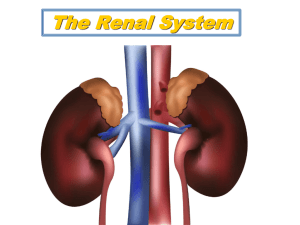
Renal Physiology 2 Basic Renal Processing Steps in urine formation
advertisement

artery Afferent arteriole Glomerular capillary Efferent arteriole Renal Physiology 2 Office hours/help after lecture Peritubular capillary Bowman’s space vein tubule Basic Renal Processing Steps in urine formation • General strategy – Everything but cells and protein gets filtered into Bowman’s space (called glomerular filtrate) – Flitrate has the same substances at same concentrations as plasma – Further along tubule, substances are added (secretion) or removed (reabsorption) 1 1. Filtration 2. Secretion 3. Reabsorption 4. Excretion (urine) 2 3 4 1 Amount excreted = amount filtered + amount secreted – amount reabsorbed 1. Filtered and secreted; not reabsorbed 3. Filtered and completely reabsorbed 2. Filtered and some reabsorbed Glomerular Filtration • For each substance in plasma there is some combination of filtration, reabsorption and secretion • For many substances (eg, Na+, Ca++, water) these processes are under physiological control 2 Capillary Fenestra allow movement from plasma to Bowman’s space Glomerular Filtration • A bulk flow process πGC PGC PBs • Glomerular Filtration Pressure • πBS Glomerular Filtration Rate (GFR) – Function of: GFP= ((PGC-PBS)-(πGC- πBS)) 1. Filtration pressure 2. Permeability of substance – GFR = filtration pressure x Kf Usually 0 GFP=(60-15)-(29) = 16 mmHg • • Kf is the filtration coefficient 70 kg person – GFR water = 180 L/day (125 ml/min) Positive pressure indicates filtration 3 Role of hydrostatic pressure in controlling GFP 1. PBC – primarily a function of the tubules & ureters; movement of fluid through the system keeps PBC low 2. PGC – a function of blood volume in glomerular capillary – – – – – Afferent and efferent arterioles may be regulated independently Function of Reff / Raff Constriction of afferent ↓flow into glomerular capillary therefore ↓ PGC Constriction of efferent ↓ flow out of glomerular capillary therefore ↑ PGC Opposites for dilation Assessing kidney function by measuring plasma clearance & GFR To estimate plasma clearance Total entering= [plasma] x renal blood flow plasma clearancesubstance X = [urine]substance x urine vol [plasma]substance Amount filtered = [plasma] x GFR If substance is completely filtered and not reabsorbed nor secreted plasma clearance = GFR Amount in urine = [urine] x urine volume 4 Inulin is a small sugar that is completely filtered and is not reabsorbed or secreted 1. Inject a small amount of inulin into blood and measure [inulin]plasma 2. Measure [inulin]urine and urine volume Inulin excretion = 0.1 L/h x 300 mg/L = 30 mg/h Plasma clearanceinulin = [inulin]plasma= 4mg/L Urine volume = 0.1 L/hour [inulin]urine = 300 mg/L 300 x 0.1 4 Plasma clearanceinulin = 7.5 L/h = GFR Steps in urine formation For any substance: • If plasma clearance <GFR there must be reabsorption • If plasma clearance >GFR there must be secretion 1 1. Filtration 2. Secretion 3. Reabsorption 4. Excretion (urine) 2 3 4 5 Distal tubule Tubular Reabsorption 180 L of glomerular filtrate, only 1 L of urine →99% of all water is reabsorbed 1800g/day of NaCl in glomerular filtrate, only 10g/day in urine → 99% of NaCl is reabsorbed Glucose → 100% reabsorption Collecting duct Proximal tubule Descending LofH Ascending LofH - thick Ascending LofH - thin paracellular capillary Tubular fluid transcellular Tight junction Na+ Na+ K+ ATP K+ ATP Na+ 6 • Na+,K+ pump establishes Na+ gradient • In the proximal tubule Na+ transport • Water movement is secondary to Na+ transport – Antiport with H+ – Symport with glucose Na+ 1. Na+ K+ 2a. ↓osmolarity Na+ Na+ H+ Na+ glucose K+ ATP ATP 2b. ↑osmolarity H2O H2O 3. osmosis 4. Bulk flow glucose • Na+,K+ pump establishes Na+ gradient • In the distal tubule Na+ transport – Symport with Cl- Na+ Na+ ClK+ ATP H20 Na+ Proximal tubule High Active transport Descending LofH High Low Ascending LofH Low Active transport Distal Tubule & Collecting Duct Variable Active transport due to hormones 7 Formation of urine Excretion of dilute urine occurs with low levels of ADH/vasopressin 100 300 1. Dilute 2. Concentrated 300 150 300 80 H2O 375 375 400 Active transport of solutes 350 H2O 500 700 500 700 65 Low permeability to water • To form dilute urine: – Reabsorb solute from tubular fluid, while leaving water in the distal tubules. – Occurs only in the absence of ADH/vasopressin 8