Assessment and Management of ConstipationPrezi
advertisement
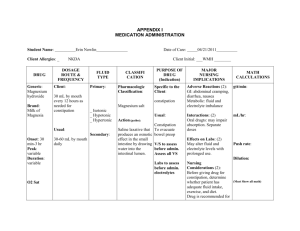
Assessment and Management of Constipation Emily Booth RN BScN MN PHC-NP NURSE LED OUTREACH TEAM Agenda Definition Types/Classification Causes Anatomy and Physiology Bowel Assessment Treatment Summary/Conclusion What is Constipation? One or more of… Excessive straining with bowel movement Sense of incomplete emptying with BM Failed or lengthy attempts to defecate Hard stools Decreased stool frequency Prevalence Most common digestive complaint 4.53 million people per year 2.5 million physician visits per year Twice as common in women than men 2 fold increase in LTC residents Types of Constipation Types of Constipation Primary Causes: Disorder of neuromuscular function and brain- gut function Slow transit time (decreased propulsion of stool) Evacuation disorders (incoordination of contractions or inadequate relaxation of pelvic floor muscles during defecation) IBS (genetic, environmental, social, biological, psych factors) Types of Constipation Secondary Causes: other conditions Dietary – inadequate fluid intake and dietary fibre Behavioural – decrease physical activity, failure to respond to initial urge to defecate, chronic use of stimulant laxatives Metabolic – hypercalcemia, hypothyroid Neurologic – parkinsons, spinal cord lesions, DM Disease of the colon – strictures, fissures, ca Anatomy and Physiology Anatomy and Physiology Colon – divided into ascending colon ( from cecum to edge of liver border), goes across the abdomen under the stomach called the transverse colon and then descends down the left side of the abdomen (descending colon)and leads into the sigmoid colon and rectum Ascending and transverse colon absorb H2O and electrolytes Descending and sigmoid colon stores fecal matter until eliminated Smooth muscle of colon contracts and relaxes in response to distension and mixing movements occur Contents of colon enter the rectum usually q am Spinal reflex to defecate occurs and the anal sphincter relaxes or contracts with pelvic and abdominal muscle movement Risk Factors for Older Adults Diet low in fibre Poor or reduces oral fluid intake Low level of physical activity or immobility Advanced age Overuse of laxatives Endocrine/metabolic disease (diabetes, hypothyroid, hypercalcemia, hypokalemia) Neurologic disease (stroke, MS, parkinsons) Disease of the colon (diverticulitis, IBS) Medications (anticholinergic drugs) Drug Induced Constipation OPIOIDS Cause Constipation Codeine, morphine, oxycodone, fentanyl patch The Hand that Writes the Narcotic Writes the Cathartic Drug Induced Constipation Antinauseant Antiparkinson meds Alzheimers meds Iron supplements Incontinence meds Antacids Ulcer meds Antidepressants Antipsychotics Antihypertensives Lipid lowering drugs Quality of Life Pain, discomfort, bloating Lack of appetite Nausea Fatigue Irritability Change in behaviour Haemorrhoids, prolapse Fecal impaction , diarrhea Bowel Assessment The most essential step is determining the etiology or cause Usual bowel pattern and measures currently used Hx of problem Ability to sense urge to defecate Daily fluid and fibre intake Relevant medical/surgical hx Functional abilities 7 day bowel record Physical assessment Treatment First line acute Treat underlying cause Diet and lifestyle measures Prunes and /or stool softener If impacted , enema/suppository/disimpaction and stimulant laxative Ongoing Constipation First line Treat underlying cause Diet/lifestyle measures Bulk laxative (metamucil/psyllium) or prunes, and/or stool softener Second line Diet/lifestyle measures Osmotic laxative (lactulose, mg containing laxatives) Third line Diet/lifestyle measures Osmotic laxative (lactulose, glycerin, PEG or mg containing products – MOM, citromag fleet) Stimulant laxative (senna, castor oil or dulcolax) if no BM x 3 days Laxatives Caution with bulk forming laxatives in elderly , may cause obstruction Stool softeners are not to be used alone for constipation. Little value for chronic constipation. Help with pain and straining with defecating Pharmacologic Considerations Meds do have a place in the treatment of constipation Short term, time limited Choose laxatives based on resident symptoms and hx Use homes bowel protocol Summary Focus is on prevention Resident specific interventions Staff communication ( 7 day bowel record and ongoing monitoring) In house bowel protocol Pharmacological interventions The End