Urinalysis - Jacobi Medical Center
advertisement

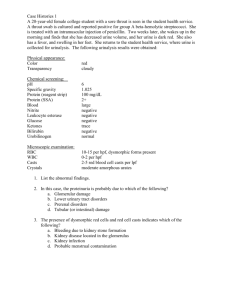
Urinalysis Belinda Jim, MD July 17, 2009 Urinalysis • Major noninvasive tool • Provide information about disease severity, though not always a direct relationship • Specimen should be examined about 30-60 minutes of voiding • Sample centrifuged at 3000 rpm for 3-5 minutes, supernatant be tested by dipstick Color • Normal color is clear and light yellow • White- pyuria or phosphate crystals • Green- administration of methylene blue, amitriptyline, propofol • Red or Brown- due to blood Turbidity Normal urine should be clear Turbidity indicates: •cellular material •bacteria •protein •lipids •crystals •salt precipitation Odor • Normal odor is urinoid • Ammonia- related to UTI, prolonged urinary retention • Sweetish- diabetic ketoacidosis due to acetone • Sulfuric- cysteine decomposition • Drugs/Foods- e.g. antibiotics, asparagus Test Reagent Strip Protein • Detects primarily albumin • Highly specific, but not sensitive • Positive only when protein excretion > 300500 mg/day • Not good to detect microalbuminuria or immunoglobulin light chains Sulfosalicylic acid test (SSA) • SSA detects all proteins in the urine • Especially useful if suspects multiple myeloma in which immunogloblin light chains form casts that obstruct the tubules • A positive SSA test in conjunction with a negative dipstick indicates presence of non-albumin proteins in urine • Mix 1 part urine supernatant with 3 parts SSA (3%), grade its turbidity pH • Reflects degree of acidification of urine • Urine pH ranges from 4.5 to 8.0 • Major clinical use for patient with metabolic acidosis • Appropriate response to increase urinary acid excretion, with urine pH falling below 5.3 • A higher value indicate presence of RTA or infection Ketones • Detects acetone and acetoacetate using nitroprusside reaction • Does not detect b-hydroxybutyrate • Presence in the urine indicates diabetic ketoacidosis, starvation ketosis, low carb diet Bilirubin/Urobilinogen • Normal bilirubin not detected in urine • If increased conjugated bilirubin in urine, indicates liver dysfunction • Bilirubin metabolized by bacteria in the intestines to form urobilins • Small % absorbed in intestine and appears in urine Osmolality and specific gravity • Osmolality- number of solute particles per unit volume • Specific gravity- weight of solution compared with weight of water – Generally varies with osmolality, though presence of large molecules in urine, such as glucose or radiocontrast media can produce large changes in specific gravity with little changes in osmolality Glucose • Presence of glucose indicates inability to reabsorb filtered glucose in the proximal tubule despite normal plasma levels • OR urinary spillage due to abnormally high plasma concentrations • Generally glucosuria does not occur until plasma glucose exceeds 180 mg/dL Hematuria and Pyuria • Dipsticks very sensitive in detecting rbc’s, as few as 1 to 2 rbc’s per high power field • Detect leukocyte esterase (pyuria) and nitrite (enterobacteriaceae converts nitrate to nitrite) • Sterile pyuria: interstitial nephritis, renal tuberculosis, and nephrolithiasis Urine sediment • • • • • • Crystals Bacteria Red blood cells (0-2 rbc’s in normal) White blood cells (0-4 wbc’s) Casts Artifact Crystals • Calcium phosphate or calcium oxalate crystals • Uric acid crystals • Magnesium ammonium phosphate crystals • Cystine crystals Bacteria • Significance depends on quality of collection • More significant in presence of wbc’s and other elements • Urine in the bladder should be sterile, but becomes contaminated as it passes through bladder Hematuria • Transient hematuria - relatively common in young subjects, not indicative of disease • Persistant hematuria- gross or microscopic – Morphology is important, usually uniform and round with extrarenal bleeding – Dysmorphic appearance with renal lesions, I.e. blebs, budding, segmental loss of membrane Pyuria • White cells are larger than red cells, granular cytoplasm and multilobed nuclei • Pyuria alone usually indicated infection • Less diagnostic value when seen with other elements such as cellular casts, and/or proteinuria • Eosinophils may indicate allergic interstitial nephritis, cholesterol emboli disease • Lymphocytes seen in disorders associated with infiltration of kidney by lymphocytes, such as chronic tubulointerstitial disease Epithelial Cells • May be shed anywhere within the GU tract • Only renal tubular cells are significant • Generally 1.5 to 3 times larger than white cells, contain a round, large nucleus • May be normal or indicative of ATN, pyelonephritis, nephrotic syndrome Casts • Conform to the shape of the renal tubule in which they form • Organic matrix composed mostly of TammHorsfall mucoprotein • Types of casts: hyaline, red cell, white cell, epithelial, granular, waxy, broad Theory of Casts Genesis • Key: A = Cellular casts B = Coarsely granular cast C = Finely granular cast D = Waxy cast RBC cast ©2005 UpToDate® e-mail this to a colleague Miscellaneous Findings Trichomonas Vaginalis Sperm Talc Fiber Case 1 • A 46 y.o. man with HTN presents with acute right flank pain that moves around. He is slightly febrile to 100.4 C. Exam unremarkable. UA shows hematuria. Case 2 • A 22 y.o. woman with no significant past medical history presents with dysuria, ammonia-smelling urine and increased urinary frequency for 3 days. • What will her UA show? • What do you expect on the urine sediment? Case 3 • A 57 y.o. woman with h/o poorly controlled HTN and DM, diabetic retinopathy presents with creatinine of 1.8 and lower extremity edema. • What would you expect your UA to show? • What would you do next? Case 4 • A 3-year old boy brought to pediatrician for increasing facial and peripheral edema of eight days duration. Urine- 4.2 grams protein/24 hours, cholesterol 450 mg/dl, albumin 3.0 g/dl Case 5 • A 45-year old man hospitalized for peripheral edema and proteinuria. Urine-6 g protein/24 hours, albumin 1.6 g/dl. Cholesterol 380 mg/dl. Creatinine 1.6. Review of medical records showed he had 1+ proteinuria four years previously. Case 6 • A 52-year old woman with sudden onset of edema, “dark urine”, headaches, malaise. BP: 150/105, urine 900 cc/24 hr, 1.7g protein/24 hours, creatinine 4.5 mg/dl, BUN 68 mg/dl. Review of records show that she had normal renal function 1 month ago.