Constipation in Adults - Gloucestershire Hospitals NHS Trust
advertisement
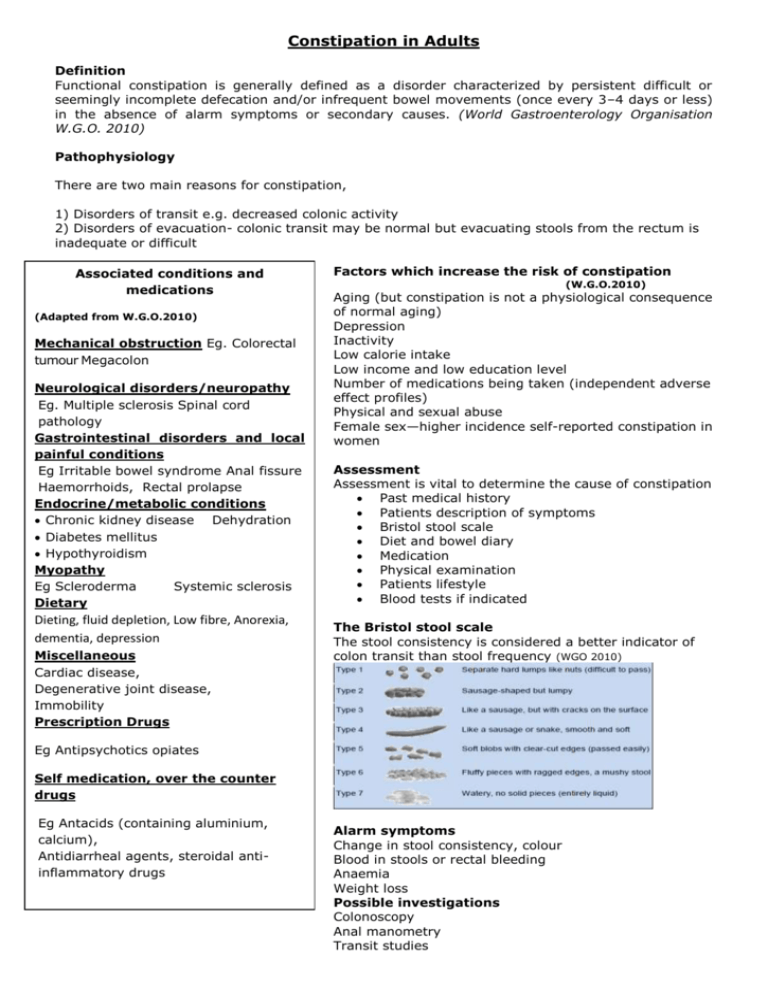
Constipation in Adults Definition Functional constipation is generally defined as a disorder characterized by persistent difficult or seemingly incomplete defecation and/or infrequent bowel movements (once every 3–4 days or less) in the absence of alarm symptoms or secondary causes. (World Gastroenterology Organisation W.G.O. 2010) Pathophysiology There are two main reasons for constipation, 1) Disorders of transit e.g. decreased colonic activity 2) Disorders of evacuation- colonic transit may be normal but evacuating stools from the rectum is inadequate or difficult Associated conditions and medications (Adapted from W.G.O.2010) Mechanical obstruction Eg. Colorectal tumour Megacolon Neurological disorders/neuropathy Eg. Multiple sclerosis Spinal cord pathology Gastrointestinal disorders and local painful conditions Eg Irritable bowel syndrome Anal fissure Haemorrhoids, Rectal prolapse Endocrine/metabolic conditions Chronic kidney disease Dehydration Diabetes mellitus Hypothyroidism Myopathy Eg Scleroderma Systemic sclerosis Dietary Dieting, fluid depletion, Low fibre, Anorexia, dementia, depression Miscellaneous Cardiac disease, Degenerative joint disease, Immobility Prescription Drugs Factors which increase the risk of constipation (W.G.O.2010) Aging (but constipation is not a physiological consequence of normal aging) Depression Inactivity Low calorie intake Low income and low education level Number of medications being taken (independent adverse effect profiles) Physical and sexual abuse Female sex—higher incidence self-reported constipation in women Assessment Assessment is vital to determine the cause of constipation Past medical history Patients description of symptoms Bristol stool scale Diet and bowel diary Medication Physical examination Patients lifestyle Blood tests if indicated The Bristol stool scale The stool consistency is considered a better indicator of colon transit than stool frequency (WGO 2010) Eg Antipsychotics opiates Self medication, over the counter drugs Eg Antacids (containing aluminium, calcium), Antidiarrheal agents, steroidal antiinflammatory drugs Alarm symptoms Change in stool consistency, colour Blood in stools or rectal bleeding Anaemia Weight loss Possible investigations Colonoscopy Anal manometry Transit studies Conservative management (once organic causes have been excluded) Dietary measures - a gradual increase in dietary fibre. Pre & probiotic drinks Note; A sudden switch can cause abdominal pain, increased flatulence and bowel urgency Irritable Bowel syndrome- Insoluble fibre is not recommended. Soluble fibre eg oats is recommended NICE 2008 Maintain an adequate fluid intake 6-8 glasses fluid per day Allow time to sit to toilet Behavioural advice Stop constipating medication if possible Biofeedback Adopt the correct seating position see trust leaflets; Dietary Fibre GHP10810-06-09 Improving bowel function and control GHP10810-096-09 Oral Medication Bulk forming laxatives Osmotics Stimulants Softeners Pro kinetics eg eg eg eg eg Psyllium methyl cellulose Polyethylene glycol, Lactulose Bisacodyl/sodium picosulfate Senna Dioctyl Prucalopride see NICE report 2010 http://www.nice.org.uk/nicemedia/live/13284/52078/52078.pdf Bulk forming laxatives are useful when dietary fibre is inadequate but should be avoided if fluid intake is poor . Osmotic laxatives are useful as they draw water into the gut softening the stool without increasing peristalsis. Softeners can be useful and are often used in conjunction with a stimulant Stimulants should not be used as a first line of treatment as they can cause abdominal cramping if the stool is hard, however are useful in neurological conditions such as multiple sclerosis with evacuation difficulties. Prokinetics normalise peristalsis and are recommended for women when other laxatives have failed and invasive methods are being considered (NICE 2010) Rectal Medication can be particularly useful with evacuation disorders. Eg Glycerine suppositories Rectal stimulation can be useful in spinal injury but should be used with caution in case of autonomic dysreflexia (AD) however this can also prevent AD Anal Irrigation Can be useful when constipation has not been resolved by conservative measures or medication. If you feel a patient would benefit from anal irrigation contact the continence service for advice Surgery when all measures have failed Only very few patients benefit from a (reversible) colostomy to treat constipation.(WGO 2010)