15 Renal - bloodhounds Incorporated
advertisement

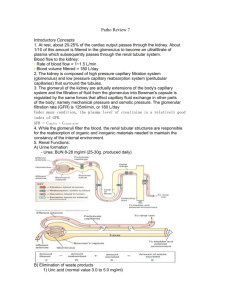
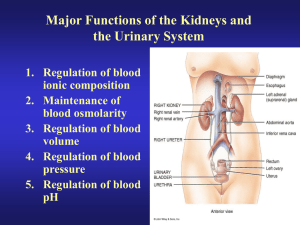
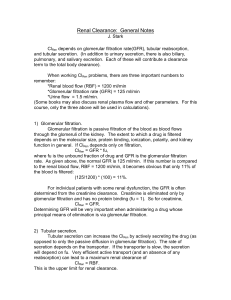
The Renal System Five Processes of Urinary System 1. 2. 3. 4. 5. Filtration, Reabsorption, Secretion, Excretion Micturition 180 L / day filtered, >99% reabsorbed, 1.5 L/day excreted 1) Filtration Movement of fluid from blood to lumen of nephron 1) Filtration: Passage across 3 Barriers 1. Capillary endothelium is fenestrated 2. 3. Basal lamina 1. Filters proteins 2. Negative Charges Bowman’s capsule epithelium (visceral layer), including podocytes Cause of Filtration Three types of pressures are at work: Hydrostatic pressure in capillaries (see exchange in tissues) Osm. Pcapillaries > Osm. P Bowman’s capsule Hydrostatic fluid P from presence of fluid in Bowman’s capsule Net driving pressure: ~ 10 mmHg 2) Tubular Reabsorption (99% of filtrate) Mostly transepithelial transport (examples: Sodium and glucose) Reabsorption may be active (Na+, glucose) or passive (urea) 2) Tubular Reabsorption (99% of filtrate) Active Transport Na+ /K+ ATPase pumps Passive concentration and osmotic gradients Na+ Reabsorption in PCT Apical: Na+ movement down conc. gradient. Basolateral: Na+/K+ ATPase. Na+ Linked Glucose Reabsorption Basolateral: Apical: Na+-glucose cotransport Glucose diffusion down conc. gradient Saturation of Renal Transport Saturation = Maximum rate of transport (tm) Same 3 characteristics as discussed in mediated transport Transport maximum determined by Saturation Renal Threshold Specificity Competition Clinical Importance of GFR and Clearance GFR is indicator for overall kidney function Clearance → non-invasive way to measure GFR Inulin (research use) Neither secreted nor reabsorbed Creatinine (clinically useful) If a substance is filtered and reabsorbed but not secreted clearance rate < GFR If a substance is filtered and secreted but not reabsorbed clearance rate > GFR Regulation of Blood Pressure via Tubuloglomerular Feedback Decrease blood pressure in afferent arteriole juxtaglomerular cells release Renin Renin Angiotensinogen Angiotensin I ACE Angiotensin I Angiotensin II Aldosterone/ ADH secretion 3) Secretion 2nd route of entry (from ECF) into tubules for selected molecules Mostly transepithelial transport (analogous to reabsorption). Depends mostly on active membrane transport systems Provides mechanism for rapid removal of substances (most important for H+, K+, foreign organic ions and drugs such as penicillin etc.) 4) Excretion = Urine Output Excretion of excess ions, H2O, toxins, “foreign molecules” “nitrogenous waste” (NH4+ , urea) Depends on Filtration, Reabsorption, Secretion E=F–R+S Direct measurement of F, R, S impossible infer from comparison of blood & urinalysis For any substance: (Renal) Clearance = plasma volume completely cleared of that substance per minute Typically expressed as ml/min 5. Micturition Spinal cord integration: 2 simultaneous efferent signals In infant just simple spinal reflex Later: learned reflex under conscious control from higher brain centers Various subconscious factors affect reflex Fig 19-18 Manneken Pis in Brussels GFR = Glomerular Filtration Rate Describes filtration efficiency: Amount of fluid filtered per unit of time Average GFR ~ 180 L/day! Filtration Coefficient is influenced by Net filtration pressure Available surface area of glomerular capillaries GFR is closely regulated to remain constant over range of BPs (80 - 180 mm Hg) Goal is to control blood flow though both afferent and efferent arterioles – via ? Regulation of GFR Several mechanisms provide close control of GFR; Filtration Pressure (BP) Tubuloglomerular feedback Hydrostatic, colloid Resistance in afferent vs. efferent arterioles JG Apparatus Hormones and ANS Angiotensin II (vasoconstrictor) Prostaglandins (vasodilator) Passive Urea Reabsorption Na+ actively reabsorbed H2O follows passively [urea] passive reabsorption (diffusion into blood) An increase in afferent arteriolar pressure will result in all of the following except A. B. C. D. An increase in GFR An increase in glomerular hydrostatic pressure An increase in the osmotic pressure of the glomerular capillaries A somewhat greater output of urine Urine flows to the urinary bladder from the kidney by means of the A. B. C. D. E. Urethra Proximal tubule Peritubular capillary Ureter Prostate The fluid that enters the glomerulus is essentially similar to A. B. C. D. E. Serum Blood Sea water Fresh water Plasma The driving force that pushes fluid from the blood into Bowman’s capsule is exerted A. B. C. D. E. By the heart By the muscles lining the abdominal cavity By the urinary bladder By the urethra Gravity The rate of reabsorption of water from the collecting duct is determined by the hormone A. B. C. D. E. Oxytocin Cortisone Antidiuretic hormone Lactogenic hormone Aldosterone If the Tm for a particular amino acid is 120 mg/100 ml and the concentration of that amino acid in the blood is 230 mg/100 ml, the amino acid A. B. C. D. Will be actively secreted into the filtrate Will be completely reabsorbed the tubule cells Will appear in the urine Only a and c Which of the following is not reabsorbed by the proximal convoluted tubule? A. B. C. D. E. Na+ K+ Glucose Creatinine Water Alcohol acts as a diuretic because it A. B. C. D. Is not reabsorbed by the tubule cells Increases the rate of glomerular filtration Blocks the activity of ADH Increases the secretion of Aldosterone The kidneys are stimulated to produce renin A. B. C. D. When the peritubular capillaries are dilated When the pH of the urine decreases By a decrease in the blood pressure When the specific gravity of urine rises above 1.10 The descending limb of the loop of Henle A. B. C. D. Is not permeable to water Is freely permeable to sodium and urea Contains fluid becoming more concentrated as it moves down into the medulla Pulls water by osmosis into the lumen of the tubule Renal Failure & Artificial Kidney Symptoms when < 25% functional nephrons due to: 1. Kidney infections 2. Chemical poisoning (lead, paintthinner) etc. Hemodialysis: 3/week 4-8h/session Alternative: CAPD Continuous Ambulatory Peritoneal Dialysis