Edema
Disorders
Kade Scott DPT, CLT
Objectives
Understand
and recognize different
edema disorders
Understand basic treatment options for
edema disorders
Explain the differences in compression
garments
What does the Lymphatic
system do?
The
lymph system is responsible for
transporting
Proteins
Water
Cells
Fat
Waste
WBC, lymphocytes, Bacteria, Virus
Lymphedema
An
abnormal accumulation of protein rich
fluid in the interstitum, which causes
chronic inflammation and reactive fibrosis
in the affected tissue
Lymphedema is classified as either
primary or secondary lymphedema
Typically asymmetrical
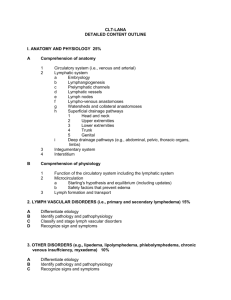
From: Differential Diagnosis, Investigation, and Current Treatment of Lower Limb Lymphedema
Arch Surg. 2003;138(2):152-161. doi:10.1001/archsurg.138.2.152
Figure Legend:
Causes of lymphedema.
Date of download: 2/17/2014
Copyright © 2014 American Medical
Association. All rights reserved.
Primary Lymphedema
The most likely occurrence of this form is
lymphangiodysplasia
Hypoplasia- less than normal expected number
of lymph collectors in the affected area
Aplasia- a distinct absence of lymph collectors
in the affected area. May also involve the
absence of lymph capillaries
Hyperplasia- Vessels are characterized by an
excessively dilated caliber which renders them
less functional due to valvular dysfunction
Primary Lymphedema
http://www.sajch.org.za/index.php/SAJCH/arti
cle/view/639/453
Present at birth or
shortly therafter is
known as Milroy’s
Disease
Primary Lymphedema
that develops during
puberty is known as
Meige’s Disease.
Praecox- Develops
before 30
Tardum- Develops after
35
Secondary Lymphedema
Secondary lymphedema means there is a
known cause for the presence of
lymphedema
Worldwide the most common cause is the
mosquito born parasite Filaria
In the United States the most common cause
is cancer therapy
Lymph node sampling
Full dissection of lymph nodes
Radiation therapy
Secondary Lymphedema
(cont)
Other
causes include any significant
trauma to the lymphatic system from
accidental or self induced incidents,
infectious episodes such as eyrsipelas or
cellulitis
Obesity may also play a role in the
development of lymphedema, however,
it is more likely due to a secondary comorbidity (lack of mobility, CVI etc)
Staging of lymphedema
Lymphedema
is divided into 4 stages
(American Society of Lymphology)
Latency stage (subclinical or stage 0)
Transport
capacity of the lymphatic system is
sub-normal but still sufficient to transport the
lymphatic load
Patients are “at risk” for developing
lymphedema
Education about subjective complaints and
preventative measures is key component of
treatment at this stage
Staging
Stage
1 (reversible stage)
Accumulation of protein rich fluid
No fibrotic alterations
Pitting is easily induced
With proper management of stage 1
patient can expect to have reduction to
normal limb size
Stage 1 is often confused with edemas of
other geneses
Staging
Stage 2 (spontaneously
irreversible)
Lymphatic fibrosis
Tissue becomes
indurated
Pitting is difficult to
induce
Positive Stemmer sign
Common cellulitic
infections
Incomplete reduction
with therapy and good
patient compliance
Stemmer Sign
Sometimes called the Kaposi
Stemmer sign
Staging
Stage 3 (Lymphostatic
Elephantitis)
Increased skin firmness,
other skin alterations
including: cysts, fistulas,
papillomas,
hyperkeratosis, mycotic
infections, ulcerations
More prominent
Stemmer sign
Recurrent cellulitis
Decreased pitting
http://www.womenshealthsection.com/content/gyno/gyno005.php3
Symptoms
Swelling of an arm or leg, which may include fingers and toes.
A full or heavy feeling in an arm or leg.
A tight feeling in the skin.
Trouble moving a joint in the arm or leg.
Thickening of the skin, with or without skin changes such as blisters or warts.
A feeling of tightness when wearing clothing, shoes, bracelets, watches, or
rings.
Itching of the legs or toes.
A burning feeling in the legs.
Trouble sleeping.
Loss of hair.
Positive Stemmer Sign (though the absence does not rule out lymphedema)
These symptoms may occur very slowly over time or more quickly if there is an
infection or injury to the arm or leg.
Chronic Venous Insufficiency
Is
an advanced stage of venous disease
in which the veins and the muscle pump
activity become incompetent causing
blood to pool in the legs and feet
Can be due to repeated damage from
superficial or deep venous pathology, or
a variety of vein-related conditions such
as the congenital absence of valves
Pathophysiology of CVI
Faulty
valves fail to prevent retrograde
flow of venous blood during muscle pump
activity
May be:
Idiopathic
Post-thrombotic syndrome
Genetics
Pelvic tumors
Vascular malformations
Symptoms
Swelling
in the lower legs and ankles,
especially after extended periods of
standing
Aching or tiredness in the legs
New varicose veins
Leathery-looking skin on the legs
Flaking or itching skin on the legs or feet
Stasis ulcers (or venous stasis ulcers)
Hemosiderin staining
Hemosiderin staining
Risk factors
Deep vein thrombosis (DVT)
Varicose veins or a family history of varicose
veins
Obesity
Pregnancy
Inactivity
Smoking
Extended periods of standing or sitting
Female sex
Age over 50
Early stages of CVI
Pitting Edema
Mostly presenting
below the knee
Corona
Phlebectatica
http://www.medicographia.com/wpcontent/uploads/2011/10/17.JPG
A myriad of tiny vein
branches that are
difficult to delineate
Red-pink hue to skin
that returns
immediately after
pressure is released
Advanced stages
Hyperpigmentation
Dermatologic changes
Venous stasis dermatitis
Lipodermatosclerosis
Scarring and fibrosis
of skin (woody texture
to skin)
There may now be a
lymphatic
component to
edema
http://www.veinsveinsveins.com/app/webro
ot/files/lipo.11.jpg
End Stage CVI
Defined by ulcerations of the
skin
Photo Credit: Charlie Goldberg
http://meded.ucsd.edu/clinicalimg/e
xtremities_venous_insuf4.htm
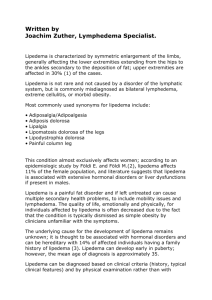
Lipedema
A
chronic
metabolic disorder
of the adipose
tissue, of unknown
etiology.
http://www.amylhwilliams.com/BEFOREAmyslegsfront1.jpg
Lipedema
Predominately
in women
Bilateral symmetrical swelling from illiac
crest to ankles
Stemmer’s sign negative
No cellulitic infections
Foot sparing
Lipedema
“I
can never lose weight in my legs no
matter how much I diet”
Very tender skin
Bruise easily
Lipedema
Stage 1
Stage 2
Skin surface is normal, tissues exhibit a smooth
nodular texture
Skin surface becomes more uneven, large fatty
lobules begin to form
Stage 3
Large contour deforming lobular shapes on
medial knee, proximal lateral thigh, and above
malleoli
Lipedema Staging
http://www.nature.com/aps/journal/v33/n2/fig_tab/aps2011153f4.html
Traumatic Edema
Edema
due to physical trauma
Results in inflammatory reactions
accompanied by high protein edema.
The majority are temprorary and self
resloving. However, it can lead to
permanent damage.
Pathophysiology of traumatic
edema
The
initial step in the inflammatory process
causes local vasodilation, followed by an
increase in the permebility of blood
capillaries toward plasma protein.
Macrophages invade and devour
damage tissue. These macrophages may
injure the lymhpatic system.
Cardiac Edema
Greatest
distally
Always Bilateral
Pitting
Complete resolution with elevation
No pain
Congestive Heart Failure
Same
symptoms as in cardiac edema
Orthopnea, paroxysmal nocturnal
dyspnea, dyspnea on exertion
Jugular venous distension
Cardiac echo, Physical exam
Renal Failure and Edema
Increased
protein in the urine
Decreased blood protein
Pitting edema in lower extremity
How do I
differentiate?
And then what?
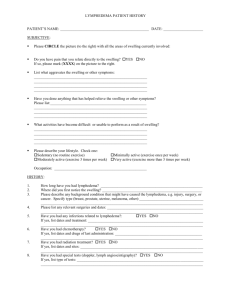
Accurate Pt Hx
Patient
history is crucial in determining the
underlying cause of edema
There are many questions that you can ask
that will help guide you down the proper
course
Intake Questions
Have
you had any lymph nodes
removed?
Any recent abdominal surgeries?
Any history of DVT?
Previous cellulitic infection?
CHF?
Renal Failure?
•MLD
•Compression Bandage
•Compression Stockings
Lymphedema •Pneumatic Compression
Lipedema
CVI
Traumatic
Edema
Cardiac, CHF,
Renal
•Light MLD
•Compression Stockings
•Compression Bandage
•Compression Bandaging
•Compression Stockings
•Pneumatic Compression
•MLD above level of injury
•Compression Bandaging
•Compression bandaging and stockings as tolerated. You MUST consult a physician on these patients prior to
initiating any treatment
2 phases to treatment
Reduction
MLD
Compression
bandaging
Pneumatic
compression
Exercise and skin
care
Maintenance
Compression
Stockings
Pneumatic
Compression
Exercise, Skin care
Manual Lymphatic Drainage
A general manual treatment which improves
lymph vascular flow. In lymphedema it reroutes the lymph fluid around blocked areas
into more centrally located healthy lymph
nodes
It is not a massage!
Must be done by someone who is properly
trained
Contraindications to MLD
CHF
if patient is unmedicated or edema is
due solely to cardiac failure
Acute infection
Renal Failure
Acute DVT (seek physician approval for
post thrombotic syndrome edema
management)
Compression Bandaging
Short stetch bandages are applied to
increase the tissue pressure in the swollen
extremity
Improves the efficiency of the muscle
pump and joint pumps
Prevents the reacummulation of
evacuated fluid
Helps break up deposits of accumulated
scar and connective tissues
Contraindications to
compression bandaging
Acute
DVT (may mobilize thrombus)
Acute infection
Cardiac edema
Advanced arterial disease <.7 on the ABI
Advanced renal disease
Malignancy (relative to severity)
Bandaging
Short
stretch-
Unna, Comprilan
Medium
Coban
Co-Plus
Long
Stretch
Ace
4-layer
stretch
Profore
Short stretch
Reduce
deep venous reflux more
effectively
High working pressure to low resting
pressure. Produce high pressure
amplitudes when patient is walking and a
decrease in pressure when patient is
supine
Main disadvantage is the loss of pressure
following reduction
Short Stretch
Comprilan
Bandage
http://curept.com/multi-layerbandaging/
Medium stretch
Sustains
compression after an initial
decrease
Has a fair working to resting pressure ratio
2-layer Wrap
http://solutions.3m.com/wps/portal/3M/en_EU/HealthcareEurope/EUHome/Products/ProductCatalogue/?PC_Z7_RJH9U52300PI40IA
1Q602S28E7000000_nid=5W2H1K4LB0be56F5WHWNG2gl
Long Stretch
Maintain
pressure for longer periods of
time
A higher pressure of at least 60 mmHg is
required to prevent reflux
Exert a high resting pressure which can
constrict the venous and lymphatic
systems creating a tourniquet effect
Helping Patients & Physicians Heal
Pneumatic Compression
Therapy
Before
Pneumatic Compression
Therapy
Before
After 2 Weeks Pneumatic Compression
Pneumatic Compression Pump
Mechanism of Action
A gentle “milking” of lymphatic fluid out of
the upper extremity. This distal to proximal
motion allows for a clearance of lymphatic
fluid to be filtered out of the system via the
urinary tract.
In essence the Pneumatic Compression
pump is designed to ‘do’ what the body is
incapable of due to age, damage or disease
state.
Contraindications
Inflammatory Phlebitis
Episodes of Pulmonary Embolism
Infections in limb without appropriate
antibiotic coverage*
Presence of Lymphangiosarcoma
Congestive Heart Failure, Uncontrolled
*48 hours
Pneumatic Compression Therapy
Convenient home use
Comprehensive in-home or office patient
training
Easy to use
Medicare and private insurance coverage
Custom sizing
Adjustable
Ability to clean the product-sanitary
Patient dictated time of use
Lifetime treatment of underlying condition
Compression garments
Class
0 10-20 mmHg
Class 1 20-30 mmHg
Class 2 30-40 mmHg
Class 3 40-50 mmHg
Class 0
Preventative
only
Should not be used for someone with
active edema
Class 1 20-30 mmHg
Minimum
compression for UE
lymphedema
Offer support, but NOT sufficient for lower
extremity lymphedema or CVI
Class 2 30-40
Most
stage 2 upper extremity
lymphedema
Minimum compression for LE lymphedmea
Offers good support for LE CVI
Class 3 40-50 mmHG
Rarely
used in UE lymphedema
Most stage 2 LE lymphedema
Minimum starting point for stage 3
lymphedema
Consideration for garment
selection
Patient
ability to manage garment
Material allergies
Price
Insurance coverage
Flat knit vs Circular knit
Flat
Custom only
Slightly easier to don
The thicker fabric offers
additional features, such as its
massaging effect, which
promotes lymph drainage, and
its strength, which ensures the
stocking does not yield to the
edema. In conjunction with
movement, it produces a high
therapeutic pressure that
provides optimum compression
of the tissue.
Circular
Custom or OTS
Difficult to don
Single layer of fabric
Not appropriate
compression for active
lymphedema, may not
be adequate for sever
venous edema
Cheaper
Goals for compression
garments
MAINTAIN
limb volume after
decongestion. Compresion garments will
NOT decongest limb
Easy don/doffing to enhance patient
compliance
Cosmetically appealing
References
Diseases and Conditions: Chronic Venous Insufficiency
(CVI).
http://my.clevelandclinic.org/disorders/venous_insufficienc
y/hvi_chronic_venous_insufficiency.aspx. Accessed 2-26-14.
Greenlee R, Hoyme H, Witte M, Crowe P, Witte C.
Developmental Disorders of the Lymphatic System.
Lymphology. 26 (1993): 156-158.
Managing edema to decrease pain and increase range of
motion and functional mobility. Loraine Lovejoy-Evans MPT,
DPT, CLT-Foldi.
Mcdonald J, Sims N, Mayrovitz H. Lymphedema, lipedema,
and the open wound. The role of compression therapy.
Surgical Clinicals of North America. 83 (2003): 639-658.
References
Norton School of lymphatic therapy course
manual: Manual Lymphatci Drainage/Complete
Decongestive Therapy .
Rathbun SW, Kirkpatrick AC. Treatment of chronic
venous insufficiency. Curr Treat Options
Cardiovasc Med. 2007 Apr;9(2):115-26.
Szuba A, Rockson S. Lymphedema: classification,
diagnosis and therapy. Vascular Medicine. 1998:
3:145-156.
Zuther J, Norton S. Lymphedema Management:
the comprehensive guide for practitioners. 3rd ed.
New York, NY: Thieme Medical Publishers; 2013.
LE Short Stretch
Compression
Foam
Open
Cell Grey Foam
Komprebinde
Komprex
Rosidal Soft
LE bandaging
Lotion
Stockinette to calf
Toe wraps
Cotton (knee, foot)
Foam (affix to calf)
Foam (affix to ankle
and dorsum of foot)
Eucerin or other low pH
TG or Tricofix
Transelast/elastomull
Cellona/Artiflex
LE bandaging
Roman Sandal
Ankle sole heel (ASH, Has)
Spiral ankle to knee
Herring bone/Figure 8
Stockinette to thigh
Affix foam to thigh
Knee to mid thigh
Knee to top
Distal thigh to top
6cm Comprilan/Rosidal K
8cm
10 cm
10 cm
12 cm
12cm
12 cm