritis. In patients with chronic low back pain, improvements have occurred with TENS. Postoperative TENS treatment in patients after thoracic surgery reduces recovery room stay and improves pulmonary function when compared to sham controls. Thus, decreasing pain with TENS increases function and allows the patient to tolerate other therapies and activities, resulting in an improved quality of life [Sluka & Walsh, 2003]. 10.0 Discussion Chronic pain is a serious problem and has a great influence on the patient’s life and the society. As mentioned in 2.0 Epidemiology, one out of five Europeans suffer from chronic pain. Because of the size of the problem it is important to investigate different treatment methods such as TENS. In this context it is necessary to look into different research studies. In 2009 the Cochrane Collaboration published a review about transcutaneous electrical nerve stimulation (TENS) for chronic pain. In this review 124 studies were considered, but only 25 studies with 1281 participants met the inclusion criteria. For instance, the trials had to be randomized controlled trials (RCT) and they had to investigate the analgesic effectiveness of TENS 25 5th of January 2010 Industrial Medicine University of Aalborg in adults with chronic pain. However, the Cochrane Collaboration estimated that only a few of the included studies were rated of good methodological quality and had performed well on randomization [Nnoaham & Kumbang, 2009]. The studies compared one or more types of TENS. 12 studies compared HFTENS and sham TENS, where eight showed active superior to sham. Another eight studies compared LFTENS and sham TENS, in which four showed active superior to sham. Further nine studies compared HFTENS and LFTENS, where two showed difference in effectiveness. These studies showed that HFTENS in 75% of the cases were more effective than sham TENS. Furthermore, only 50% of the participants receiving LFTENS found it effective compared to sham TENS. However, when the two types of TENS were compared, only a small difference in effectiveness was found. This shows that the results are contradictory [Nnoaham & Kumbang, 2009]. The authors found several factors that could improve the quality of the 25 studies. One problem could be the lack of a non-treatment group in most of the trials. This group should have been compared with both the placebo- and the active-TENS-group, to illustrate if the pain relief were due to the placebo effect or natural improvements. Another factor, that could refine these studies and future trials, could be to fulfill the many experts’ beliefs in this field [Nnoaham & Kumbang, 2009]. They believe that 30 to 40 minutes of stimulation twice a day for at least one month may be necessary to achieve significant pain relief, and this was not met in most of the 25 studies [Cheing, 2003]. For instance, about 80 % of the studies lasted less than four weeks and in 70% of the trials stimulation occurred less than ten hours per week, with 60% of the participants having less than ten sessions of TENS [Nnoaham & Kumbang, 2009]. This may explain why the results were not that convincingly. If the study designs were based upon the experts’ beliefs, more useful results could have been achieved. The lack of evidence-based studies makes it impossible for the Cochrane Collaboration to make a metaanalysis. The data found in the 25 studies were insufficient and the study designs were too different to compare [Nnoaham & Kumbang, 2009]. Despite the before mentioned factors, which reduced the standard of the trials, some positive results has been achieved. In 22 out of the 25 studies active TENS was compared with sham TENS and in 13 out of these 22 studies, they could conclude that TENS had a positive effect on chronic pain in one way or another. Other trials have also yielded positive effects of TENS for instance in the treatment of multiple sclerosis and chronic low back pain, as described in 9.6 The Clinical use of 26 5th of January 2010 Industrial Medicine University of Aalborg TENS. Thus, in some cases TENS is effective for the relief of chronic pain [Nnoaham & Kumbang, 2009]. Other advantages of TENS are the economic aspects. TENS is a cheap treatment option compared to long-term drug therapy; a TENS device is available from less than 250 Dkr [Johnson, 2008]. TENS is also cheaper for the society because patients with chronic pain receive a grant to pay for their medication. Additionally, TENS has few side effects compared to pharmacological treatments and is easy to administer for the patient. If TENS becomes effective in more patients it could resolve many of the problems caused by chronic pain. Besides the chronic pain the patients often suffer from anxiety and depressions, and they have a reduced quality of life. The pain and the subsequent problems often make the patients unable to work, which is a great expense for the society. Thus TENS could improve the patients’ quality of life and save the society a great amount of expenditures [Eriksen & Sjøgren, 2006]. So far in this report TENS has been explained by the gate control theory, which indicates that stimulation of large diameter afferents by TENS inhibits nociceptive fibres’ responses in the dorsal horn, but other theories exist [Sluka & Walsh, 2003]. Research suggests that the mechanisms of TENS can be explained by endogenous opioids. Studies show that TENS can result in the release of endogenous opioids, which activates the opioid receptors during different frequencies of TENS. This contributes to the analgesic system and the relief of pain [Sluka & Walsh, 2003]. The explanation of the mechanisms of TENS should probably be found in a combination of the GCT and the release of endogenous opioids. More evidence-based research is necessary in order to clarify the exact explanations of TENS and may be able to improve the treatment method [Sluka & Walsh, 2003]. When considering GCT and TENS it is evident that more research is needed. The purpose should be to get a better knowledge about the undiscovered mechanisms behind GCT and the effect of TENS. This knowledge is important in order to make the use of GCT in treatments like TENS more effective than today. In future research it might be helpful to consider the psychological aspects and the central control triggers in relation to better understand GCT and pain physiology in general, as mentioned in 5.0 Psychological Pain Model and in 8.1 Reconsideration of the theory. Both the psychological aspects and the central control triggers were already contemplated by Melzack when he and Wall developed the Gate Control Theory [Friis-Hasché et al., 2004]. Thus, the scientists should probably pay more 27 5th of January 2010 Industrial Medicine University of Aalborg attention to these factors in research than they do today. These factors should not only be present in the research of GCT, but also in the general research of pain. 11.0 Conclusion One of the aims of this report was to understand the concept touch inhibits pain by looking at the Gate Control Theory. This theory states that stimulation of large diameter afferents inhibits nociceptive fibres' responses in the dorsal horn via the SG interneurons. This means that when you feel pain, touch can affect the pain signaling and thereby reduce the pain perception. The second aim was to look into how the GCT is used to treat chronic pain with TENS. With this treatment afferents are stimulated by the TENS electrodes, which means that TENS indirectly represents the touch that inhibits the pain. When dealing with TENS it became clear that other theories could explain the mechanisms of TENS. One theory claims that TENS can result in the release of endogenous opioids, which then contribute to the analgesic effect. After all, the mechanisms of TENS can probably be explained by a combination of the theories. The effect of TENS as a treatment option is still unclear. Studies have yielded many different results which predominantly did not give convincing outcomes to support the use of TENS. One of the reasons that the results did not give a clear overview of the effect of TENS could be that the existing trials are of mixed quality. This is also why the results cannot be compared in a metaanalysis. More evidence-based research is necessary in order to clarify the effectiveness of TENS. Additionally, future research should consider if psychological aspects of pain perception must be included when designing the study and interpreting the results. If TENS shows to be an effective treatment option, it could help millions of people who daily suffer from chronic pain. In this way, the society and the patients will benefit from the concept touch inhibits pain. 28 5th of January 2010 Industrial Medicine University of Aalborg 12.0 Putting into perspective As we have progressed through the rapport it is now clear that chronic pain is a major problem both for the person suffering from chronic pain and socioeconomically. As mentioned in the conclusion better methodology quality research is needed in order to increase the effectiveness of the use of TENS. The cost for the society and the social cost for the persons suffering from chronic pain are enormous. As mentioned earlier, the Danish Health Care System used 13-15 billion Danish kroner in 2008. The prediction, we are about to make, is based on the premises that more research shows how to effectively use TENS on almost every person suffering from chronic pain. In this scenario the cost for the society and the social cost will be heavily reduced. We visualize a society where all patients suffering from chronic pain will get treated by the use of TENS. This will lead to a relief of pain, a decrease in cases of e.g. anxiety and depression, which then will result in a higher quality of life for the persons and increased working force in general. As this is less likely to happen, a more realistic future landmark would be a combination of TENS and drugs or maybe other alternative treatments e.g. acupuncture, where TENS being the most dominating factor. We believe that more research will help to reduce the amount of drugs now used in treatments by a substitution of TENS. This will be far more economic and also give fewer side effects and therefore give the person suffering a better quality of life. 29 5th of January 2010 Industrial Medicine University of Aalborg 13.0 Explanations of words Activation of inhibitory interneurons: the periaqueductal grey and the rostral ventromedial medulla in the midbrain can excite inhibitory interneurons in the dorsal horn, which then release GABA and glycine that have an inhibitory effect on the firing of nociceptive neurons and thereby it contribute to the descending controls [McMahon & Koltzenburg, 2006]. Antidromic: nerve impulse that run in the physiological abnormal direction [Lindskog, 2004]. Compression syndrome: symptoms which occur when an organ is exposed to (longterm) compression [Lindskog, 2004]. Direct inhibition of projection neurons: brain stem neurons directly inhibit projecting nociceptive dorsal horn cells (T cells). This can occur when the rostral ventromedial medulla (RVM) produce a monosynaptic inhibitory postsynaptic potential in neurons of the spinothalamic tract [McMahon & Koltzenburg, 2006]. Dorsolateral path: a descending pathway where the majority of the fibres crosses to the opposite site in the lower medulla and descend into the lateral corticospinal tracts of the spinal cord [Guyton & Hall, 2006]. Failed laminectomy syndrome: failure of the surgical procedure involving removal of one or more vertebral laminae in order to relieve the symptoms of a spine stenosis or to access the vertebral canal [Tortora, 2005; Lindskog, 2004]. Inhibition of primary afferents (presynaptic) and excitatory interneurons: descending signals can inhibit the pain perception by exciting opioid inhibitory interneurons in the dorsal horn. Then these interneurons can, via opioid receptors, either presynaptically inhibit the release of neurotransmitters from the primary afferents, or inhibit excitatory interneurons postsynaptically [McMahon & Koltzenburg, 2006]. Intralaminar nuclei of the thalamus: lie within the internal medullary lamina and make connections with the reticular formation, cerebellum, basal ganglia and wide areas of the cerebral cortex. They function in pain perception, integration of sensory and motor information and arousal [Tortora, 2005]. Laparoscopic surgery: an operation method where you examine the contents of the peritoneum with a laparoscope (a type of endoscope) passing through the abdominal wall [Tortora, 2005; Lindskog, 2004]. 30 5th of January 2010 Industrial Medicine University of Aalborg Nucleus reticularis paragigantocellularis: one of the major components of the rostral ventromedial medulla, which is involved in nociceptive processing and pain modulation [Semnanian et al., 1998]. Ortodromic: nerve impulse that run in the physiological normal direction [Lindskog, 2004]. Pavlov and Beecher´s observations: Pavlov’s observations were about dogs that showed little pain behaviour when food was paired with the noxious stimuli. Beecher’s observations were about wounded soldiers who showed much less pain behaviour than comparable wounded civilians [Sufka & Price, 2002]. Periaqueductal gray areas of the mesencephalon and upper pons: also called the periaqueductal gray region and abbreviated PAG. The area plays a role in the descending modulation of pain. It is called the epicenter of analgesia [McMahon & Koltzenburg, 2006]. Periaqueductal gray region surrounding the aqueduct of Sylvius: see Periaqueductal gray areas of the mesencephalon and upper pons. The aqueduct of Sylvia is a narrow channel in the midbrain connecting the third and fourth ventricles and containing cerebrospinal fluid [Encyclopedia Britannica, 2009]. Periventricular areas of the mesencephalon and upper pons: the part of mesencephalon and upper pons located near the ventricles. Together with periaqueductal gray areas of the mesencephalon and upper pons it plays a role in the analgesia system [Merriam-Webster, 2009; McMahon & Koltzenburg, 2006]. Post-herpetic neuralgia: a longterm pain condition after shingles in the area of the trigeminal nerve [Lindskog, 2004]. Radiculopathy: illness of a root/nerve root. In this case it is back pain [Lindskog, 2004]. Raphe magnus nucleus: a nucleus located in the rostral ventromedial medulla of the brainstem and stimulated from axons in the spinal cord and cerebellum. The main function is pain mediation. It sends projections to the dorsal horn of the spinal cord to directly inhibit pain and it receives descending afferents from the periaqueductal gray, amygdala etc. [Encyclopedia Britannica, 2009]. Reticular nuclei of the medulla, pons and mesencephalon: nuclei found in the reticular formation of the brainstem, which is the core of the brain stem [Encyclopedia Britannica, 2009]. 31 5th of January 2010 Industrial Medicine University of Aalborg Slow temporal summation: action potentials from a single presynaptic terminal, if they occur rapid enough, can add to one another and summate so the threshold is reached [Guyton & Hall, 2006]. Spatial and temporal summation: spatial summation is the effect of summing simultaneous postsynaptic potentials by activating multiple terminals on the neuronal membrane to reach the threshold. Temporal summation is described just above [Guyton & Hall, 2006]. Tectal area of the mesencephalon: a roof-like structure in the dorsal portion of the midbrain, formed by the quadrigemina bodies/optic lobes, which help to cross several fibres of the optic nerve [Encyclopedia Britannica, 2009]. Unilateral inguinal herniorrhaphy: stitching up a hernia sac on one side of the groin [Lindskog, 2004]. Ventrobasal complex: the complex is the combination of two nuclei of the thalamus: nucleus ventralis posterolateralis and nucleus ventralis posteromedialis. It receives sensory input from the medial lemniscus, from spinothalamic tracts and from the trigeminal nerve. It subsequently relays the inputs to the primary sensory area of the cerebral cortex. Synchronously, it distinguishes sensory inputs from deep sensory receptors from cutaneous inputs [Encyclopedia Britannica, 2009]. Ventrolateral nuclei of the thalamus: relay impulses from the cerebellum and basal ganglia to motor parts of the cerebral cortex. Its neurons are active during movements on the opposite side of the body [Tortora, 2005; Bjarkam, 2009]. 32 5th of January 2010 Industrial Medicine University of Aalborg 14.0 List of references Bear, M. F., Connors, B. W. & Paradiso, M. A., 2007. Neuroscience – exploring the brain. 3rd edition. Lippincott Williams & Wilkins. Bjarkam, C. R., 2009. Neuroanatomi. Munksgaard Danmark. 1st edition, issue 4. Cheing, G., Tsui, A., Lo, S. & Hui, C., 2003. Optimal stimulation duration of tens in the management of osteoarthritic knee pain. Journal of Rehabilitation Medicine: 35: 62–8. DeSantana, P.T., Josimari, M., Deirdre, M.., Walsh, P.T., Carol Vance, P.T., Barbara, A., Rakel, R.N. & Sluka, K., 2008. Effectiveness of Transcutaneous Electrical Nerve Stimulation for Treatment of Hyperalgesia and Pain. Curr Rheumatol Rep: December; 10(6): 492–499. Encyclopedia Britannica, 2009. Nucleus raphe magnus; Sylvian fissure; Tectum mesencephalon; Ventrobasal complex. Encyclopedia Britannica Online. 2nd of December. Eriksen, J. & Sjøgren, P., 2006. Epidemiologiske forhold vedrørende langvarige/kroniske noncancersmertetilstande i Danmark. Ugeskrift for læger, 168(20); 1947. Fricker, J., 2003. Pain in Europe – A report. NFO WorldGroup. Friis-Hasché, E., Elsass, P. & Nielsen, T., 2004. Klinisk sundhedspsykologi. Munksgaard Danmark. Granger, R. H. & Hearn, R. A., 2007. Models of thalamocortical sytem. Scholarpedia, 2(11); 1796. Guyton, A. C. & Hall, J. E., 2006. Textbook of medical physiologi. 11th edition. Elsevier Inc. IASP-pain.org [Seen 16th of December 2009]. Johnson, M., 2008. Electrotherapy: evidence-based practice. 12th edition. Elsevier Ltd. Lindskog, B. I., 2004. Medicinsk ordbog. Gyldendal. McCance, K. L. & Huether, S. E., 2006. Pathophysiology; The Biologic Basis for Disease in Adults and Children, 5th edition. Elsevier Mosby. 33 5th of January 2010 Industrial Medicine University of Aalborg McMahon, S. B. & Koltzenburg, M., 2006. Wall and Melzack’s Textbook of Pain. 5th edition. Elsevier Limited. Melzack, R., 1993. Pain: Past, present and future. Canadian Journal of Experimental Psychology. Ottawa: Dec. Volume 47, issue 4; 615. Melzack, R. & Wall, P.D., 1965. Pain Mechanisms: A New Theory. Science 19th of November. Volume 150, number 3699; 971-979. Merriam-Webster, 2009. Periventricular. Merriam-Webster Online. 2nd of December. Miller, G. A., Fellbaum, C., Tengi, R., Wakefield, P. & Langone, H., 2009. The Trustees of Princeton University. Search=sensation. Available at http://wordnet.princeton.edu [Seen 12th of November 2009]. Nnoaham, K. E. & Kumbang, J., 2009. Transcutaneous electrical nerve stimulation (TENS) for chronic pain (Review). The Cochrane Collaboration. John Wiley and Sons, Ltd. Painineurope.com [Seen 16th of December 2009]. Pud, D., Granovsky, Y. & Yarnitsky, D., 2009. The methodology of experimentally induced diffuse noxious inhibitory control (DNIC)-like effect in humans. Pain; 144: 16-19. Scherder, E., Van Someren, E. & Swaab, D., 1999. Epilepsy: a possible contraindication for transcutaneous electrical nerve stimulation. Journal of Pain and Symptom Management: 17; 152–153. Seeley, R. R., Stephens, T. D. & Philip, T., 2008. Anatomy & Physiology. 8th edition. McGraw-Hill. Semnanian, S., Gheibi, N., Fathollahi, Y. & Haghparast, A., 1998. Responsiveness of the nucleus reticularis paragigantocellularis neurons to the formalin as a peripheral noxious stimulus. Elsevier. Simpson, B. A., 2003. Electrical Stimulation and the Relief of Pain. Volume 15. Elsevier B.V. Sindrup, S. H., 2007. Basal og klinisk farmakologi. 3rd edition. Fadl´s forlag. Sluka, K. A. &Walsh, D., 2003. Transcutaneous Electrical Nerve Stimulation: Basic Science Mechanisms and Clinical Effectiveness. The Journal of Pain. Volume 3; 4: 109-121. 34 5th of January 2010 Industrial Medicine University of Aalborg Stanfield, C. L. & Germann, W. J., 2008. Human Physiology. 3rd edition. Pearson. Sufka, K. J. & Price, D.D., 2002. Gate Control Theory Reconsidered. Brain and Mind; 3: 277-290. Tortora, G. J., 2005. Principles of Human Anatomy. 10th edition. Wiley. Uldall, H., 2008. Kiropraktikken i samfundet. Available at http://netdoktor.dk [Seen 5th of November 2009]. Warke, K., Al, S., Baxter, D., Walsh, D. & Lowe, S. 2006. Efficacy of transcutaneous electrical nerve stimulation tens for chronic low-back pain in a multiple sclerosis population: a randomized, placebo-controlled clinical trial. The Clinical Journal of Pain; 22: 812–9. Werner, M., 2009. Smertebehandling. Available at http://medicin.dk [Seen 10th of November 2009]. 35