Project Review Event Template_SHUNKrevised
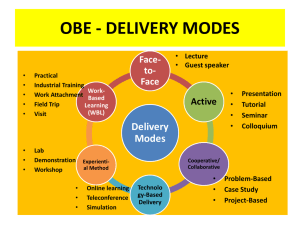
advertisement

Te4Q Educational Project Review Interprofessional Continuous Quality Improvement and Patient Safety Curriculum: A Guide for Clinical Faculty/Mentors in Primary Care Settings JoAnne M. Saxe, DNP, ANP-BC Maya Dulay, MD Rebecca Shunk, MD Bridget O'Brien, PhD Goal/Aim Overall aim: Increase the number/ expertise of faculty CQI leads to 8 interprofessional faculty (IP) by 9/1/16 as demonstrated by these IP faculty developing and leading a CQI session or developing or evaluating an eposter. Process aim: At the end of the 6 month curriculum 100% of faculty will demonstrate an increase in their knowledge, skills, and confidence in teaching CQI concepts and mentoring CQI projects by presenting their own CQI curriculum or trainee team projects to faculty peers at monthly faculty development meetings. Logic Model Resources/Inputs Resources needed to operationalize the curriculum Activities Activities that need to be completed to assure successful implementation and evaluation of the curriculum Outputs If we complete the expected planned activities, several outputs will likely be assured. Outcomes If we accomplish the intended planned activities, then the participants will note the following benefits. Impact If these benefits to the participants are achieved, then certain changes might occur. Faculty: J. Saxe, M. Dulay, B. O’Brien and R. Shunk MedEdPortal Staff UCSF Ed Tech Staff Interprofessional Funds for IT support -Delineation of project goals, objectives and work plan -Define roles and responsibilities of faculty -Delineate detailed timeline -Design online curriculum -Identify resources to share with participants --Design online training opportunities for participants -Mutual understanding of goals and objectives -Clarity about roles and responsibilities -Defined process for decision-making and for assuring deliverables -Well-designed curriculum -Detailed list relevant resources needed for teaching trainees -Enriched train-the trainer experiences for clinical faculty teaching CQI & PS in primary care settings -Training materials that support satisfying CQI &PS clinical experiences for teams of interprofessional learners at primary care training sites -Faculty and preceptors prepared to provide and evaluate interprofessional CQI & PS didactic and clinical experiences especially for older adults to our learners. -Sustained educational and clinical training models that support CQI &PS interprofessional education -Prepared workforce to improve processed and outcomes of care Learning Objectives IP faculty and mentors will: 1. Demonstrate an increase in knowledge, skills, and confidence in teaching CQI concepts and mentoring CQI projects including identifying topics for improvement 2. Plan, implement, and evaluate their own CQI- PS curriculum including assessing trainee learning 3. Develop & evaluate an e-poster presentation of desired curriculum or project Educational Design and Strategies Knowledge • IHI Open school modules • Lean Training • Faculty Leads will teach key improvement tools by using a case study Problem, Aim Microsystems Analysis – Current Process & Fishbone Test of Change – PDSA cycle Educational Design and Strategies Skills • CQI project listed above • Coaching • Presentation of projects Including aim, microsystems analysis, etc. Attitudes • Have faculty attend Lean training Huddle Improvement Board Educational Design and Strategies Module Module Objectives Teaching/Learning Strategy Assessment Strategy Responsible Person (s) CQI Planning Stage: Part 2 Learning objective -Use Model for Improvement resources and tools to assist trainees in selecting and addressing an area for improvement Performance objectives -Write an aim statement -Complete a microsystems analysis -Describe a test of change Participant objective -Identify the deliverables to expect from trainee teams at the end of the planning stage Satisfaction objective -Apply Model for Improvement resources and tools to the case study and a selfidentified quality improvement challenge -Lecture (15 minutes) -Case study Quiz: Aim statements Try it on exercise: Complete a PDSA Cycle for your QI concern M. Dulay J. Saxe Learner Assessment Faculty- Knowledge 1. Pre- assessment of knowledge, skills and attitudes related to CQI 2. Critical reflection: Identify a problem in the participants clinical setting that would benefit from trainee involvement. 3. Review/ critique Root Cause analysis or QI steps for the case and/or the participant’s QI project 4. Quiz 5. Critical Analysis of an eposter Program Evaluation 1. Faculty Outcomes a. Satisfaction b. Skill 2. Trainee Outcomes a. Knowledge b. Satisfaction c. Skill 3. Patient Outcomes 4. Organizational Outcomes Summary of progress to date 1. Logic Model 2. Course Outline 3. Case Study 4. Determining general format for lecture/content 5. Creating Timeline for video- taping Barriers/challenges 1. Time 2. Time 3. Time Timeline • Curriculum be implemented in the fall 2015 Next steps • • • Case Study Determining general format for lecture/content Creating Timeline for video- taping Dissemination Plan and Additional Activities • MedEd Portal submission • Interprofessional academic patient aligned care team (iaPACT) working group • Interprofessional Conferences