Generalidades del cáncer de pulmón
advertisement
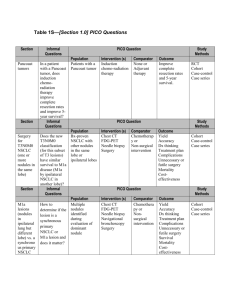
Lung Cancer Genotyping in Colombia Mauricio Lema Medina MD Clínica de Oncología Astorga Medellín Acknowledgments Dr. Andrés Felipe Cardona Zorrilla M.D Globocan, 2008 Registro Poblacional de Cáncer, Cali – Colombia Registro Poblacional de Cáncer, Antioquia – Colombia, 2007-2009 Registro Poblacional de Cáncer, Antioquia – Colombia, 2007-2009 Registro Poblacional de Cáncer, Antioquia – Colombia, 2007-2009 http://rpcc.univalle.edu.co/ Colombia Creado por: Mauricio Lema Medina - LemaTeachFiles© - 2010 Globocan, 2008 Cisplatin-based CT in advanced NSCLC 100 Supportive care + CT Supportive care 80 Survival (%) 60 40 Meta-Analysis Modest improvement in OS 20 0 0 6 12 18 24 Time from randomisation (months) Cisplatin-Based chemotherapy for advanced NSCLC NSCLC Collaborative Group. BMJ 1995;311:899–909 Platinum-Based Doublets in Advanced NSCLC Probabilidad de supervivencia 1.0 Cisplatin / paclitaxel Cisplatin / gemcitabine Cisplatin / docetaxel Carboplatin / paclitaxel 0.8 0.6 0.4 0.2 0.0 0 5 10 15 20 25 30 Meses ECOG trial 1594 ECOG, Eastern Cooperative Oncology Group Schiller et al. N Engl J Med 346:92, 2002 Schiller, et al. NEJM 2002 NSCLC Outcomes in Bogotá, Colombia n=345 n=176 Stage IIIB / IV NSCLC Received anti cancer agents Male 64% PS 0/1 45% Adeno 60% Squamous 24% Weight loss 61.5% 1st Line therapy Platinum-doublets 71% Gem/Vin mono 19% Erlotinib 4.5% Cardona AF. Rev Venez Oncol 2010; 22(1):66-83 NSCLC Outcomes in Bogotá, Colombia PFS Cisplatin: 4.7 m Carboplatin: 3.2 m OS Median: 9.2 m 1-yr OS: 26% 3.4 Cardona AF. Rev Venez Oncol 2010; 22(1):66-83 Molecular subtypes of lung carcinoma Recently described LKB1 MEK1 ROS fusion gene EGFR PDGFR amp ERK BIM MET Lung cancer 2010 – USA 219,000 new cases Small-cell lung cancer (13%) EGFR mutated (10% NSCLC ) Other NSCLC KRAS mutated (25% of adenocarcinoma) Yearly incidence of cancers with driver mutations KRAS-mutated NSCLC 36.000 cases/year Pao W. ASCO 2010. EGFR-mutated NSCLC 18.000 cases/year EML4-ALK NSCLC 9.000 cases/year CML 5.000 cases/year EGFR mutations around the world Overall 17% E19 62% E21 37% E20 38% Overall 14% E19 60% E21 30% E20 8% - 38% Overall 32.8% E19 54.3% E21 44.5% E20 2.2% Overall 40% - 50% E19 51% E21 42% E20 2% Overall 15.8% E19 64.3% E21 24.7% IPASS: Carboplatin + Paclitaxel vs Gefitinib in metastatic NSCLC adenocarcinoma (very low smoking burden) Adenocarcinoma, Stage IV, PS 0-2, very low smoking burden (n=1217) Carboplatin + Paclitaxel (PC) (n=608) Gefitinib (n=609) PC: Carboplatin AUC 5-6 d1 + Paclitaxel 200 mg/m2 d1. q21 days x6. Gefitinib: 250 mg vía PO qd. Crossover allowed Median OS (months) PC Gefitinib P All 17.3 18.6 NS HR for progression HR P Wild type EGFR 2.85 0.0001 Mutated EGFR 0.48 0.0001 Mok T, et al. ESMO 2008 EURTAC: CT vs Erlotinib in mEGFR NSCLC Chemotherapy (n = 87) Chemo-naive metastastic NSCLC with mEGFR (n = 173) Erlotinib 150 mg PO qd (n = 86) Primary End-Point: Overall survival. Rosell R, et al. ASCO 2011. Abstract 7503. EURTAC: Response and Safety Erlotinib (n = 86) Chemo (n = 87) • CT-treated patients had increased frequency of: 58 15 – Grade 3/4 AEs (81% vs 45%) CR 2 0 PR 56 15 Disease control rate 79 66 – Dose modification or interruption due to treatment-related AE (47% vs 23%) SD 21 51 PD 7 13 No response assessed 14 22 Response Outcome, % Objective response Rosell R, et al. ASCO 2011. Abstract 7503. – Discontinuation due to treatmentrelated AE (14% vs 5%) – Treatment-related serious AEs (16% vs 7%) Clinical Care Options. EURTAC: Erlotinib vs Chemo in EGFR Mutation-Positive, Stage IIIB/IV NSCLC • Phase III; significant benefit in PFS and with erlotinib vs chemotherapy 1.0 Erlotinib (n = 86) Chemotherapy (n = 87) PFS Probability 0.8 0.6 5.2 HR: 0.37 (95% CI: 0.25-0.54; log-rank P < .0001) 9.7 0.4 0.2 0 0 3 Patients at Risk, n Erlotinib 86 63 Chemo 87 49 6 9 12 15 18 21 24 27 30 33 9 3 7 1 4 0 2 0 2 0 0 0 Mos 54 20 32 8 21 5 17 4 Rosell R, et al. ASCO 2011. Abstract 7503. Reprinted with permission. Clinical Care Options. EURTAC: OS and PFS Across Patient Subgroups • • No significant difference in OS at interim analysis; data immature with high rate of crossover (HR = 0.80; 95% CI: 0.47-1.37; P = .4170) No PFS benefit of erlotinib vs chemotherapy among former smokers HR (95% CI) 0.37 (0.25-0.54) 0.44 (0.25-0.75) 0.28 (0.16-0.51) 0.38 (0.17-0.84) 0.35 (0.22-0.55) 0.26 (0.12-0.59) 0.37 (0.22-0.62) 0.48 (0.15-1.48) 0.56 (0.15-2.15) 1.05 (0.40-2.74) 0.24 (0.15-0.39) 0.30 (0.18-0.50) 0.55 (0.29-1.02) All < 65 yrs ≥ 65 yrs Male Female PS 0 PS 1 PS 2 Current smoker Former smoker Never smoker Exon 19 deletion L858R mutation 0.1 0.2 0.4 0.6 0.8 1.0 1.5 2.0 Favors Erlotinib Rosell R, et al. ASCO 2011. Abstract 7503. HR n 173 85 88 47 126 57 92 24 19 34 120 115 58 4.0 Favors Chemotherapy Clinical Care Options. Study design Between subjects factorial design Target population Colombia incident cases of LAC EGFR+ Accesible population LAC cases analized in a centralized laboratory 10 BRAF KRAS/EGFRWt 20 Study sample LAC cases with complete genotipification 10 Random allocation Control Her2 KRAS+ PI3K Main objective •To establish the frequency of driver mutations in NSCLC in LATAM population. Methods •Direct sequencing in patients from Argentina, Colombia, Mexico, and Peru was performed at each site. Measurement of clinical outcomes Alk Main study schedule - Colombia Test for ALK/ELM4 Translocation + N=1 N=26 Test BRAF - Test Her2 - N=322 Test for KRAS mutation N=205 Test for EGFR mutation N=322 N=80 No further molecular testing + N=1 N=36 Test PI3k + N=20 N=35 No further molecular testing + N=0 N=60 N=170 N=242 + Patients with available data concerning the use of erlotinib (N=41) + N=1 Main characteristics of EGFR mutant population Variable Number of pts treated with erlotinib (follow-up available data) Mean age (SD) Stratified age >65 yrs <65 yrs ND Sex Male Female Tobacco exposure Never smoker Former smoker Current smoker Main metastasis (site) Pleuropulmonary Brain Liver Bone ND N (%) 41 (51%) 63 yrs (±12) 13 (31.7) 24 (58.5) 4 (9.8) 9 (22.0) 32 (78.0) 30 (73.2) 10 (24.4) 1 (2.4) 26 (63.4) 4 (9.8) 3 (7.3) 2 (4.9) 6 (14.6) Hormonal receptor status (tumor tissue) Positive Negative ND TTF1 status Positive Negative ND Mutation type delE19 L858R T790M basal Positive Negative ND Line of treatment 1 2 3 ND Response Stable disease Partial response Complete response Progressive disease ND Overall response rate Clinical benefit 22 (53.7) 11 (26.8) 8 (19.5) 22 (53.7) 11 (26.8) ND 8 (19.5) 26 (63.4) 15 (36.6) 2 (4.9) 23 (56.1) 16 (39.0) 17 (41.5) 14 (34.1) 9 (22.0) 1 (2.4) 7 (17.1) 30 (73.2) 2 (4.9) 1 (2.4) 1 (2.4) 32 (78.1) 39 (95.2) Colombia (ONCOLGroup study) Median 14.7 mo IC95% (11.8-17.6) Colombia IC95% (11.8-17.6) Survival Survival P = 0.093 México IC95% (8.8-13.1) Time (months) Time (months) Progresion free survival Cardona AF, et al. ASCO 2011. Outcomes in Latin American NSCLC patients harboring wild-type or activating mutations of EGFR (CLICaP Registry) - submitted to ASCO 2012 PFS: 13 months mEGFR (n=175) Stage IV NSCLC - CLICaP Registry (n=589) OS: 36 months RR: 70% PFS: 3 months Non-EGFR mEGFR % Female 57% Adenocarcinoma 89% Exon 19 mutations 58% L858R mutation 36% (n=414) PFS: 14 months RR: 29% Arrieta O, Cardona AF, Bramuglia G, Campos AD, Becerra H, Martín C, Richardet E, Serrano S, Y powazniak, Rosell R, on behalf of the CLICaP. Main study schedule - Colombia Test for ALK/ELM4 Translocation + N=1 N=26 Test BRAF - Test Her2 - N=322 Test for KRAS mutation N=205 Test for EGFR mutation N=322 N=80 No further molecular testing + N=1 N=36 Test PI3k + N=20 N=35 No further molecular testing + N=0 N=60 N=170 N=242 + Patients with available data concerning the use of erlotinib (N=41) + N=1 ALK/ELM4 Juxtaposed the 5’ end of the EML4 gene with the 3’end of the ALK gene MET Cytoplasmic Fusion Variants of ALK ALK b a SEMA Extracellular TM TM Extracellular TM TM P Intracellular Kinase Kinase Intracellular YY YY P P Kinase YY YYP YY P P YYP P P YY P YYP P P YY YY YYP YY NPM-ALK YY P YY Soda S, et al. Nature 2007.; Perner, et al. Neoplasia 2009.; Soda S, et al. PNAS 2008. P Kinase YY P YY YYP P YY EML4-ALK ALK/EML4 mutation around the world 4.2% 8.0% 2.7% 3.7% J Clin Oncol 2009;27:4232–4235. J Thorac Oncol .2009;4:1450-1454. Tumor responses to crizotinib by patient PROFILE 10011 PROFILE 10052 Median time to response: 8 wk 30 1. Camidge et al., ASCO 2011; Abs #2501. 2. Riely et al., IASLC 2011; Abs #O31.05. Survival in ALK-positive NSCLC with crizotinib versus crizotinib-naive controls WT/WT Control (n=125) ALK Crizotinib ALK Control (n=30) (n=23) 100% 80% Median Survival, mo NR 6 11 1-yr Survival, % 70 44 47 2-yr Survival, % 55 12 32 60% From 2nd/3rd line crizotinib HR = 0.49, p=0.02 40% 20% 0% 0 31 1 2 3 4 Overall survival (years) Shaw et al., ASCO 2011; Abs #7507. Adenocarcinoma de pulmón en mujer no fumadora T3N2(multinivel)M1(hueso) G2LxVx ALK/EML4+ NSCLC NPA (Female/53 yo) Lung adenocarcinomaT3N2(multilevel)M1(bone) G2LxVx Stage IV EGFR 19 - L858R - T790M basal Wt/BCRA1 (T1)/RAP80 (T1)/ERCC1 (bajos niveles)/NKX2 (T1)/ ALK/ELM4 (V1+) 8 months 14 months Diagnosis 24.10.09 1st line Cis/Pem x 6 cycles 02.12.09 d OS 3 months OS 2.4 years Manteinance Pem x 4 cycles 27.05.10 2nd line CBP/Gem/Bev 21.07.10 Manteinance Bev x 13 cycles 27.05.10 3rd line Doc x 3 cycles 03.07.11 PD 14.06.11 (Pleural) PD 22.08.11 (Pericardial) + RT 6.000 cGy PD 25.06.10 (one lesion brain) Radiosurgery 02.07.10 4th line Crizo x 1 cycles 13.10.11 NSCLC in Colombia Relatively low incidence compared to other countries: 15/100.000 High letality Other mutations ALK/EML4 and others have been found They hold the promise of individualized care Outcomes with CT At first glance (and with very limited data): Similar to other countries EGFR mutations In mEGFR enriched samples: 32% PFS/OS with 1st-line anti EGFR TKI appear to be non-inferior to other cohorts When should we perform genotyping in NSCLC? SCENE 4 Different sub-types of NSCLC Never At progression EGF/ALK Mutation At diagnosis When should we perform genotyping in NSCLC Different sub-types of NSCLC Never At progression EGFR/ALK Mutations At diagnosis When should we perform genotyping in NSCLC Different sub-types of NSCLC Never... Never All patients are candidates to anti-EGFR therapy 1st Line (EURTAC) Maintenance (Saturn-trial) 2nd / 3rd Line (BR.21) No proven increase in OS with 1st Line TKI in mEGFR Likelihood of driver mutations other than EGFR, low No anti ALK/EML4 therapy in Colombia (at this time) When should we perform genotyping in NSCLC? Different sub-types of NSCLC. Post-progression Progression After chemotherapy progression To define anti EGFR vs 2nd Line Chemotherapy To identify other driver mutations (ie, ALK+ NSCLC) Not supported by clinical evidence May be reasonable Whom? All EGFR/ALK enriched populations? When should we perform genotyping in NSCLC? Different sub-types of NSCLC. At diagnosis Diagnosis In mEGFR patients may delay Chemotherapy initiation No benefit in OS for mEGFR (non-asiatic) patients with 1st Line TKIs May help identify other driver mutations (ie, ALK+) But, should we treat those 1st or after conventional Rx? Whom? Restrict to non/light-smokers with adenocarcinoma?