Chapter 13: The Spinal Cord, Spinal Nerves, and Spinal Reflexes

Chapter 13:
The Spinal Cord, Spinal Nerves, and Spinal Reflexes
1
General Organization of the Nervous System
• Highly organized, very efficient
2
Figure 13–1
Nervous System
• Organization:
– CNS = brain and spinal cord
– PNS = all other neural tissue
• Structures in the PNS
1. Ganglia = collection of somas together in one place
2. Nerves = bundles of axons
• Structures in the CNS:
1. Center = collection of somas with a common function
2. Nucleus = a center with a visible boundary
3. Neural cortex = gray matter (somas) covering the brains
4. Tracts = bundles of axons with common origins, destinations and function
5. Columns/funiculi = large tracts in the spinal cord
6. Pathways = centers and tracts that link brain with body
• Sensory pathways: receptor CNS
• Motor pathways: CNS effector
3
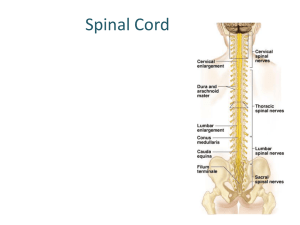
Gross Anatomy of the Spinal Cord
• 45cm (18”) from brain to L2
• Inside vertebral canal
– Stacked vertebral foramen
• Surrounded by CT:
– Spinal Meninges
• Support spinal cord
• Protect spinal cord
4
Figure 13-2
Spinal Meninges
Three Layers:
1. Dura Mater
2. Arachnoid
3. Pia Mater
Functions:
– protect spinal cord
– carry blood supply
All three layers are continuous with cranial meninges of the same name and the connective tissue around the spinal nerves.
5
Figure 13–3
Spinal Meninges
1.
Dura Mater: Outermost
Dense collagen fibers
Attaches to periosteum of occipital bone and coccyx by coccygeal ligament
Surrounded by the epidural space which contains blood vessels and adipose
2.
Arachnoid: Middle
Two layers
1.
Arachnoid membrane:
- Simple squamous epithelium, contacts dura mater
2.
Arachnoid tradeculae:
- Collagen and elastin fibers that bind to pia mater
- Fibers pass through the subarachoid space which contains cerebrospinal fluid
- CSF: for shock absorption and diffusion medium 6
Spinal Meninges
3. Pia Mater: Innermost
- Fine mesh of collagen and elastin fibers bound to neural tissue
- Attached to arachnoid trabeculae
- Has dentriculate ligaments that extend through arachnoid to dura mater to prevent lateral movement of the cord
7
Anatomy of the Spinal Cord
8
Figure 13–5a
Anatomy of the Spinal Cord
• Posterior median sulcus
– Posterior surface bears a shallow longitudinal groove
• Anterior median fissure
– Deeper groove along the anterior surface
• Central canal: contains CSF for diffusion
• Gray matter: somas, neuroglia, unmyelinated axons
– Posterior gray horn:
• somatic and visceral sensory nuclei
– Anterior gray horn:
• somatic motor nuclei
– Lateral gray horn:
• throacic and lumbar only, visceral motor nuclei (ANS)
– Gray commissure:
• axons for decussation (cross over to other side)
9
Anatomy of the Spinal Cord
• White Matter: myelinated axons
– Posterior white column/funiculus
– Anterior white column/funiculus
– Lateral white column/funiculus
– All 6 column contains tracts:
• Ascending tracts: sensory to brain
• Descending tracts: motor from brain
• Transverse tracts: decussation
• Axons exit as spinal roots (dorsal +ventral = spinal nerve)
– Dorsal root: sensory axons from receptor to CNS
– Dorsal root ganglion: somas of the sensory neurons
– Ventral root: motor axons from CNS to effectors 10
KEY CONCEPT
• Spinal cord has a narrow central canal
– surrounded by gray matter
– containing sensory and motor nuclei
• Sensory nuclei are dorsal
• Motor nuclei are ventral
• Gray matter:
– is covered by a thick layer of white matter
• White matter:
– consists of ascending and descending axons
– organized in columns
– containing axon bundles with specific functions
11
Anatomy of the Spinal Cord
• Spinal roots exit vertebral canal through intervertebral foramen
• Dorsal and ventral roots combine to form spinal nerve
12
Damage to which root of a spinal nerve would interfere with motor function?
1.
posterior root
2.
anterior root
3.
dorsal root
4.
ventral root
13
Where is the cerebrospinal fluid that surrounds the spinal cord located?
1.
epidural space
2.
subarachnoid space
3.
above the dura mater
4.
between the pia mater and the nervous tissue of the brain
14
Spinal Nerves
• 31 pairs
• Exit via intervertebral or sacral foramen
• Name for location of exit on spin beginning between skull and C1
• Nerves:
– C1-C8
– T1-T12
– L1-L5
– S1-S5
– Co1
15
Spinal Nerves
• Cord and column grow together until age 4
• Column continues to grow but cord does not
– Roots “stretch” to reach foramen
• Adult: cord ends at L1-L2
• “stretched” spinal roots after
L2
– cauda equina
• Lumbar puncture:
– “spinal tap” at L3-L4 draw CSF from subarachnoid space
16
Intervertebral foramen
Maintained by intervertebral
Discs between vertebrae
17
• Herniated disc:
– Nucleus pulposus ruptures through anulus fibrosis
– Compresses nerves in intervertebral foramen and/or spinal cord in vertebral canal
• Slipped disc:
– Intervertebral disc distorted or displaced
– Causes pressure
18
Nerve Structure
• Dorsal root + ventral root + blood vessels + connective tissue
1.
Epineurium
Outermost layer
Dense collagen fibers
2.
Perineurium
Partitions that extend inward from epineurium and divide axons into bundles called fascicles
3.
Endoneurium
Innermost layer
Thin collagen fibers that surround each axon
19
Figure 13–6
Nerve Structure
• Axons repair if cut , it will follow original path
• Severed nerves do not usually repair
– Axons do not line up correctly
• Spinal nerves branch off cord near to what they innervate
• Cervical and lumbar enlargements of cord house cell bodies of motor neurons for muscles of appendages
• Dermatome : Region of skin surface
– Innervate by one pair spinal nerves
20
Dermatomes
21
Figure 13–8
Nerve Plexus
• Most spinal nerves do not go directly to target:
– Axons from multiple nerves intermingle in a nerve plexus
22
Spinal Nerve Plexus
• Nerve plexus:
– Interwoven network of nerves
1. Cervical plexus:
– Nerves C1-C5
– Innervate muscles of neck and diaphragm
2. Brachial plexus:
– Nerve C5-T1
– Innervate pectoral girdle and upper limbs
3. Lumbar plexus:
– Nerves T12-L4
– Innervate pelvic girdle and lower limbs
4. Sacral plexus:
– Nerves L4-S4
– Innervate lower limbs
23
Trauma and Disorders
• Often result form damage or pressure
1. Paralysis:
– Loss of motor function
– Disorder of ventral root or anterior gray horn
2. Paresthesias:
– Sensory loss
– Disorder of dorsal root or posterior gray horn
– Complete transection results in loss of both motor and sensory below injury
3. Paraplegia:
– Sever between T1 and L4
– Loss of lower limb function
4. Quadriplegia:
– Sever in cervical
– Loss of all limb function (above C5 can kill)
24
Organization of Neural Pathways
• 10 million sensory neurons
– receptor to CNS
• 500 thousand motor neurons
– CNS to effector
• 20 billion interneurons
– coordinate sensory and motor, they are between sensory and motor neurons located in the CNS
• Interneurons organized into neuronal pools
– functional groups with limited input sources (sensory) and output locations (motor)
• Spread of info organized into neural circuits
25
5 Neural Circuits
26
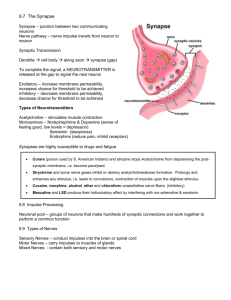
Reflexes
• Rapid, automatic nerve responses triggered by specific stimuli
• Used to maintain homeostasis
• Simple reflex:
– Sensory perception in, motor response out
• Simple reflexes can be grouped together for complex actions
• Reflex arc = single reflex
27
5 Steps in a Neural Reflex
28
Figure 13–14
5 Steps in a Neural Reflex
• Step 1: Stimulus Activates Receptor
– Receptor = specialized cell or dendrite of sensory neuron
– Receptor responds to a particular type of stimuli
• physical or chemical changes
• Step 2: Sensory Neuron is Activated
– Stimulation causes action potential on axon of sensory neuron
– Nerve impulse travels into spinal cord via dorsal root
29
5 Steps in a Neural Reflex
• Step 3: Information Processing
– Simple case: sensory neuron synapses on motor neuron
– More complex: sensory neuron synapses on an interneuron
– Sensory neuron causes EPSP which is integrated with other stimuli
• Step 4: Motor Neuron is Activated
– Motor neuron is stimulated to threshold
– Action potential travels down motor neuron axon to effector
• Step 5: Peripheral effector responds
– Neurotransmitters released by motor neuron trigger events in effector
– E.g. muscle contraction
30
Reflex Arcs
• Negative Feedback
– Action opposes stimulus as form of defense
– Fast response, but not always coordinated
31
Reflex Classification: 4 Ways to Classify
32
4 Classifications of Reflexes
1. By early development
2. By type of motor response
3. By complexity of neural circuit
4. By site of information processing
33
Response
• Nature of resulting motor response:
– somatic reflexes :
• involuntary control of nervous system
– superficial somatic reflexes
» Stimuli originate at skin or mucous membranes
– stretch reflexes (deep tendon reflexes)
» Stimuli from overstretched tendon
» e.g., patellar reflex
– visceral reflexes (autonomic reflexes):
• control systems other than muscular system
34
Complexity
• Complexity of neural circuit:
– monosynaptic reflex :
• sensory neuron synapses directly onto motor neuron
– polysynaptic reflex :
• at least 1 interneuron between sensory neuron and motor neuron
• Response delayed by each synapse but capable of more complex output
35
Examples of Common Spinal Reflexes
1. Patellar Reflex
2. Withdrawal Reflex
36
1. Patellar Reflex
• Monosynaptic stretch reflex
• Carried on type A fibers: largest myelinated axons
– Carries action potential at the fastest rate
• Sudden stretch of patellar ligament activates muscle spindle signal quadriceps group to contract
37
Figure 13–15
Stretch Reflex
• Muscle spindles = sensory receptors involved in the stretch reflex
– Consist of a bundle of small, specialized skeletal muscle fibers called intrafusal muscle fibers
• Innervated by sensory and motor neurons
– Surrounded by a larger extrafusal muscle fiber responsible for
• The resting muscle tone
• The contraction of the entire muscle, when greater levels of stimulation are present
38
A Muscle Spindle
Axons of motor neurons innervating intrafusal fibers
39
Figure 13–16
Muscle Spindle:
Specialized Muscle Fiber
• Constantly signal CNS
• Relaxed = signal less
• Stretched = signal more
– threshold, trigger reflex arc
• Prevent overstretching of muscle and tendons
• Aid in maintaining upright position
40
2. Withdrawal Reflexes
• Complex polysynaptic spinal reflex
• Consists of three parts:
1. Flexor reflex: flex to withdraw
2. Reciprocal Inhibition: inhibit extensors
3. Crossed extensor reflex: maintain balance
41
Withdrawal Reflexes
• Pain flexor muscles pull limb away
extensors same limb inhibited to prevent opposition to flexion
limbs on opposite side extend to provide balance for sudden flexion
42
A Flexor Reflex
43
Figure 13–17
44
Reflexes
• Reflexes automatic but can be impacted by higher brain centers:
– Fine tune or combine reflexes
– Take cues from reflex for coordinated voluntary movements
– Facilitate or inhibit reflexes
• Reflexes serve as diagnostic tool to assess health and function of spinal cord and brain
45
Integration and Control of Spinal Reflexes
• Though reflex behaviors are automatic:
– processing centers in brain can facilitate or inhibit reflex motor patterns based in spinal cord
46
Voluntary Movements and
Reflex Motor Patterns
• Higher centers of brain incorporate lower, reflexive motor patterns
• Automatic reflexes:
– can be activated by brain as needed
– use few nerve impulses to control complex motor functions
– walking, running, jumping
47
KEY CONCEPT
• Reflexes :
– rapid, automatic responses to stimuli
– “buy time” to plan and execute complex, conscious responses
• Somatic motor reflexes :
– fastest reflexes
– involve myelinated axons
– involve only 1 spinal cord segment or brain nucleus
– are monosynaptic
48
SUMMARY
• General organization of nervous system:
– CNS, PNS
• Afferent (sensory) and efferent (motor) fibers
• Structures and functions of spinal meninges
• Gray matter and horns of spinal cord
• 4 major nerve plexuses:
– cervical, brachial, lumbar, sacral
• Neuronal pools and neural circuit patterns:
– divergence, convergence, serial, parallel, reverberation
49
SUMMARY
• Reflexes and reflex arcs
• Classifications of reflexes:
– innate vs. acquired
– somatic vs. visceral
– cranial vs. spinal
– monosynaptic, polysynaptic, or intersegmental
• Characteristics of monosynaptic reflexes:
– stretch reflex, postural reflex, muscle spindles
• Characteristics of polysynaptic reflexes:
– tendon, withdrawal, flexor, and crossed extensor reflexes
50