Andrew_Gratzon_Lymphedema_abstract_for_Fl_College_of_Surg
advertisement

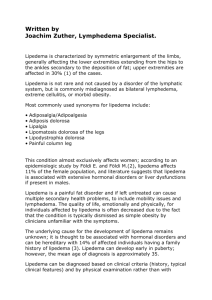
VASCULARIZED LYMPH NODE TRANSFERS FOR TREATMENT OF UPPER EXTREMITY LYMPHEDEMA AFTER BREAST CANCER THERAPY Andrew Gratzon, MDa, Allyson Deziel, BSb, James Kotick, MDa, Kristine Secrest, OTR/L, CLT-LANAa, Kenneth Lee, MD, FACSa, Jeffrey Feiner, MDa, Richard Klein, MD, MPH, FACSa Background It is estimated that approximately 6.8 million people suffer from lymphedema in the United States. The majority of these cases are classified as secondary lymphedema, which results from a disruption of the lymphatic drainage by an acquired blockade. Secondary lymphedema is seen in many patients following breast cancer surgery, especially in those who require radiation therapy and axillary lymph node dissection. In addition to swelling, these patients can experience pain, heaviness, restricted motion and recurring infections all leading to poor quality of life. Currently the most widely used non-surgical treatment for lymphedema is complete decongestive therapy (CDT), which involves compression sleeves/gloves, bandaging or bulky night garments, self manual lymph drainage, exercises and meticulous skin care. CDT is often a lifelong treatment that is rigorous and time consuming. Vascularized lymph node transfer (VLNT) is a surgical treatment for lymphedema that re-establishes local flow within the lymphatic channels. VLNT offers the possibility of reduction or elimination of symptoms, significant improvement in quality of life, and reduction or cessation of CDT. Objectives The goal of this prospective, ongoing study is to investigate the clinical and psychosocial outcomes of patients undergoing vascularized lymph node transfer for the treatment of upper extremity lymphedema after breast cancer therapy. Methods The inclusion criteria for patients included development of lymphedema following breast cancer therapy and having an indication for VLNT surgery [lymphedema resistant to conservative therapy, chronic infections, ongoing pain, or worsening lymphedema]. There were forty-five patients that met this criteria. Patients were evaluated preoperatively and postoperatively at 1,3,6,9 and 12 month intervals by circumferential measurements, pain/heaviness scales, and the LymQOL for quality of life. A frustum formula was used to calculate the volume of each arm and then a percentage difference was used to compare the affected and unaffected arms. At every reassessment interval, the volume differences between the arms were compared to the preoperative volume difference to achieve a percentage of reduction in edema; this accommodated for overall changes in weight or fluid retention. Before surgery all of the patients had a bilateral MR lymphangiogram to locate any visible lymphatic blockage. During the procedure, visible scar tissue was first removed from the axilla to create a pocket for the flap. A flap of soft tissue containing the lymph nodes was harvested from a donor site. The donor site varied based on patient anatomy and included the neck for three patients, the chest wall for four patients, and the lower abdomen for thirty-six patients. After the flap was raised and inset into the pocket, the microscope was used to connect the artery and vein. Then an intraoperative angiogram was performed to ensure adequate flow to the flap before closing the incision. Results Preliminary results showed a decrease in arm volumes by 23.47% at 1 month, 25.8% at 3 months, 45.62% at 6 months, 60% at 9 months, and 46.7% at 12 months. Pain and heaviness consistently decreased over time to 0 and 0.2 respectively at 12 months. For many patients in this study, only minimal CDT was required postoperatively to maintain the decreased arm volume. Overall quality of life scores improved from 5.4 at pre-op to 6.7 at 1 month, 6.9 at 3 months, 7.1 at 6 months, 8.7 at 9 months, and 9.3 at 12 months. There was also a significant decrease in the number of infections of the affected arm postoperatively. VLNT continues to demonstrate its value as an effective treatment option and has the ability to transform the outlook for patients afflicted with upper extremity lymphedema. a Orlando Health, Orlando, FL, bUniversity of Central Florida College of Medicine, Orlando, FL