Lymphatic filariasis
advertisement

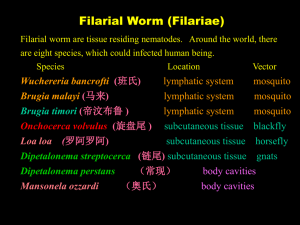
Introduction ; Definition & Epidemiology Causal Agents The Worm The vector Signs & Symptoms Risk Factors Diagnosis Treatment Prevention & Control Definition:Lymphatic filariasis, commonly known as elephantiasis, is a neglected tropical disease Filariasis (Philariasis) is a parasitic and infectious It's caused by microscopic, threadlike parasitic worm (mosquito-borne parasitic disease) that invades the body's lymphatic system. It is a disease that is characterized by the thickening of the skin and underlying tissues, especially in the legs and male genitals. Epidiomology An estimated 1.3 billion people around the world are at risk of LF infection affects over 120 million people in 73 countries. Countries where LF is found are mostly in the tropical and sub-tropical regions of Asia, Africa, the Western Pacific, and parts of the Caribbean and South America. They also are among the world’s poorest countries, as LF is closely linked to poor sanitation and poor housing quality. Geographic distribution The areas in red indicate the geographic distribution of lymphatic filariasis. Classification There are three types of these thread-like filarial worms: Wuchereria bancrofti, which is responsible for 90% of the cases. W. bancrofti is the most well-documented and widespread cause of lymphatic filariasis. It is more common to find elephantiasis in patients affected with W. bancrofti than those affected with the Brugian filariasis, although it can occur. W. bancrofti is transmitted mainly by Anopheles. They have no known animal reservoir. Brugia malayi, which causes most of the remainder of the cases. The distribution of B. malayi is very similar to that of W. bancrofti. However, cases are concentrated in Asia, including South China, India, Indonesia, Thailand, Vietnam, Malaysia, the Philippines, and South Korea. B. malayi is mainly transmitted by Mansonia mosquitos. This type of worm has been found in other mammals other than humans ; Macaques, leaf monkeys, cats and civet cats. In Indonesia, human cases have been transmitted from animals, which pose a particular challenge to the control of B. malayi. Brugia timori, which also causes the diseases. B. timori is the least common, and therefore least studied species of filaria known to cause lymphatic filariasis. This species was first reported on the island of Timor in 1964, and has since been found in other islands in Indonesia. In regards to vectors, and reservoirs, B. timori is more similar to W. bancrofti than to B. malayi. Transmission of B. timori is by the Anopheles barbirostris, also has no known animal reservoir Mode of transmission The worms are spread by mosquitoes, which picks it up from an infected person when they feed on the blood as they bite. The tiny worms develop in the mosquito over the next seven to 21 days into a larval “Infective stage” stage which can be passed on to another human when the mosquito bites them. Life Cycle & Pathogenesis Human filarial nematode worms have a complicated life cycle, which primarily consists of five stages. After the male and female worm mate(The female worms measure 80 to 100 mm in length and 0.24 to 0.30 mm in diameter, while the males measure about 40 mm by .1 mm.), the female gives birth to live microfilariae by the thousands. The microfilariae are taken up by the vector insect (intermediate host) during a blood meal. In the intermediate host, the microfilariae molt and develop into 3rd stage (infective) larvae. Upon taking another blood meal the vector insect injects the infectious larvae into the dermis layer of our skin. After approximately one year the larvae molt through 2 more stages, maturing into the adult worm. Infective larvae are transmitted by infected biting mosquitoes during a blood meal. The larvae migrate to lymphatic vessels and lymph nodes, where they develop into microfilariae-producing adults. The adults dwell in lymphatic vessels and lymph nodes where they can live for several years. The female worms produce microfilariae which circulate in the blood. The microfilariae infect biting mosquitoes. Inside the mosquito, the microfilariae develop in 1 to 2 weeks into infective filariform (third-stage) larvae. During a subsequent blood meal by the mosquito, the larvae infect the human host. They migrate to the lymphatic vessels and lymph nodes of the human host, where they develop into adults. Lymphatic filariasis is transmitted by different types of mosquitoes. Wuchereria bancrofti is transmitted mainly by Anopheles mosquitoes. Brugia malayi is transmitted by Mansonia mosquitoes. Brugia timori is transmitted by Anopheles barbirostris mosquito. Lymphatic filariasis infection involves asymptomatic, acute, and chronic conditions. Asymptomatic: Although the parasite damages the lymph system, majority of infected people are asymptomatic and will never develop clinical symptoms. These people do not know they have lymphatic filariasis unless tested. These asymptomatic infections still cause damage to the lymphatic system and the kidneys as well as alter the body's immune system. Acute: Acute episodes of local inflammation involving Skin Lymph nodes Lymphatic vessels Some of these episodes are caused by the body's immune response to the parasite. However most are the result of bacterial skin infection where normal defenses have been partially lost due to underlying lymphatic damage. Chronic: When lymphatic filariasis develops into chronic conditions, in a small percentage of people, it leads to lymphoedema (tissue swelling). This is caused by fluid accumulation due to inadequate functioning of the lymph system resulting in swelling. This mostly affects the legs, but can also occur in the arms, breasts, and genitalia. The swelling and the decreased function of the lymph system makes it difficult for the body to get rid of bacteria and unwanted pathogenes. This will result in high number of bacterial infections in the skin and lymph system causing hardening and thickening of the skin, which is called elephantiasis. Men can develop hydrocele or swelling of the scrotum due to infection with one of the parasites that causes LF specifically W. bancrofti. Filarial infection can also cause tropical pulmonary eosinophilia syndrome. This syndrome is typically found in infected persons in Asia. Clinical manifestations of tropical pulmonary eosinophilia syndrome include cough, shortness of breath, and wheezing. The eosinophilia is often accompanied by high levels of IgE (Immunoglobulin E) and antifilarial antibodies Patient with elephantiasis Patient with lymphedema. Since lymphatic filariasis does not always result in clinical symptoms, it is very critical to perform diagnostic test to determine the diagnosis. Microscopic Examination of blood smear: identification of microfilariae in a blood smear by microscopic examination it is the standard method for diagnosing an active infection. Serologic techniques: provide an alternative to microscopic detection of microfilariae Patients with active filarial infection typically have elevated levels of antifilarial (IgG4) in the blood and these can be detected using routine assays. Immuno chromatographic test ( ICT ): antigen detection assay it can be done by card test or through ELISA. Circulating Fitarial Antigen detection is the “ Gold Standard “ for diagnosing Wuchereria bancrofti . The left ICT card displays negative results for LF infection, while the right card displays positive results Non pharmacological treatment: 1) Wearing shoes that can help prevent further exposure to the irritants. 2) Compression bandage and elastic stocking can also help manage the swelling and inflammation caused by this condition. 3) Physicians often suggest cleaning the affected area with soap and water, as well as soaking the area in a mixture of water and antiseptic, for the management of non-filarial elephantiasis. Medications The most commonly used drugs for the treatment of lymphatic filariasis are: ✦ Albendazole ✦ Diethylcarbamazine ✦ Ivermectin » Albendazole and diethylcarbamazine have been found to be effective in killing the microfilariae, and also the adult worms. However, in the sub-Saharan Africa, albendazole is usually used along with ivermectin. Ivermectin can kill the microfilariae, though its effects on the adult worms are not very clear. » Diethylcarbamazine is often regarded as a better option than ivermectin for killing adult worms. This medicine is also effective in reducing the size of enlarged lymph nodes considerably. However, this medicine can sometimes produce an allergic reaction, which can necessitate the use of antihistamines and steroids. This side effect is generally attributed to the destruction of the parasites. As the parasitic worms die, they release certain chemicals that can produce the allergic reaction. » Antibiotics such as doxycycline has also shown some promising results in treating lymphatic filariasis. The parasitic worms that cause elephantiasis have a population of symbiotic bacteria, known as Wolbachia, without which they cannot survive. Antibiotics help destroy these symbiotic bacteria, and thus wipe out the parasitic worms as well. » Along with medications, regular cleaning of the affected area can also help control the symptoms of elephantiasis to a great extent. This is probably due to the fact that, many times secondary skin infections play a very important role in aggravating the symptoms of elephantiasis. Daily cleaning can help prevent secondary infections. Surgery When elephantiasis causes gross enlargement of the scrotum, then surgery may be required to address this condition. However, surgery is usually ineffective in resolving the swelling of the limbs or trunk. Class: benzimidazole drug Indication: is an orally administered broad-spectrum anthelmintic e.g. Neurocysticercosis, Hydatid Disease Mechanism of action Albendazole causes degenerative alterations in the intestinal cells of the worm by binding to the colchicine-sensitive site of tubulin, thus inhibiting its polymerization or assembly into microtubules. The loss of the cytoplasmic microtubules leads to impaired uptake of glucose by the larval and adult stages of the susceptible parasites, and depletes their glycogen stores. Also, degenerative changes in the endoplasmic reticulum, the mitochondria of the germinal layer, and the subsequent release of lysosomes result in decreased production of adenosine triphosphate (ATP), which is the energy required for the survival of the helminth. Due to diminished energy production, the parasite is immobilized and eventually dies Side Effects: Serious S.E easy bruising or bleeding, unusual weakness fever with chills, body aches, or flu-like symptoms leukopenia ; aplastic anemia, bone marrow suppression and agranulocytosis Less Serious S.E. stomach pain nausea, vomiting headache, dizziness temporary hair loss PRECAUTIONS: This medication may cause liver problems. Patients with liver disease, appear to be more at risk of bone marrow suppression Albendazole should not be used in pregnant women except in clinical circumstances where no alternative management is appropriate. Patients should not become pregnant for at least 1 month following cessation of albendazole therapy. If a patient becomes pregnant while taking this drug, albendazole should be discontinued immediately. Pharmacokinetics Absorption Albendazole is poorly absorbed from the GI tract; however, it is rapidly converted to its primary active metabolite, albendazole sulfoxide, prior to reaching systemic circulation. Fatty meals enhance bioavailability, as indicated by up to a 5fold increase in plasma concentration in albendazole sulfoxide Disturbution Albendazole sulfoxide is 70% protein bound and widely distributed throughout the body. Metabolisim Hepatic metabolsim Class: Diethylcarbamazine citrate is derived from the anthelminthic agent piperazine. Indication: Used for the treatment of individual patients with certain filarial diseases including tropical pulmonary eosinophilia, loiasis, and lymphatic filariasis caused by infection with Wuchereria bancrofti, Brugia malayi, or Brugia timori. Mechanism of Action: Proposed mechanisms of action include platelet-mediated triggering of the release of excretory antigen from microfilariae, with killing involving free radicals, druginduced alteration of prostaglandin metabolism in microfilariae and/or in host endothelial cells, leading to immobilization of microfilariae on endothelial surfaces and adherence and killing by host platelets and granulocytes and inhibition of microtubule polymerization. 1) 2) 3) 4) Side Effects: More common Itching and swelling of the face, especially the eyes Headache Joint pain Unusual tiredness or weakness Less common 1. Fever 2. Painful and tender glands in the neck, armpits, or groin 3. Skin rash 4. Dizziness 5. Nausea or vomiting Pharmacokinetics: Absorption: readily absorbed following oral administration. Distribution: widely distributed throughout all body compartments, except adipose tissue, Half-life: 8 hr Metabolites: diethylcarbamazine N-oxide, -Excretion: urine & feces Pregnancy:No data exist regarding the safety or dose modification of the drug in pregnancy. Indication: Used as an Anthelmintic, Antiprotozoal Agent, and Antinematodal Agent Mechanism of action Ivermectin binds selectively and with high affinity to glutamate-gated chloride ion channels in invertebrate muscle and nerve cells of the microfilaria. This binding causes an increase in the permeability of the cell membrane to chloride ions and results in hyperpolarization of the cell, leading to paralysis and death of the parasite. Ivermectin also is believed to act as an agonist of the neurotransmitter gamma-aminobutyric acid (GABA), thereby disrupting GABA-mediated central nervous system (CNS) neurosynaptic transmission 1) 2) 3) 4) Side Effects : Headache, dizziness, muscle pain, nausea, or diarrhea may occur. Precautions : allergic reactions. liver problems, Limit alcoholic beverages During pregnancy, this medication should be used only when clearly needed. Ivermectin passes into breast milk. Though there have been no reports of harm to nursing infants. Pharmacokinetics: Absorption: Readily absorbed. Distribution: Due to the high lipid solubility of ivermectin, this compound is widely distributed within the body. However it does not cross the blood brain barriers in humans and most mammalians Ivermectin binds strongly to plasma proteins in healthy subjects (93.2%) Elimination: This drug is extensively metabolized by human liver microsomes by cytochrome P450. Half life: 22 to 28 hours. The best way to prevent lymphatic filariasis is to avoid mosquito bites. The mosquitoes that carry the microscopic worms usually bite between the hours of dusk and dawn. If you live in an area with lymphatic filariasis: at night sleep in an air-conditioned room sleep under a mosquito net between dusk and dawn wear long sleeves and trousers and use mosquito repellent on exposed skin.