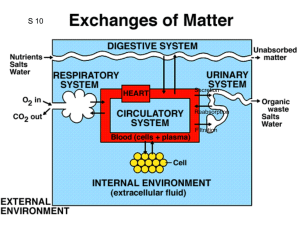
Regulation of kidneys work. Role of kidneys in homeostasis
advertisement

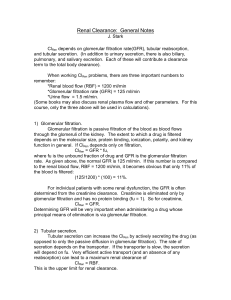
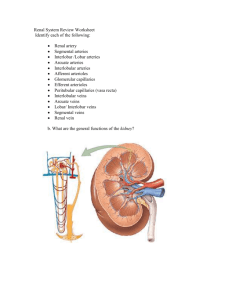
Regulation of kidneys work. Role of kidneys in homeostasis maintenance. Balancing role of the kidney • Water balance • Sodium / potassium / chloride intake and excretion balanced • Average daily requirements: • Water : 25 - 35 ml/kg/day • Sodium : 1 - 1.4 mmol/kg/day • Potassium: 0.7 - 0.9 mmol/kg/day • Chloride : 1.3 - 1.9 mmol/kg/day Urine formation results from Glomerular filtration, Tubular reabsorption, and Tubular secretion Filtration only GFR = C in Filtration, reabsorption Filtration, secretion C sub. ˂ C in. C sub. in. Urine Urine ˃C Urine Urinary excretion rate = Filtration rate – Reabsorption rate + Secretion rate Glomerular Filtration Rate - Determinants This is simplification of Starlings principle for movement across capillaries Net Filtration = Kf NFP Kf is Filtration co-efficient Incorporates surface area membrane permeability NFP= Net filtration pressure in mmHg: NFP = Glomerular capillary hydrostatic pressure – Bowman’s capsule hydrostatic pressure – Glomerular capillary oncotic pressure Glomerular filtration rate (GFR) Kf affected by: – Mesangial cell contraction ↓ area – Causes - angiotensin II - ADH - bradykinin – Membrane permeability relatively constant Think about the effects of each of the determinants of net filtration pressure – GCHP e.g: if afferent arteriole constriction, efferent arteriole dilatation, GCHP falls. This leads to a fall in GFR BCHP e.g: ureteric obstruction causes ↑BCHP and ↓GFR GCOP e.g: fluid overload with low oncotic pressure - ↑GFR Net Filtration Pressure along glomerulus Drop along capillary due to Decreased glomerular capillary hydrostatic pressure Increased glomerular capillary oncotic pressure Glomerular capillary NFP: NFP = GCHP – BCHP – GCOP Numbers: Afferent end: 24 = 60 - 15 – 21 Efferent end: 10 = 58 – 15 - 33 Factors affecting GFR - summary 1. Mean Hydrostatic driving force (pressure in GC-BC) 2. Kf (filtration coefficient) 3. Oncotic pressure gradient Measuring GFR Ideal is CLEARANCE of a substance that is freely filtered by the glomerulus but not secreted or reabsorbed. Also not stored, metabolised in kidney, not toxic, does not alter GFR and easy to measure. INULIN is gold standard Would need constant infusion to maintain a constant plasma concentration Creatinine – not ideal – formed by muscle, released at reasonably constant rate, BUT – overestimates GFR by approx 10% due to SECRETION in tubules Plasma Clearance Plasma clearance is defined as the amount of plasma that is cleared or “cleansed” of a particular substance in one minute. The kidneys will carry out this clearance process through the use of filtration, reabsorption and secretion Filtration will directly affect clearance. As filtration increases, more material will be removed from the blood plasma. Reabsorption will indirectly affect clearance. As reabsorption increases, less material will be removed from the blood plasma. Secretion will directly affect clearance. As secretion increases, more material will be removed from blood plasma. Plasma Clearance The formula used to calculate plasma clearance is: C = V x U/P C = plasma clearance rate in ml/min V = urine production rate in ml/min U = the concentration of a substance in the urine in mg/ml P = the concentration of a substance in the plasma in mg/ml As you track the units in the equation, you will notice that mg/ml cancel out, leaving ml/min. Let us practice calculating plasma clearance using the clearance equation. In all your calculations, assume that the urine production rate (V) is 2 ml/min. Let’s start with the substance inulin (not insulin!). If after a dose of inulin, your urine has 30 mg/ml and your plasma has 0.5 mg/ml of this substance, what is the inulin clearance rate? If you got 120ml/min, you are correct! 120 ml/min = 2 ml/min x 30 mg/ml/ 0.5 mg/ml Renal Blood Flow (RBF) Very high – 20% cardiac output at rest, (1200ml blood/min or 600ml of plasma/min). Kidneys <1% body wt Tightly autoregulated (similar to heart, brain) Why the high blood flow: High O2 consumption – 6ml/100g/min (C/W heart 8-10, Brain 3.5) Second highest behind heart (per gram tissue) Most blood flow and O2 consumption goes to cortex Oxygen extraction quite low – 1.5vol% c/w 5vol% for body as whole Related mainly to active Na+ reabsorption and H+ ATPase pumps. Linked to GFR. (↑ GFR ↑02 consumption.) Regulation of RBF SYSTEMIC and LOCAL (=autoregulation) SYSTEMIC effects blood flow to more than just kidneys Neural – sympathetic/noradrenergic Vasoconstriction – ↓ RBF. Small ↓ GFR (partially offset by increased oncotic pressure in glomerular capillaries) Increased renin secretion (direct effect on 1 receptors). Causes angiotensin II release Afferent and efferent V/C and also action on mesangial cells ↓ GFR (but ↓ RBF more so filtration fraction increases) Increased sensitivity of juxtaglomerular cells Humoral Noradrenaline – V/C Prostaglandins – PGI2, PGE2. Cause renal arteriole V/D Renin (as per prev page) Other – e.g. exercise, diet Renin – Angiotensin system Autoregulation of RBF • MYOGENIC and METABOLIC components • Metabolic component here is tubuloglomerular feedback, that also regulates GFR • RBF relatively constant between approx MBP 75 and 170 mmHG Reabsorption of sodium Mechanisms of reabsorption