Antimicrobial Agents
advertisement

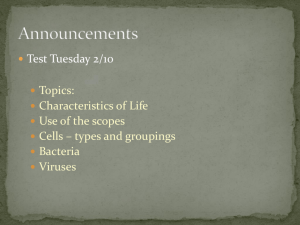
Antimicrobial Agents Prof. Khaled H. Abu-Elteen What is an Antibiotic? • An antibiotic is a selective poison. • It has been chosen so that it will kill the desired bacteria, but not the cells in your body. Each different type of antibiotic affects different bacteria in different ways. • For example, an antibiotic might inhibit a bacteria's ability to turn glucose into energy, or the bacteria's ability to construct its cell wall. Therefore the bacteria dies instead of reproducing. Antibiotics • Substances produced by various species of microorganisms: bacteria, fungi, actinomycetes- to suppress the growth of other microorganisms and to destroy them. Today the term antibiotics extends to include synthetic antibacterial agents: sulfonamides and quinolones. Where do antibiotics come from? • Several species of fungi including Penicillium and Cephalosporium • E.g. penicillin, cephalosporin – Species of actinomycetes, Gram positive filamentous bacteria • Many from species of Streptomyces – Also from Bacillus, Gram positive spore formers – A few from myxobacteria, Gram negative bacteria – New sources explored: plants, herps, fish Selective toxicity • The more distantly related the invader, the more targets available for the drug to hit – The less likelihood of direct toxic effects. • Prokaryotes biochemically least similar • Fungi and Protozoa are eukaryotes, so more closely related to humans. • Helminths (worms) also animals • Viruses use our own cell machinery • Cancer cells ARE our cells. History of Antimicrobial Therapy • 1909 Paul Ehrlich – Differential staining of tissue, bacteria – Search for magic bullet that would attack bacterial structures, not ours. – Developed salvarsan, used against syphilis. • 1929 Penicillin discovered by Alexander Fleming • 1940 Florey and Chain mass produce penicillin for war time use, becomes available to the public. • 1935 Sulfa drugs discovered • 1944 Streptomycin discovered by Waksman from Streptomyces griseus Sir Alexander Fleming Fleming’s Petri Dish Historical distinctions • Antibiotics: substances produced by organisms that have inhibitory effects on other organisms. – Penicillin, streptomycin • Synthetic drugs: produced in a lab. – Salvarsan, sulfa drugs • Nowadays, most antimicrobials are semisynthetic – Distinction between “antibiotics” and “synthetic drugs” slowly being abandoned. Selective toxicity means safer for host • Antibiotics generally have a low MIC – Minimum inhibitory concentration – Effective at lower doses • Good therapeutic index ( Ti) – Safer; larger quantity must be administered before harmful side effects occur. e.g. Ti = LD50 / ED50 Where LD = lethal dose ED = effective dose Bacteriostatic vs. Bactericidal • Antibiotics differ by mode of action • Bacteriostatic compounds inhibit the growth of bacteria – Holds invaders in check; host immune system does the killing • Bactericidal compounds directly kill the bacteria • Location and severity of infection affect choice of antibiotic – E.g. CNS infection calls for bactericidal treatment. VI. Antibacterial Agents • • • • • • • • • • • • • • • • • • • • • • A. Inhibitors of cell wall synthesis 1. Penicillins 2. Cephalosporins 3. Other antibacterial agents that act on cell walls B. Disrupters of cell membranes 1. Polymyxins 2. Tyrocidins C. Inhibitors of protein synthesis 1. Aminoglycosides 2. Tetracyclines 3. Chloramphenicol 4. Other antibacterial agents that affect protein synthesis a. Macrolides b. Lincosamides D. Inhibitors of nucleic acid synthesis 1. Rifampin 2. Quinolones E. Antimetabolites and other antibacterial agents 1. Sulfonamides 2. Isoniazid 3. Ethambutol 4. Nitrofurans Antibiotic Mechanisms of Action Alteration of Cell Membrane Polymyxins Bacitracin Neomycin Transcription Translation Translation Review and Overview of Bacterial Targets • Bacterial cell walls – Except for Mycoplasma and relatives, all bacteria of the Domain Eubacteria possess peptidoglycan – Peptidoglycan provides shape and structural support to bacterial cells – Bacterial cytoplasm is generally hypertonic compared to their environment • Net flow of water: into cell • Wall under high osmotic pressure Cell walls continued • Chemical structure of peptidoglycan contributes to its function – Polysaccharide chains composed of 2 alternating sugars, N-acetylglucosamine (NAG) and N-acetylmuramic acid (NAM) – Cross-linked in 3 dimensions with amino acid chains – A breach in peptidoglycan endangers the bacterium Peptidoglycan Molecule Cross links are both horizontal and vertical between glycan chains stacked atop one another. There is no molecule similar to peptidoglycan in humans, making drugs that target cell wall synthesis very selective in their toxicity against bacteria. Gram positive & Gram Negative • Gram positive bacteria have a thick cell wall – Peptidoglycan directly accessible from environment • Gram negative bacteria have a different wall – Thin layer of peptidoglycan – Surrounded by an outer membrane composed of lipopolysaccharide, phospholipids, and proteins – Outer membrane is a barrier to diffusion of molecules including many antibiotics • Some hydrophobic antibiotics may diffuse in. • Porins allow passage of only some antibiotics Gram negative cell structure 1-Inhibition of cell wall synthesis • beta-lactam containing antibiotics inhibit transpeptidase; bacteria cannot synthesize reinforced cell wall and they lyse when they try to grow • Vancomycin and cyclo-Ser inhibit specific binding of Ala’s in crossbridges to transpeptidase in many gram+ bacteria • Bacitracin inhibits secretion of NAG and NAM subunits • All of these only kill growing bacteria Cell wall synthesis inhibitors Penicillins • Penicillins contain a b-lactam ring which inhibits the formation of peptidoglycan crosslinks in bacterial cell walls (especially in Gram-possitive organisms) • Penicillins are bactericidal but can act only on dividing cells • They are not toxic to animal cells which have no cell wall Synthesis of Penicillin b-Lactams produced by fungi, some ascomycetes, and several actinomycete bacteria b-Lactams are synthesized from amino acids valine and cysteine b Lactam Basic Structure Penicillins Clinical Pharmacokinetics • Penicillins are poorly lipid soluble and do not cross the blood-brain barrier in appreciable concentrations unless it is inflamed (so they are effective in meningitis) • They are actively excreted unchanged by the kidney, but the dose should be reduced in severe renal failure Penicillins Resistance • This is the result of production of b-lactamase enzyme in the bacteria which destroys the blactam ring • It occurs in e.g. Staphylococcus aureus, Haemophilus influenzae and Neisseria gonorrhoea Penicillins Examples • There are now a wide variety of penicillins, which may be acid labile (i.e. broken down by the stomach acid and so inactive when given orally) or acid stable, or may be narrow or broad spectrum in action Penicillins Examples • Benzylpenicillin (Penicillin G) is acid labile and b-lactamase sensitive and is given only parenterally • It is the most potent penicillin but has a relatively narrow spectrum covering Strepptococcus pyogenes, S. pneumoniae, Neisseria meningitis or N. gonorrhoeae, treponemes, Listeria, Actinomycetes, Clostridia Penicillins Examples • Phenoxymethylpenicillin (Penicillin V) is acid stable and is given orally for minor infections • it is otherwise similar to benzylpenicillin Penicillins Examples • Ampicillin is less active than benzylpenicillin against Gram-possitive bacteria but has a wider spectrum including (in addition in those above) Strept. faecalis, Haemophilus influenza, and some E. coli, Klebsiella and Proteus strains • It is acid stable, is given orally or parenterally, but is b-laclamase sensitive Penicillins Examples • Amoxycillin is similar but better absorbed orally • It is sometimes combined with clavulanic acid, which is a b-lactam with little antibacterial effect but which binds strongly to b-lactamase and blocks the action of blactamase in this way • It extends the spectrum of amoxycillin Penicillins Adverse effects • Allergy : Patient should be always asked about a history of previous exposure and adverse effects • Superinfections (e.g.caused by Candida ) • Diarrhoea : especially with ampicillin, less common with amoxycillin • Rare: haemolysis, nephritis Penicillins Drug interactions • The use of ampicillin (or other broadspectrum antibiotics) may decrease the effectiveness of oral conraceptives by diminishing enterohepatic circulation Cephalosporins • They also owe their activity to b-lactam ring and are bactericidal. • Produced from a fungus Cephalosporium acremonium. • Good alternatives to penicillins when a broad spectrum drug is required • should not be used as first choice unless the organism is known to be sensitive Cephalosporins • BACTERICIDAL- modify cell wall synthesis • Interfere at the final step of peptidoglycan synthesis ( Transpeptidation) • CLASSIFICATION- first generation are early compounds • Second generation- resistant to β-lactamases • Third generation- resistant to β-lactamases & increased spectrum of activity • Fourth generation- increased spectrum of activity Cephalosporins • FIRST GENERATION- eg cefadroxil, cefalexin, Cefadrine - most active vs gram +ve cocci. An alternative to penicillins for staph and strep infections; useful in UTIs • SECOND GENERATION- eg cefaclor and cefuroxime. Active vs enerobacteriaceae eg E. coli, Klebsiella spp,proteus spp. May be active vs H influenzae and N meningtidis Cephalosporins • THIRD GENERATION- eg cefixime and other I.V.s cefotaxime,ceftriaxone,ceftazidine. Very broad spectrum of activity inc gram -ve rods, less activity vs gram +ve organisms. • FOURTH GENERATION- cefpirome better vs gram +ve than 3rd generation. Also better vs gram -ve esp enterobacteriaceae & pseudomonas aerugenosa. I.V. route only Cephalosporins Adverse effects • Allergy (10-20% of patients with penicillin allergy are also allergic to cephalosporins) • Nephritis and acute renal failure • Thrombophlebitis • Superinfections • Gastrointestinal upsets when given orally Vancomycin • This interferes with bacterial cell wall formation and is not absorbed after oral administration and must be given parenterally. • It is excreted by the kidney. • It is used i.v. to treat serious or resistant Staph. aureus infections and for prophylaxis of endocarditis in penicillin-allergic people. Vancomycin Adverse effects • Its toxicity is similar to aminoglycoside and likewise monitoring of plasma concentrations is essential. • Nephrotoxicity • Allergy 2- Inhibition of protein synthesis • Aminoglycosides (bactericidal): streptomycin, kanamycin, gentamicin, tobramycin, amikacin, netilmicin, neomycin • Macrolides • Chloramphenicol, Lincomycin, Clindamycin (bacteriostatic) Protein synthesis inhibitors • Need to affect bacteria, not mitochondria • Aminoglycosides (streptomycin, gentamicin) change shape of 30S ribosome subunit • Tetracycline blocks access to A site of 30S subunit • Chloramphenicol block peptide bond formation from 50S subunit • Macrolides (erythromycin) block 50S subunit action • Antisense NAs bind to beginning of mRNA and block translation Protein synthesis inhibitors Ribosomes: site of protein synthesis • Prokaryotic ribosomes are 70S; – Large subunit: 50 S • 33 polypeptides, 5S RNA, 23 S RNA – Small subunit: 30 S • 21 polypeptides, 16S RNA • Eukaryotic are 80S Large subunit: 60 S • 50 polypeptides, 5S, 5.8S, and 28S RNA – Small subunit: 40S • 33 polypeptides, 18S RNA Differences in structure between prokaryotic and eukaryotic ribosomes make antibiotics that target protein synthesis fairly selectively toxic against bacteria. Aminoglycosides (bactericidal) streptomycin, kanamycin, gentamicin, tobramycin, amikacin, netilmicin, neomycin (topical) • Mode of action - The aminoglycosides irreversibly bind to the 16S ribosomal RNA and freeze the 30S initiation complex (30S-mRNAtRNA) so that no further initiation can occur. They also slow down protein synthesis that has already initiated and induce misreading of the mRNA. By binding to the 16 S r-RNA the aminoglycosides increase the affinity of the A site for t-RNA regardless of the anticodon specificity. May also destabilize bacterial membranes. • Spectrum of Activity -Many gram-negative and some gram-positive bacteria • Resistance - Common • Synergy - The aminoglycosides synergize with β-lactam antibiotics. The β-lactams inhibit cell wall synthesis and thereby increase the permeability of the aminoglycosides. Aminoglycosides Clinical pharmacokinetics • These are poorly lipid soluble and, therefore, not absorbed orally • Parenteral administration is required for systemic effect. • They do not enter the CNS even when the meninges are inflamed. • They are not metabolized. Aminoglycosides Clinical pharmacokinetics • They are excreted unchanged by the kidney (where high concentration may occur, perhaps causing toxic tubular demage) by glomerular filtration (no active secretion). • Their clearance is markedly reduced in renal impairment and toxic concentrations are more likely. Aminoglycosides Resistance • Resistance results from bacterial enzymes which break down aminoglycosides or to their decreased transport into the cells. Aminoglycosides Examples • Gentamicin is the most commonly used, covering Gram-negative aerobes, e.g. Enteric organisms (E.coli, Klebsiella, S. faecalis, Pseudomonas and Proteus spp.) • It is also used in antibiotic combination against Staphylococcus aureus. • It is not active against aerobic Streptococci. Aminoglycosides Examples • Tobramycin: used for pseudomonas and for some gentamicin-resistant organisms. • Some aminoglycosides,e.g. Gentamicin, may also be applied topically for local effect, e.g. In ear and eye ointments. • Neomycin is used orally for decontamination of GI tract. Aminoglycosides Adverse effects • The main adverse effects are: Nephrotoxicity Toxic to the 8th cranial nerve (ototoxic), especially the vestibular division. • Other adverse effects are not dose related, and are relatively rare, e.g. Allergies. Macrolides (bacteriostatic) erythromycin, clarithromycin, azithromycin, spiramycin • Mode of action - The macrolides inhibit translocation by binding to 50 S ribosomal subunit • Spectrum of activity - Gram-positive bacteria, Mycoplasma, Legionella (intracellular bacterias) • Resistance - Common Macrolides Examples and clinical pharmacokinetics • Erythromycin is acid labile but is given as an enterically coated tablet • It is excreted unchanged in bile and is reabsorbed lower down the gastrointestinal tract. • It may be given orally or parenterally Macrolides Examples and clinical pharmacokinetics • Macrolides are widely distributed in the body except to the brain and cerebrospinal fluid • The spectrum includes Staphylococcus aureus, Streptococcuss pyogenes, S. pneumoniae, Mycoplasma pneumoniae and Chlamydia infections. Macrolides – side effects • • • • Nauzea, vomitus Allergy Hepatitis, ototoxicity Interaction with cytochrome P450 3A4 (inhibition) Chloramphenicol, Lincomycin, Clindamycin (bacteriostatic) • Mode of action - These antimicrobials bind to the 50S ribosome and inhibit peptidyl transferase activity. • Spectrum of activity - Chloramphenicol - Broad range; Lincomycin and clindamycin - Restricted range • Resistance - Common • Adverse effects - Chloramphenicol is toxic (bone marrow suppression) but is used in the treatment of bacterial meningitis. Clindamycin • Clindamycin, although chemically distinct, is similar to erythromycin in mode of action and spectrum. • It is rapidly absorbed and penetrates most tissues well, except CNS. • It is particularly useful systematically for S. aureus (e.g.osteomyelitis as it penetrates bone well) and anaerobic infections. Clindamycin Adverse effects • Diarrhoea is common. • Superinfection with a strain of Clostridium difficile which causes serious inflammation of the large bowel (Pseudomembranous colitis) Chloramphenicol • This inhibits bacterial protein synthesis. • It is well absorbed and widely distributed , including to the CNS. • It is metabolized by glucoronidation in the liver. • Although an effective broad-spectrum antibiotics, its uses are limited by its serious toxicity. Chloramphenicol • The major indication is to treat bacterial meningitis caused by Haemophilus influenzae, or to Neisseria menigitidis or if organism is unknown.It is also specially used for Rikettsia (typhus). Chloramphenicol Adverse effects • A rare anemia, probably immunological in origin but often fatal • Reversible bone marrow depression caused by its effect on protein synthesis in humans • Liver enzyme inhibition Tetracyclines (bacteriostatic) tetracycline, minocycline and doxycycline • Mode of action - The tetracyclines reversibly bind to the 30S ribosome and inhibit binding of aminoacyl-t-RNA to the acceptor site on the 70S ribosome. • Spectrum of activity - Broad spectrum; Useful against intracellular bacteria • Resistance - Common • Adverse effects - Destruction of normal intestinal flora resulting in increased secondary infections; staining and impairment of the structure of bone and teeth. Tetracyclines Examples and clinical pharmacokinetics • Tetracycline, oxytetracycline have short half-lives. • Doxycycline has a longer half-life and can be given once per day. • These drugs are only portly absorbed. • They bind avidly to heavy metal ions and so absorption is greatly reduced if taken with food, milk, antacids or iron tablets. Tetracyclines Examples and clinical pharmacokinetics • They should be taken at least half an hour before food. • Tetracyclines concentrate in bones and teeth. • They are excreted mostly in urine, partly in bile. • They are broad spectrum antibiotics, active against most bacteria except Proteus or Pseudomonas. • Resistance is frequent Tetracyclines Adverse effects • Gastrointestinal upsets • Superinfection • Discolouration and deformity in growing teeth and bones (contraindicated in pregnancy and in children < 12 years) • Renal impairment (should be also avoided in renal disease) 3- Metabolic inhibitors • Sulfonamides (sulfanilamide) are structural analogs of PABA, a molecule crucial for Nucleic acid synthesis • humans do not synthesize dihydropteroic acid from PABA • Trimethoprim interferes in next step DHF -> THF Mechanism of Action ANTIMETABOLITE ACTION tetrahydrofolic acid (cont’d) Sulfonamides and trimethoprim • Sulfonamides are rarely used alone today. • Trimethoprim is not chemically related but is considered here because their modes of action are complementary. Sulfonamides, Sulfones (bacteriostatic) • Mode of action - These antimicrobials are analogues of para-aminobenzoic acid and competitively inhibit formation of dihydropteroic acid. • Spectrum of activity - Broad range activity against grampositive and gram-negative bacteria; used primarily in urinary tract and Nocardia infections. • Resistance - Common • Combination therapy - The sulfonamides are used in combination with trimethoprim; this combination blocks two distinct steps in folic acid metabolism and prevents the emergence of resistant strains. Trimethoprim, Methotrexate, (bacteriostatic) • Mode of action - These antimicrobials binds to dihydrofolate reductase and inhibit formation of tetrahydrofolic acid. • Spectrum of activity - Broad range activity against grampositive and gram-negative bacteria; used primarily in urinary tract and Nocardia infections. • Resistance - Common • Combination therapy - These antimicrobials are used in combination with the sulfonamides; this combination blocks two distinct steps in folic acid metabolism and prevents the emergence of resistant strains. p-aminobenzoic acid + Pteridine Pteridine synthetase Sulfonamides Dihydropteroic acid Dihydrofolate synthetase Dihydrofolic acid Dihydrofolate reductase Trimethoprim Tetrahydrofolic acid Methionine Thymidine Purines Sulfonamides and trimethoprim Mode of action • Folate is metabolized by enzyme dihydrofolate reductase to the active tetrahydrofolic acid. • Trimethoprim inhibits this enzyme in bacteria and to a lesser degree in animal s, as the animal enzyme is far less sensitive than that in bacteria. Sulfonamides and trimethoprim Clinical pharmacokinetics • It is the drug of choice for the treatment and prevention of pneumonia caused by Pneumocystis carinii in immunosupressed patients. • Trimethoprim is increasingly used alone for urinary tract and upper respiratory tract infections, as it is less toxic than the combination and equally effective. Sulfonamides and trimethoprim Adverse effects • Gastrointestinal upsets • Less common but more serious: sulfonamides: allergy, rash, fever, renal toxicity trimethoprim: anemia, thrombocytopenia -cotrimoxazole: aplastic anemia 4-Interference with nucleic acid synthesis • Bacterial DNA is negatively supercoiled – Supercoiling is maintained by gyrase, a type II topoisomerase. – Inhibition of gyrase and type IV topoisomerase interferes with DNA replication, causes cell death – Eukaryotic topoisomerases differ in structure Quinolones (bactericidal) nalidixic acid, ciprofloxacin, ofloxacin, norfloxacin, levofloxacin, lomefloxacin, sparfloxacin • Mode of action - These antimicrobials bind to the A subunit of DNA gyrase (topoisomerase) and prevent supercoiling of DNA, thereby inhibiting DNA synthesis. • Spectrum of activity - Gram-positive cocci and urinary tract infections • Resistance - Common for nalidixic acid; developing for ciprofloxacin Mechanism of Action INHIBITION OF DNA/RNA SYNTHESIS (cont’d) Quinolones • The quinolones are effective but expensive antibiotics. • With increased use, resistance to these drugs is becoming more common. Quinolones Examples and clinical pharmacokinetics • Nalidixic acid, the first quinolone, is used as a urinary antiseptic and for lower urinary tract infections, as it has no systemic antibacterial effect. • Ciprofloxacin is a fluoroquinolone with a broad spectrum against Gram-negative bacilli and Pseudomonas, Quinolones Examples and clinical pharmacokinetics • It can be given orally or i.v. to treat a wide range of infections, including respiratory and urinary tract infections as well as more serious infections, such Salmonella. • Activity against anaerobic organism is poor and it should not be first choice for respiratory tract infections. Quinolones Adverse effects • Gastrointestinal upsets • Fluoroquinolones may block the inhibitory neurotransmitter, and this may cause confusion in the elderly and lower the fitting threshold. • Allergy and anaphylaxis Quinolones Adverse effects • Possibly damage to growing cartilage: not recommended for pregnant women and children Metronidazole • Metronidazole binds to DNA and blocks replication. Pharmacokinetics • It is well absorbed after oral or rectal administration and can be also given i.v. • It is widely distributed in the body (including into abscess cavities) • It is metabolized by the liver. Metronidazole Uses • Metronidazole is active against anaerobic organisms (e.g. Bacteroides, Clostridia), which are encountered particularly in abdominal surgery. • It is also used against Trichomonas, Giardia and Entamoeba infections. Metronidazole Uses • Increasingly, it is used as part of treatment of Helicobacter pyloris infestion of the stomach and duodenum associated with peptic ulcer disease. • It is used also to treat a variety of dental infections, particularly dental abscess. Metronidazole Adverse effects • Nausea, anorexia and metallic taste • Ataxia • In patients, who drink alcohol, may occur unpleasant reactions. They should be advised not to drink alcohol during a treatment. Nitrofurantoin • This is used as a urinary antiseptic and to treat Gram-negative infections in the lower urinary tract. It is also used against Trypanosoma infections. • It is taken orally and is well absorbed and is excreted unchanged in the urine. Nitrofurantoin Adverse effects • Gastrointestinal upsets • Allergy • Polyneuritis Fucidin • Fucidin is active only against Staphylococcus aureus (by inhibiting bacterial protein synthesis) and is not affected b-lactamase. • It is usually only used with flucloxacillin to reduce the development of resistance. • It is well absorbed and widely distributed, including to bone • It can be given orally or parenterally. • It is metabolized in the liver. Antibiotics for leprosy • Leprosy is caused by infection with Mycobacteria leprae. • A mixture of drugs are used to treat leprosy, depending on the type and severity of the infection and the local resistance patterns. Antibiotics for leprosy • Rifampicin is used, which is related to the sulphoamides. • Rifampicin and Rifamycin block synthesis of m-RNA. • Its adverse effects include haemolysis, gastrointestinal upsets and rashes. 5- Cell membranes as targets • Bacterial cell membranes are essentially the same in structure as those of eukaryotes – Antibiotics also affect Gram neg. cell walls, ie. Outer membrane together with cell membrane – Anti-membrane drugs are less selectively toxic than other antibiotics. – Many antifungal drugs ( Polyenes as Amphotericin B, Nystatin) make use of cell membrane differences. Cell membrane disruptors • Amphotericin B binds to ergosterol of cell membranes of fungi, causing lysis of cell • Azoles (fluconazole) and allyamines (turbinafine) block ergosterol synthesis • Polymixin disrupts bacterial cell membranes, but is toxic to people Antibiotic resistance • Inherent: Outer membrane of Gram negative bacteria, wall-less bacteria. • Mutations: change in transport protein, ribosome, enzyme, etc. Normally harmful mutations are selected FOR in the presence of antibiotic. • Plasmids: through conjugation, genetic information allowing cell to overcome drug. Mechanisms of drug resistance • Alteration of target: active site of enzyme changes, ribosome changes. • Alteration of membrane permeability: transport protein changes, drug no longer enters; drug that does enter is actively pumped out. • Enzymatic destruction of drug: penicillinases (beta lactamases) • “End around” inhibitor: bacteria learns to use new metabolic pathway, drug no longer effective. Drug resistance • Beta- lactamase is now wide-spread and often is found on plasmids • New synthetic versions of penicillin have been developed that are not cleaved by beta-lactamase • Other resistances develop Spectrum of action of antimicrobials Spectrum • When specific testing is not done or delayed, antibiotic with a broad spectrum is administered – Broad spectrum antibiotics can penetrate Gram – outer membranes, resist inactivation, etc. – Shotgun: better chance of inhibiting pathogen • Death of normal microbiota results in overgrowth of resistant bacteria (endogenous infection; “superinfection”) or allows invasion by outside opportunists. Drug administration • Antibiotics administered oral, i.v., i.m.,i.p – Same caveats apply, i.e. acid instability, delayed absorption with food for oral – i.v. gives higher, quicker concentrations, reaches more compartments with sufficient dose quickly Combination therapy • Some valuable reasons why combination therapy is used – Synergistic effects between two drugs – Polymicrobial infections, e.g. abdominal injuries – Avoid Antagonistic effects. Chemotherapy for viruses • • • • • • • • • • • • • • • • • • • • • Antifungal Agents A. Imidazoles and triazoles B. Polyenes 1. Amphotericin B 2. Nystatin C. Griseofulvin D. Other antifungal agents 1. Flucytosine 2. Tolnaftate 3. Terbinafine Antiviral Agents A. Purine and pyrimidine analogues 1. Idoxuridine and trifluridine 2. Vidarabine 3. Ribavirin 4. Acyclovir 5. Ganciclovir 6. Zidovudine B. Amantadine C. Treatment of AIDS Antiviral drugs • Antiviral chemotherapy is still in its infancy. • Viruses are more difficult ‘targets’ than bacteria: they are most vulnerable during reproduction, but all use host cell organelles and enzymes to do this, so that antiviral compounds are often as toxic to host cells as to virus. Antiviral drugs (cont.) • Current antiviral drugs are thought to work in one of the following ways: 1- inhibition of viral ‘uncoating’ shortly after penetration into the cell; they are best for prophylaxis or very early in the disease course (e.g.amantadine) 2- interference with viral RNA synthesis and function (e.g. ribavirin) Antiviral drugs (cont.) 3- interference with DNA synthesis (e.g. cytarabine and Vidarabine) 4- inhibition of viral DNA polymerase (e.g.acyclovir, Penciclovir and gancyclovir) 5- inhibition of reverse transcriptase at retroviruses such as HIV (e.g.zidovudine, Azidothymidine(AZT)) Acyclovir Mode of action • It is active against Herpes simplex and Herpes zoster. • Acyclovir targets virus-infected cells quite specifically, and inhibit viral replication and this explains the drug`s relatively low toxicity. Acyclovir (cont.) Therapeutic uses • It is the drug of first choice for Herpes simplex and zoster infections, because of the great efficacy and lower toxicity than the alternatives. • The drug has little activity against cytomegalovirus or Epstein-Barr virus. Acyclovir (cont.) Therapeutic uses • Herpes simplex infections of skin, mucous membranes and cornea • Life-threatening Herpes simplex infections; acyclovir i.v. reduces mortality • Herpes zoster that is less sensitive to acyclovir than H. simplex .It is used for early topic or oral treatment of zoster. Zidovudine (AZT) Mode of action • HIV virus is an RNA virus capable of including the synthesis of a DNA transcript of its genome, which can then become integrated into the host cell`s DNA, thereby allowing viral replication. • Synthesis of the initial DNA transcript involves the enzyme reverse transcriptase. • Zidovudine is a potent inhibitor of reverse transcriptase. Purine and pyrimidine analogues Mode of action • These drugs are effective against DNA viruses • The compounds structurally resemble purine and pyrimidine nucleosides • The resulting DNA molecule is more easily fragmented, leading to transcription errors. • They also inhibit viral DNA polymerase. Purine and pyrimidine analogues Examples and clinical pharmacokinetics • Idoxuridine: it is not absorbed from the gut, and is used topically • Vidarabine: cannot be given orally because it is metabolized in the gut - it is usually given i.v. or topically Purine and pyrimidine analogues Therapeutic uses • Idoxuridine: may be used topically for Herpes simplex and zoster but is too toxic for systemic use and has largely been supplanted by aciclovir • Vidarabine: may be used for lifethreatening systemic Herpes infections Zone of Inhibition • Around the fungal colony is a clear zone where no bacteria are growing • Zone of inhibition due to the diffusion of a substance with antibiotic properties from the fungus Susceptibility vs. Resistance of microorganisms to Antimicrobial Agents • Success of therapeutic outcome depends on: • Achieving concentration of ATB at the site of infection that is sufficient to inhibit bacterial growth. • Host defenses impaired- bactericidal agents • Complete ATB-mediated killing is necessary Susceptibility vs. Resistance (cont.) • Dose of drug has to be sufficient to produce effect inhibit or kill the microorganism: • However concentration of the drug must remain below those that are toxic to human cells – • If can be achieved – microorganism susceptible to the ATB • If effective concentration is higher than toxicmicroorganism is resistant Susceptibility Tests 1. Broth dilution - MIC test 2. Agar dilution - MIC test Minimal Inhibitory Concentration (MIC) vs. Minimal Bactericidal Concentration (MBC) 32 ug/ml 16 ug/ml 8 ug/ml Sub-culture to agar medium 4 ug/ml 2 ug/ml 1 ug/ml MIC = 8 ug/ml MBC = 16 ug/ml Susceptibility Tests (cont’d) 3. Agar diffusion Kirby-Bauer Disk Diffusion Test Susceptibility Tests “Kirby-Bauer Disk-plate test” Diffusion depends upon: 1. 2. 3. 4. 5. Concentration Molecular weight Water solubility pH and ionization Binding to agar (cont’d) Susceptibility Tests “Kirby-Bauer Disk-plate test” (cont’d) Zones of Inhibition (~ antimicrobial activity) depend upon: 1. pH of environment 2. Media components – 3. 4. 5. 6. Agar depth, nutrients Stability of drug Size of inoculum Length of incubation Metabolic activity of organisms Antibiotic Susceptibility Testing Disk Diffusion Test Determination of MIC Str Tet 8 4 2 1 Tetracycline (μg/ml) MIC = 2 μg/ml 0 Ery Chl Amp Resistance (cont.) • Bacteria produce enzymes at or within the cell surface –inactivate drug • Bacteria possess impermeable cell membrane prevent influx of drug. • Transport mechanism for certain drug is energy dependent- not effective in anaerobic environment. • ATB as organic acids penetration is pH – dependent.