Lymphedema – Frequently Asked Questions What is Lymphedema
advertisement

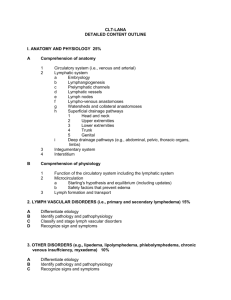
Lymphedema – Frequently Asked Questions What is Lymphedema? Lymphedema is a protein rich swelling or collection of fluid usually in the arms or legs. It can also affect the abdomen, chest, back, groin, head and neck. What is the Lymphatic System? Our lymphatic systems form part of our circulatory system. A complex network of vessels and nodes drain the clear fluid from the tissues and organs that make up our anatomy and transport it to the heart where it re-enters the blood system. It is not only a drainage system but an intrinsic part of our immune system for controlling infection. What causes Lymphedema? Lymphedema is the result of a compromised lymphatic system. This can be primary lymphedema, which is genetic/congenital (born with an incomplete lymphatic system) or it can be secondary lymphedema where the lymphatic system is damaged through illness (vascular disease, diabetes), injury or trauma to the body, for example, vascular disease, surgery, radiation or chemotherapy. How is Lymphedema diagnosed? There is no medical test for lymphedema. Patients do however report consistent symptoms that allow a health care professional to diagnose lymphedema. These are: Copyright: Restorative Therapies Mauritius Limited - Any persistent and unexplained swelling in any part of the body. - A full or heavy sensation in a limb. - A lack of symmetry and finding that clothes are tighter on one arm or leg. - Decreased flexibility in an arm or leg. A thorough medical evaluation and questionnaire is needed to confirm a diagnosis of lymphedema. A growing education and understanding of the disease in recent years means that more patients are getting treatment sooner and preventative therapy is becoming standard in countries such as North America, France, Germany and Austria. What are the stages of Lymphedema? Lymphedema develops in stages from mild (stage 1) to severe (stage 3). It is a progressive disease and without treatment a patient will usually progress to stage 3 over a period of time. Stage 1 Pushing your finger into the skin will leave an indentation. This is known as ‘pitting’ and is the result of lymph fluid collecting in the tissues. There is mild visible swelling or heaviness to the area but it is usually resolved by elevating the limb, resting or lying down. Once the patient is up and mobile, the swelling returns. Stage 2 Increased swelling and loss of symmetry are visible. The limb will be noticeably larger and as the tissues begin to harden (fibrosis begins), pitting will no longer be possible. Elevating the limb and rest no longer reduce the swelling. Stage 3 The swelling is now irreversible and skin changes are visible. Fibrosis and papilloma’s form and the skin becomes hardened and resistant to treatment. Infections (cellulitis) are common as the immune system to the area is compromised allowing bacteria and fungus to grow. This is a very traumatic stage for any patient. It affects quality of life; mobility and can often lead to depression. Is Lymphedema Treatable? Yes. Lymphedema is treated by managing the symptoms using Complete Decongestive Therapy or CDT. What is Complete Decongestive Therapy? CDT is the gold standard in the treatment of lymphedema. It consists of the following therapies: Intensive Phase (1-4 weeks approximately) - Manual Lymph Drainage – A hands-on therapy where gentle and precise stretching movements to the skin result in protein rich fluid draining from the affected area. Existing drainage pathways are stimulated and new drainage pathways established. - Compression Bandaging (day and night)– short stretch (no-elastic) bandages are applied to encase the affected area. The bandages support the limb and the natural movement of the body and muscles within this non-stretch ‘shell’ pump fluid out the affected area. Copyright: Restorative Therapies Mauritius Limited - Exercise – Gentle and appropriate exercise is an important part of the treatment. Muscle movement within the compression bandages acts as a pump to further drain fluid from the affected area. - Meticulous Skin Care – Daily skin care and cleaning are essential. - Education and Support – both the patient and a family member(s) or carer will be taught how to self-administer basic MLD; apply bandages and use compression garments. The Maintenance Phase - Compression garments – lymphedema is a chronic condition and following the intensive phase, a patient will need to maintain and control the swelling. Compression garments are custom made and fitted for each patient and they need to be worn every day to avoid fluid collecting in the affected area. They are made from breathable flat-knit fabrics. - Bandaging at night – patients will be taught how to comfortably apply a compression bandage at night. - Exercise – Keeping the muscle pump working and maintaining a healthy weight are important goals with long term management of Lymphedema. - MLD – as and when needed. - Meticulous Skin Care and Precautions - patients are taught how to keep their skin in top condition and how to reduce the risk of injury to the skin that can lead to infection. Copyright: Restorative Therapies Mauritius Limited