Renal problem set
Bio 370
Fall 2005
Dr. Janet Daniel
Practice problems for Renal Physiology
Also include end of chapter 14 exercises: Quantitative exercises 1-4.
1.
Fully describe the anatomy of your “filter”. a.
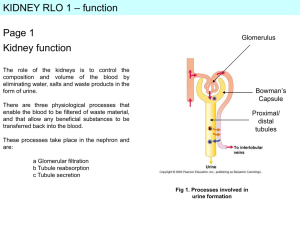
What is the Bowman’s Capsule; is it part of the Nephron?
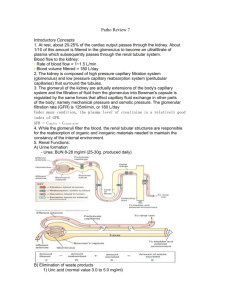
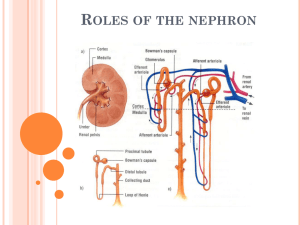
ANSWER: Bowman’s capsule” an expanded, double walled invagination of the kidney tubule (nephron) that cups around the glomerulus to collect the fluid filtered from the glomerular capillaries. b.
What are Podocytes, and what is their role in filtration? If the filter is selective, what does it select for? How selective is it?
ANSWER: Podocytes are octopuslike cells that encircle the glomerular tuft. The podocytes interdigitate (weave like fingers) to form slits of varying sizes into the lumen of the Bowman’s capsule. They form the lumen of the Bowman’s capsule. Size selection and can vary depending on the size of the slits. c.
What is the driving force for filtrate formation?
ANSWER: Three physical forces contribute to the pressure gradient from the capillaries to the lumen of the Bowman’s capsule: Glomerular capillary blood pressure, plasmacolloid osmotic pressure, and Bowman’s capsule hydrostatic pressure. All are considered in the calculation of the net filtration pressure (which is the driving force for filtration)
2.
What is the Juxtaglomerular Assembly (JGA) and where is the JGA located? a.
What parts of the Nephron are “joined” in the JGA?
ANSWER: See figure 14-23.
3.
What is the chemical composition of the primary filtrate vs. final product emerging from the kidney?
ANSWER: The filtrate resembles plasma in osmolarity, but is devoid of proteins. Final product is urine, devoid of most solutes. Note that composition of urine with respect to H
2
0 and secreted substances, primarily K
+
, and H
+
. can vary.
4.
Compare the recovery / reabsorption of the following in the (1) proximal tubule, (2) distal tubule, (3) loop of Henle, (4) collecting duct: a.
H
2
O
ANSWER: 1) passively with solutes, 2) occurs only with vasopressin, 3) descending loop only 4) occurs only with vasopressin b.
Amino Acids
ANSWER: 1) Secondary active transport using Na/amino acid transporter, 2) none
3) none, 4) none
c.
HCO
3
-
ANSWER: “reabsorbtion” is coordinated with H+ secretion. d.
Glucose
ANSWER: 1) reabsorption by secondary active transport 2) none 3)none 4) none. e.
PO
4
-
ANSWER: 1) reabsorption (can be increased with parathyroid hormone) 2)none 3) none
4) none.
5.
Propose cellular / molecular schemes for the movement of the following molecules from
Nephron lumen to interstitial fluids: a.
Glucose across the cells of the proximal tubule.
ANSWER: Sodium glucose cotransporter in the apical membrane and facilitative glucose transporter in the basolateral of the renal proximal tubule cells. b.
Na
+
across the cells of the thick ascending duct of the Loop of Henle
ANSWER: Na+, K+, Cl- across the apical membrane using the Na+/K+/Cl- channel, and Na+ across the basolateral membrane via the Na/K ATPase c.
H
2
O in the collecting duct.
ANSWER: vasopressin mediated increase of water permeability in the duct. This is caused by activation of the secondary messenger system involving cAMP which leads to the insertion of water channels (aquaporins) in the apical membrane.
6.
Describe the events that occur in the Loop of Henle and the Collecting Duct that establish the osmotic gradient within the Renal Pyramid.
HINT: The cells of the Loop of Henle have different properties. How might the cells of one region differ than cells of the other region with respect to H
2
O permeability and Na + permeability?
7.
Draw a curve that shows how tubular transport (i.e. reabsorption) using a carrier-mediated mechanism varies with plasma concentration.
Transport
Concentration of substance
NOTE: This is a curve of transport of a substance that is mediated by a transporter protein in the membrane. Shows classic saturation kinetics and can be described by
Michaelis-Menten kinetics. My point in doing this is to promote the understanding that reabsorption of most solutes in the proximal tubule is mediated by a protein carrier and that it can be saturated (as evidenced by the tubular maximum) and that at the point of saturation the rest of the solute is “spilled” into the urine.
8.
A creatinine clearance test is performed on an 80-kg man. The following results are obtained:
[Creatinine (Cr)] plasma
= 3.5 mg/dl
24-hour urine volume = 800ml
[Cr] urine
=125 mg/dl a.
Calculate the creatinine clearance.
ANSWER: first need to convert mg/dl to mg/ml
1dl to L = 1dl * .1 = .1L
L to ml = .1L * 1000 = 100 ml to convert to 1 ml move decimal point two places to left on mg
.035 mg/ml and 1.25 mg/ml second need to convert 800 ml/ 24 hours to ml/min
800/24 = 33.33ml/hr 33.33/60min = 0.55ml/min equation: Ccr (Creatine clearance) = [Cr] urine
* V/ [Cr] plasma
CCr = (1.25mg/ml * .55 ml/min)/.035 mg/ml
CCr = 19.64 ml/min b. Is this an accurate estimate of the GFR? Why or why not?
ANSWER: This is not 100% accurate as a small amount of creatinine is also secreted
9. Use the following data to answer the questions a through d below (make sure you give the units throughout):
Plasma inulin concentration = 0.01 mg/ml
Urine inulin concentration = 1.00 mg/ml
Urine flow rate = 1.20 ml/min
Plasma concentration of solute x = 0.05 mg/ml
Urine concentration of solute x = 2.00 mg/ml
Plasma PAH concentration = 0.001 mg/ml
Urine PAH concentration = 0.390 mg/ml
Hematocrit = 0.50
Calculate: a. What is the GFR?
ANSWER: GFR= Cinulin = ([inulin] urine
*V)/[inulin] plasma
= (1.20 ml/min)(1.00 mg/ml)/0.01 mg/ml = 120 ml/min
b.
Show whether there is net reabsorption or net secretion (or neither) of solute x.
ANSWER: For net secretion: Cx > GFR
For net reabsorption: Cx < GFR
Cx = [X] urine
V/[X] plasma
= (1.20 ml/min)(2.00 mg/ml)/ 0.05 mg/ml = 48 ml/min
= NET REABSORPTION c. What is the Filtration fraction?
ANSWER: Filtration fraction = GFR/RPF
RPF = Cpah/0.91 = UpahV/Ppah(0.91) = 514.3 ml/min
Filtration Fraction = 120 ml/min / 514.3 ml/min = 2.3% d. What is the renal blood flow?
RBF = RPF / (1- hematocrit)
= (514.3 ml/min) / (1 - 0.5)
= 1028.6 ml/min