Human parasitology
advertisement

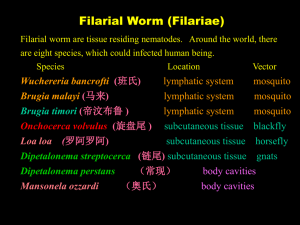
Filariae Filariasis is one of the five major parasitic disease in China and also one of the six major tropical diseases to which WHO devotes much attention (malaria, shistosomiasis, filariasis, leishmaniasis, trypanosomiasis) . Wuchereria bancrofti and Brugia malayi are found in China. Eight Species of Filariae Parasitizing Humans _____________________________________________________________________________ Species Site of inhabitation Vector Pathogenesis Distribution _______________________________________________________________________ W. bancrofti lymphatic tissues mosquito lymphatic damage worldwide ____________________________________________________________________ Brugia malayi lymphatic tissues mosquito lymphatic damage Asian _______________________________________________________________________ Brugia timori lymphatic tissues mosquito lymphatic damage Island of timor ____________________________________________________________________ Onchocerca subcutaneous; eye black fly蚋 river blindness Africa volvulus _______________________________________________________________________ Loa loa subcutaneous deer fly斑虻 skin swellings Africa _______________________________________________________________________ Dipetalonema subcutaneous midge库蠓 indefinite Africa streptocerca _______________________________________________________________________ Dipetalonema thoracic and midge库蠓 indefinite Middle and perstans abdominal cavities South America _______________________________________________________________________ Mansonella peritoneal cavity midge库蠓 indefinite South America ozzardi _______________________________________________________________________ I. Morphology 1. The adults are white and thread-like worms. The female is about 5-10 cm and the male 2.5-4 cm. 2. The microfilaria ranges from 177-296µm in length. They are encased in a sheath. number of body nuclei A large are seen in the stained specimen. A nerve ring with no nuclei can be seen at the anterior 1/5 of the body. The morphological differences between bancroftian and malayan microfilariae are the following: Adult worm of filaria Morphological Differences of Microfilariae between W. bancroti and B. malayi ________________________________________________________________ Species W. bancrofti B. malayi ________________________________________________________________ Appearance graceful, sweeping curves irregular, stiff curves ________________________________________________________________ Size larger 244-296× 7 µm smaller 177-230 × 6 µm ________________________________________________________________ Cephalic space shorter(1:1 or1:2) longer(2:1) (length:width) ________________________________________________________________ Nuclei body nuclei equal sized, clearly unequal sized, coalescing, defined, countable uncountable ________________________________________________________________ Terminal nuclei no two ________________________________________________________________ Microfilaria of W. bancrofti and B. malayi Microfilaria of W. bancrofti Anterior part and posterior part of bancroftian microfilaria Microfilaria of W. bancrofti showing it’s appearance Bancroftian microfilaria:body nuclei equal sized, clearly, defined, countable without caudal nucleus Microfilaria of W. bancrofti Microfilaria of B. malayi: the body nuclei is unequal sized, coalescing,uncountable. The cephalic space is longer with two caudal nuclei. Microfilaria of B. malayi II. Life Cycle: 1.Biohelminth: intermediate hosts(vector) are mosquitoes, bancroftian filaria is transmitted by Culex pipiens pallens in which the larval development takes 10-14 days, the development of malayan filaria in Anopheles sinensis requires 6-6.5 days; 2. Infective stage: filariform larva(L3); 3. Infective route: by skin( the wound bitten by mosquito ); 4. Site of inhabitation: lymphatic tissue; 5. Life span: 4-10 years; 6. Microfilariae may survive 1-3 months; 7. Viviparous; 8. Nocturnal periodicity: The microfilariae present in the peripheral blood during daytime is very low in density. The number of microfilariae gradually increase from evening to midnight. Proboscis of a mosquito containing filariform larvae A large number of 3rd stage larvae of a filarial sp emerging from the proboscis of a mosquito. III. Clinical manifestation 1. Acute stage: The symptoms are due to allergic reaction. It begins with a chill followed by a high fever. It is called filarial fever. The lymphangitis(淋巴管 炎 ) , lymphadenitis( 淋 巴 结 炎 ) may occur, orchitis ( 睾 丸 炎 ) and inflammation of spermatic cord are only found in infection of W. bancrofti. 2. Chronic stage: The manifestations are caused by lymphatic lesion. (1) Elephantiasis: Lymph edema may occur in the limbs, scrotum, breast, vulva and etc. (2) Chyluria only caused by W. bancrofti. (3) Hydrocele is only found in infection of W. bancrofti. A patient of elephantiasis Elephantiasis of leg due to filariasis Elephantiasis due to Brugia malayi. Pitting does not occur in this stage (solid edema) Elephantiasis due to Brugia malayi, complicated by severe dermatitis and secondary bacterial infection This lady has elephantiasis of the right leg and edema in the left Hydrocele is only found in infection of W. bancrofti. elephantiasis of the left leg and scrotum IV. Diagnosis The diagnosis depends on the symptoms, signs and history of living in endemic areas, but the confirmative diagnosis depends on the demonstration of microfilariae. 1. First choice method is thick blood smear, taking blood at night from 9pm-2am. 2. Millipore membrane filtration is used for screening the patients or checking curative effect in the endemic areas with the low infective rate. 3. Fresh blood smear used for mass education. 4. Immunological tests are only made reference of the diagnosis. V. Treatment and Prevention Elimination the source of infection and control mosquitoes. 1. First choice drug is diethylcarbamazine ( DEC, Hetrazan ). 2. DEC table salt (3:1000 ) are sold in endemic areas. People take this salt over 6 months, resulting in an elimination or great reduction of microfilariae in the blood stream, for treating and preventing filariasis. 3. Remove the giant elephantiasis of the scrotum, chest and limbs. 4. Eradicate mosquito breeding place and control mosquitoes.It is important to protect people from mosquito biting for controlling filariasis. VI. Epidemiology 1. Source of infection: The people harbor microfilariae in the blood stream. 2. Vector: Culex pipiens pallens, C. fatigans for W. bancrofti, Anopheles sinensis, Anopheles anthropophagus transmitting B. malayi. 3. Distribution: Filariasis of W. bancrofti is world-wide distribution, while filariasis of B. malayi is in Asia. In China, W. bancrofti distributes in south of Yellow River 16 provinces and city, while B. malayi in south of Yellow River 13 provinces and city. B. malayi is not in Shandong, Hainan and Taiwan. 4. Reservoir host: W. bancrofti is no reservoir host, while cat, monkey may be the reservoir host of B. malayi. Trichinella spiralis T.spiralis is the smallest human nematode and a biohelminth. The adults and juveniles (larvae) live in the same host, but they have to change a host to complete their life cycle.They cause trichinosis, a zoonosis, which is spread by mammals kill each other. Human infections result from eating raw meat. I. Morphology ♂1.5mm, ♀3-4mm, both have a single set of reproductive organs and stichocytes surrounding the esophagus. The secretions of stichocytes are relative to digestion and pathogenesis. 2. Juvenile: 124×6 µm, one or more coil in a cyst in the skeletal muscle fibers. The cyst is about 0.25-0.5 ×0.21-0.42mm in size. This is infective stage. There are stichocytes around the esophagus. 1. Adults: Trichinella spiralis encysted larva T. spralis – posterior end, male & female II. Life cycle 1. Infective stage: juveniles in cyst 2. Site of inhabitation: adults in small intestine(mainly in duodenum and jejunum), juveniles in skeletal muscles 3. Route of infection: by mouth 4. Life span of female: 1-2 months 5. Final host and intermediate host: person 6. Reservoir host: pigs, cats, dogs, mice etc swallowed by man Juveniles in raw meat duodenum digestive juice cysts rupture penetrate mucosa, develop and molt Larvae Mate free from the cysts die return to intestinal lumen ♂burrow into mucosa give birth to ♀ Liver R.H lungs L. H juveniles ♂adults ♀ portal vein skeletal muscle cells III. Clinical manifestation The process of the pathogenesis may be divided into 3 stages: 1. Invading stage(about 1 week): The damage is mainly found in the intestine. In this stage, abdominal pain, nausea,vomiting,diarrhea and fever may occur. 2. Migrating stage of the juveniles(2-3weeks):The damage is mainly in the skeletal muscles. In this stage, muscular pain with high fever is main symptoms, especially in active muscles. Wandering juveniles may also cause pneumonitis, pleurisy, encephalitis, nephritis and myocarditis etc. 3. Encysted stage(4-16 weeks): In this stage, only muscular pain present without other symptoms. IV. Diagnosis 1. Muscular biopsy; 2. Examination of left food and xenodiagnosis; 3.Immunodiagnosis:(1) CPT(circumlarval precipitin test) (2) ELISA (3) IHA V. Treatment: Albendazole and Mebendazole VI. Epidemiology: Worldwide distribution. Lots of mammals can serve as reservoir hosts. The spread of trichinosis is due to mammals killing each other. Humans get the infection by eating raw meat. VII. Prevention 1. Quarantine of meat; 2. Avoid eating raw meat and feeding animals on raw meat.