Leadership Styles
advertisement

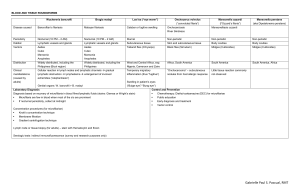
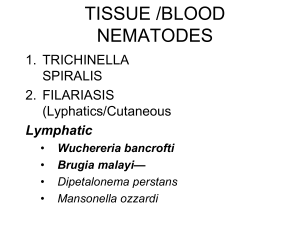
Filaria • RONALD C. CABUDOY, MD, DPSP, DHPED • wide geographic distribution • B.malayi - endemic in Asia • W. bancrofti has a larger distribution – tropical areas, worldwide • According to World Health Organization statistics, • 1 billion people in more than 80 countries • More than 120 million people have been affected more than 40 million of them are seriously incapacitated and disfigured • One third of the people infected with the disease live in India, • one third live in Africa, • and most of the remaining affected people live in Asia, islands in the Pacific Ocean, and the Americas. Filaria Wuchereria bancrofti - lymphatic Brugia malayi filariasis Onchocerca volvulus – river blindness Loa loa – eye worm Wuchereria bancrofti • • • • • • 1863 – Demarquay (hydrocele fluid) 1866 – Wucherer (chylous urine) 1872 – Lewis (peripheral blood) 1877 – Bancroft ( adult female) 1888- Sibthorpe (adult male) 1879 – Manson ( intermediate host) The disease infects an estimated 100 million people and its distribution is widespread, - South America, - Central Africa, - Middle East, - India - South East Asia. This is a disease of the lymphatic system causing a condition known elephantiasis, in which the adult worms cause damage to the lymphatic valve system which causes the lymph to drain to the extremities invading and swelling the subcutaneous tissue. Brugia malayi • • • • • 1927 – Brug ( microflaria of another species) 1940 – Rao and Maplestone (adult male and female) 1941- Bonne 1960 - Buckley Brugia malayi is a filarial worm very similar in its life cycle to W. bancrofti, except it is a zoonosis, infecting other animals as well as humans. With this parasite, depending on factors such as vector species, host range, ecosystem and geographical location the periodicity is less well defined and is known as subperiodic. A phenomenon also observed in some geographical locations where W. bancrofti is found. • Four stages of the disease are recognized. 1. The incubation period of 3 to 12 months in which there are no symptoms. 2. The acute symptomatic stage in which some swelling of the extremities may occur and this may be accompanied by pain, weakness of arms and legs, headache, insomnia. Fever is usually not present. 3. There is a period of recovery which is permanent if reinfection does not occur. 4. If there is continued reinfection the cycle repeats and elephantiasis may result. Diagnosis, Treatment and Control • The detection of microfilariae in a thick blood smear • because of its periodic nature, several smears need to be taken over a 24-hr period to confirm the presence of filariasis. • millepore filter • intradermal skin tests using Dirofilaria immitis antigen (drawback is that it cannot distinguish between past and present infections) • DEC, diethylcarbamazine is the drug of choice, • kills the larvae and adults. • The main draw back is there are frequently adverse side reactions such as nausea, dizziness and shaking. • More recently Ivermectin has been used in trials with promising results and fewer side effects. • Chemotherapeutic control of filariasis has three main objectives: 1.Reduced mortality 2.Reduced transmission by treating people with microfilaremia 3.Interrupt transmission Pathogenesis: • The worms in the lymphatic system cause tissue changes which • restrict normal flow of lymph and result in swelling, fibrosis and eventually secondary infections in the affected tissues. • The lower extremities and groin are the parts most likely to be affected. The adult worms live for several years. Complications: complications occurs as a result of the lymphedema. The most serious complication is massive infection (cellulitis, lymphangitis). Other complications include fibrosis (hardening) of the affected tissue, severe pain, gross disfigurement, sexual dysfunction. Long term fibrosis or tissue hardening can also cause venous thrombosis (blood clot). Management 1.Antibiotics to prevent secondary infections. 2.Pressure bandages to reduce swelling. 3.Surgical removal of infected tissues to improve lymph flow. 4.Chemotherapy to kill circulating microfilaria. Diethylcarbamazine (Hetrazan) 5.Vector (intermediate host) control. Wb Onchocerca volvulus • 1915 – Leukart • 1919 - Brumpt • 1927 – Blacklock (Simulium) IH • Adult worms are commonly located in nodules • Nodule may appear on any part of the body – Region of pelvic arch – Junction of long bones – Temporal or occipital regions of scalp • Adults reside typically in subcutis rather than lymphatics, (subcutaneous tissue and eye) • Typical lesion is onchocercoma – Firm, round well circumscribed subcutaneous tumor. – Composed of an outer layer of hyalinized and vascularized fibrous tissue that encloses the adult worm – 0.5-10cm in diameter or more – Fully movable Clinical Manifestations • Skin – Onchocercal dermatitis • Immune and direct irritative mechanism – Pruritus – Altered pigmentation Ocular Manifestations • Depend on the duration and severity of infection • Anatomic location of adult worm – Sclerosing keratitis – Anterior uveitis – Punctate keratitis – Iridocyclitis – Symptoms- photophobia, gradual blurring of vision – blindness • Diagnosis – Puncture of suspected tumor and discovery of microfilaria in the aspirate – Biopsy of small piece of epidermis • Treatment – Nodulectomy – DEC and Suramin – Antihistamine – Corticosteroids • Prognosis – good • Prevention – Vector control – Insecticides – Removal of nodules Loa loa (eye worm) • Humans acquires the infection from bite of IH (Chrysops silacea or dimidiata) • Forest and rubber plantation • Adult worms normally live in subcutaneous tissue migrate back and forth provoking temporary Inflammation (Fugitive or calabar swelling Causes eiosinophilia (50-70% of leukocytes) Allergic reactions (caucasians) Giant urticarial lesions of the skin and mucous membrane (back, axilla, groin, breast, penis, scalp, eyelids and bulbar conjunctiva) Fever Loaisis – traversing of the cornea beneath the conjunctiva • Other Ocular manifestations – – – – In Uganda 1. Conjunctival granulomata (Painless) 2. Edema of eyelids ( bung eye) 3. proptosis • Diagnosis: – Identification of microfilaria in peripheral smear – Removal of adult worms from the skin of conjunctiva Treatment: - surgical removal - Suramin - DEC Feature Periodicity W. bancrofti nocturnal B. malayi nocturnal Tail tapering to delicateoften constricted point, no terminal between 2 terminal nuclei nuclei Loa loa diurnal tapering gradually, caudal nuclei continuous with those of the trunk Appearance graceful sweepingstiff with secondary curves kinks similar to malayi Pathology fugitive swelling of subcutaneous tissue regional lymphadenitis similar to bancrofti and lymphanditis elephantiasis Intermediate Culex, Anopheles Mnasonia, Anopheles Chrysops host Aedes,