Slide - community360.net
advertisement

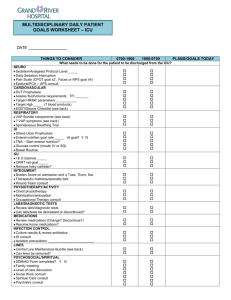
Pre-Mortems and Action Plans VAP Coaching Call January 3, 2013 1 Objectives • Share key responses and considerations from pre-mortems • Share key components and unique ideas from action plans • Discussion • Next Steps 2 Pre-Mortems A select summary of key responses and considerations 3 Pre-Mortem • Step 1 – Imagine we are 2 years in the future. Things have gone completely wrong. What could have caused this? • Step 2 – Generate a list of all the reasons failure occurred. • Step 3 – Address the 2 or 3 items of greatest concern and list what you will do differently now that you have considered them. 4 Leadership and Staff Involvement Bedside staff not involved in the decision‐making process/overwhelmed by competing initiatives: My unit started a CUSP team when our hospital joined On the CUSP: Stop BSI. Perhaps it is because we were so focused on a single problem that we never quite focused on the real mission of “CUSP”. It is not a disjointed approach to individual initiatives! It is a way of life! And so we will backtrack a bit to renew our staff’s commitment to CUSP. We will return to our roots by administering the two‐question safety survey: how will the next patient be harmed, and what would you do to prevent that harm. The survey will be distributed at our December staff meeting with a “New Years Resolution” theme. Then, we will choose two of the most commonly reported safety concerns (one that is an easier fix/low hanging fruit and another that is more complex/higher branch) and work on these concerns together. By using CUSP in this way, staff will feel more ownership of the CUSP process rather than see it as “one more thing to do”. Competition for resources with Hospital Engagement Network (HEN), which is running a huge project on the same spinal cord injury unit. Problems with pressure ulcers appear to be much more pressing than our current VAP issues. We have not had much difficulty with VAPs historically, so the urgency of this project is difficult to sell. Need to use executive sponsor to bring some focus to bear on this project and emphasize the importance of preserving the health of our most frail patients with SCI by using appropriate measures, even though a problem has not been identified. Failure to obtain leadership buy-in (i.e. lack of leadership support, leadership defined as: Nurse Manager and Director, CNO, President, All MDs, and the Hospital Board of Directors.) Educate the leadership team regarding collaborative: importance, impact on finances/pt satisfaction/readmission. Provide hospital CME on VAP. Plan a yearly house wide kick-off. None of the identified “leaders” for this project has taken the lead in any way. Work with VAP team leaders to help them understand their roles, now that project is underway. 5 If these leaders are over-committed at this time, identify new champions for this project. •BUILD the TEAM’S CAPACITY to adapt to new technology or clinical evidence •Re-focus unit by administering the 2 question safety assessment – staff select 2 high priorities areas to work on •Use of unit-based “CUSP” team •EDUCATE LEADERSHIP on VAP effort, benefits of participation •Offer CME for VAP education •Define ROLE and expectations of LEADERSHIP Leadership and Staff Involvement Lack of staff support of VAP initiatives. Educate staff on the impact of VAP on patient outcomes, costs, length of stay and how this relates back to the staff individually and as a whole organization. Ensure staff are knowledgeable regarding Total Patient Revenue (TPR) and how HAIs impact costs and overall budgets. Raise awareness and accountability by in-depth case review of each VAP occurrence at the frontline staff level. These cases will be reviewed with individual staff, at unit staff meetings and at VAP team meetings. Build on the solid base of staff awareness of the CUSP team processes and the positive results from the CUSP teams that have experience with CLABSI and CAUTI. Convey the support received from administration, including the CNE and CMP, to all levels of the CUSP team members. Preventing HAI including VAP is a strategic goal for the Board of Directors with outcomes and rates shared with all members. Lack of staff engagement Include staff in data collection. Invite staff to CUSP: Eliminate VAP meetings. Make the project fun - create a competition or contest. Perform root cause analysis on all VAE patients so staff can place a name with a number. Education/Staff involvement – Staff must be made aware of the problem and its impact on patient safety; with increased risk of mortality, increased LOS, ventilator days and cost of care. Monthly Breakfast Clubs (Multidisciplinary Team). Grassroots Committee/sub committee to review cases by case VAE’s; present findings to front-line staff. Provide updates and strategies to staff that may be working at other facilities. Monthly Unit Dashboards. Full orientation of duties and expectations of new staff. •BUILD the TEAM’S CAPACITY to adapt to new technology or clinical evidence •Invite staff to unit CUSP-VAP meetings •Include staff in data collection •EDUCATE STAFF •Healthcare payment and reform •Impact of HAI’s, VAP •In-depth VAP case review •Reinforce the positive results with CLABSI, CAUTI •Convey administrative support 6 Leadership and Staff Involvement, continued Staff Activities •PROMOTE “TEAM” & improved work relations Bi-monthly dinners outside of work. Organized lunches at work with varying themes. •Bi-monthly dinners Participate in organized activities together such as (5-10Ks), Susan G Komen for the Cure, Adopt a family. Staff/Unit Recognition lunches at work •Themed Perfect VAP Bundle Compliance Awards for staff (weekly, month, quarter, year). participation in thank organized activities •Promote Individual/personalized notes/cards to staff saying you. “We always do it this way”/“It’s not MY job”: My hospital started a “Wake Up and Breathe” protocol several •RECOGNIZE months ago along with aSTAFF Spontaneous Breathing Trial order set. RNs were all educated on the program, even re‐educated when necessary (as determined by audits). Because nurses were in control of the sedation on/off •VAP Bundle compliance awards switch, they knew what to expect and when to expect it. RTs were often left out of the timing decision. And so tensions developed when the thank patient was awake, •Personalized youagitated, cardsready to breathe, but the RT was busy elsewhere. It seemed like there was never the perfect time to wake up and breathe! We should address this •Wake Upmaking andsureBreathe problem by first that both sides Protocol are educated on the validity of SAT/SBT as a VAP prevention process measure. Then, both sides should be consistently represented at CUSP meetings (at this point, no RTs •Nurses driven are on our CUSP team). Finally, each day should start with the RN and RT discussing a mutually convenient schedule for weaning. The unit charge nurse will be ideally “out of the numbers” and able to step in as •Ensure multidisciplinary teamassign responsibility needed to facilitate scheduling. •Coordinate efforts to ensure success 7 Data Collection Reliable and efficient daily data collection Assure respiratory, pharmacy, and nursing understand goals of project during CCU rounds. Data collection test by Quality Dept. to model and measure efficiency. Assist in the daily process design and define responsibilities. Work with pharmacy to develop process for case reviews and identification of qualifying antibiotics. •Define DATA COLLECTION process •Define multidisciplinary team goals during rounds •Quality team “tests” data collection process Several charge nurses will be educated regarding the data collection definitions. This will allow some of the data•Engage collection to occur during dailynurses patient rounds. The Intensivists will be involved in ensuring that all charge and Intensivists components of the data collection are addressed during clinical rounds. Additional information, (Ex: oral hours ofrecord staff time weekly to care)•Implement will need to be obtained4 from the medical by thededicated nursing staff. support data collection We have arranged for an experienced ICU nurse to have four hours of dedicated time weekly to assist with data•Enlist entry. subgroup to investigate electronic data Pull acollection subgroup together to explore ways to collect the data electronically. Ask for staff ideas and input about what would be helpful to improve compliance with predetermined best •Ask staff what would increase data collection practices. compliance All data collecting tools require refinement. Listening and acting on the feedback of the staff using the document(s) when they offer suggestions of improvement 8 Communication and Education Tailor communication to fit the audience. Manage communication flow to avoid •TAILOR MESSAGE tomisinterpretation audienceof vital information. Our team will have monthly meetings to ensure our progress. We will have the assessment of resources as a •Well-defined standing agenda item. roles for team members Define each team member’s role and the expectations of their role upfront, provide an open communication •Monthly progress meetings and routine staff updates for questions/concerns and hold each team member accountable. Lack of education to new staff, orientees on VAP prevention •EDUCATION Have a “fast facts” sheet on VAP prevention added to orientee binders and included as something the •Inservice staff preceptor needs to all sign off on. Request some education on VAP be included in the mandatory core curriculum courses which all critical •NEW STAFF care orientees attend. Educate all the intensivists on the new definitions of VAE. •VAP “fast facts” Educate the ICU nurses and respiratory therapy staff on the new definitions. •Add VAP content to critical care core curriculum Lack of education •INTENSIVISTS Inservice staff. Provide 1:1 education to staff. •New VAP surveillance definitions Engage artistic staff members to create educational items such as posters, bulletin boards to spread information about the project. Include progress updates in staff meetings; ask for feedback routinely from staff; encourage improvement suggestions from staff. 9 Resources Overwhelming amount of work with limited resources, personnel, time, and funds: Utilize incentives (personalize to the interests of the staff) Meet with finance: educate regarding collaborative purpose, action plan, needs, goals, and financial impact. Continue to meet quarterly to update on progress, changes, current data, results, adjustments. Develop yearly competency to maintain new definitions and updated bundle. Include VAP in General Orientation and Agency Orientation. Update Admission Orders to include “Initiate VAP Protocol”. •Strategic PARTNERS - FINANCE •Use STAFF INCENTIVES •Develop YEARLY COMPETENCY Identify solutions that are easy to implement resulting in immediate process improvement. •Add VAP education to AGENCY ORIENTATION Non-compliance of VAP bundle and accountability Provide focused education to staff VAP regardingBUNDLE VAP bundle requirements and benefits of compliance for •Monitor and Audit COMPLIANCE patient, staff and organization. Initiate Daily Rounding Form for VAP in participating units to evaluate current practice and high risk areas •SHARED RESPONSIBILITY to target team efforts. •Vary assignments Monitor Q4Hdaily oral care and Q12H CHG oral care routinely to ensure consistent practice and increase accountability with staff. •Include “non-clinical” staff It is important that staff have a solid idea of how their compliance impacts the project. That includes when compliance is not optimal and asking for improvement suggestions from frontline staff. •High-census plans Shift Resources Decompression plan for unit based staff with a high census. Varied daily unit assignment. Debrief healthcare professionals after emotional encounters, whether with coworkers or patients. 10 Action Plans A select summary of the components of strong action plans 11 Action Plans • A good Action Plan sets the stage for achieving the goal – it maps out the work process with a detailed schedule of key activities needed to accomplish the goal (i.e., sustainability and cultural competence). 12 Structure and Layout of Action Plan Broke-down action plan into sections: tools, participation, training, supplies, and policy. Aligned specific activities with due dates and named people responsible. Indicated which activities were dependent on the completion of others. Identified back-up staff Broke-down action plan into sections, one section for each goal. Broke-down action plan into target areas: senior leadership engagement, physician engagement, staff engagement, and patient and family engagement. Results expressed as “success looks like” (e.g., Success for physician engagement looks like 90% of meetings attended by Physician Champion.) 13 SMART Goals (Specific, Measurable, Attainable, Relevant, Timebound) Participation of at least one team member in at least 80% of VAP coaching calls and webinars in order to actively participate in EVAP efforts and bring valuable information and resources back to staff. Improve HOB compliance to 95% by June 30, 2013. Improve oral care compliance to 95% by June 30, 2013. The compliance rate for performing both a daily sedation awakening trial (SAT) and a spontaneous breathing trial (SBT) will be 85%, by June 30, 2013. By June 30, 2013, the compliance rate for the subglottic ETT’s being connected to suction correctly and working properly will be 99%. In addition to stating goals, state objectives, e.g., Staff will be able to explain their role in data collection. Identification of Potential Barriers Staff does not always relate care given to VAP prevention. Sub-glottic ETTs not yet available in all sizes in the organization. Sub-glottic ETTs that are in house are not compatible with suction equipment. 14 Activities Will be holding a “mobility fair.” Handouts with the 5 steps of oral care were developed, placed into travel toothbrush kits and are being given as “free gifts” during Kick-off rounds in the unit with the CUSP Executive. Creating a test to ensure education of staff is successful. Will recognize and reward staff for participation, achieving goals, meeting target data, etc. (reward in a step-wise fashion: i.e. gift cards, all the way up to paying for an outside conference for staff who really go “above and beyond”) Will research Early Mobility protocols from other institutions for recommendations. Will compile evidence of cost savings from reducing VAP rates and implementation of Early Mobility Equipment, Subglottic-ETT and continued use of CHG oral care kits. Acquiring new chairs for the Unit to facilitate mobilization. Presentation to the Board regarding VAP: what it is, clinical impact, financial impact, expectations of team outcomes, and expectation of Board. Annual Confusion Assessment Method-ICU delirium assessment education to be implemented by October 2013. Staff education will also focus on the importance of their work (patient safety, financial benefits, pride in improvement). Regarding consistent SAT documentation, will capitalize on the parts of the process that are already occurring and organize the existing workflow so that SATs are performed and documented in a logical and consistent manner. 15 Tools and Strategies Make use of the physician engagement difficulty assessment and checklist to assist in prioritizing initiatives. Will perform audits to monitor compliance with the use of a daily goals checklist, and at beginning of night shift to make sure mouth care kits have been used. Assessment of project resources will be a standing agenda item at team meetings. Show support from Executive Sponsor by adding a comment with a signature in the family brochure. To improve Head Of Bed (HOB) compliance: will design a questionnaire which asks staff RNs to estimate HOB degree looking at pictures and attaching laminated arrows which highlight HOB to patient beds. Utilizing multiple methods for communication: live in- service, bulletin board, weekly e-bulletin and direct practice observation and feedback. “How will the next patient be harmed” and “How can it be prevented” will be asked at the end of each meeting to the staff. Conducting weekly audits to monitor progress and compliance with goals. Will complete Root Cause Analysis on any patient identified as having a VAE. When an infection occurs, will interview all staff, patient, and family for ways in which this might have occurred. Team includes finance department as a partner/stakeholder in the effort. Have included night shift staff on team. Implementing a specific time to place labeled mouth care kits in appropriate patient’s rooms (this routine builds habit) Will include CUSP and VAP initiative education in new Nurse’s orientation to the unit. Utilizing unit secretaries for daily data collection. 16 Tools and Strategies, continued Hand hygiene goal included in the action plan. Will utilize audit tool to track oral care and CHG oral care. Will conduct root cause analysis to review all cases of probable/possible VAP. Will display HOB compliance graphs with all VAP graphs in prominent locations. Identified replacements for data collectors when they are unavailable. Audits will document reasons for interruptions in oral care. 17 Patient and Family Engagement Several plans listed the creation of handouts, posters and/or other educational materials intended for patients and families, yet none of the teams suggested including a consumer in the design or review of the materials (or trialing the materials with actual patients and families on the unit to test effectiveness). We think we know what patients and families need to know, but have we ever asked them? Campaign Zero http://www.campaignzero.org/safety-checklists/ Institute for Patient- and Family-Centered Care http://www.ipfcc.org/tools/downloads-tools.html 18 Discussion • What ideas and actions are most appealing to you? Why? • What will you do with information shared today? • What does it mean to engage patients and families? • How can you include patients and families in this effort? 19 Next Steps 1. Continue Collecting Data – VAE algorithm – Daily Rounding 2. Quarterly Interview – Will be conducted regularly with team leaders throughout the effort. Interviews will take about 30 minutes. Someone will contact team leaders to arrange dates and times. 3. January 10 Content Call at 2:00 PM – Audio: 800-779-9891 – Pass code: 4757941 – Web link: https://connect.johnshopkins.edu/vaecontent01102013/ 4. Science of Safety – Be prepared to discuss how you ensured staff watched the video, how you assessed their knowledge of the message and content, and your plans to further learning in this area. 5. Staff Safety Assessment – Be prepared to discuss what harm staff identified and suggestions for preventing or minimizing the harm. 20 Questions? • Maryland Participants – Karol G. Wicker, MHS – Phone 410-540-5056 – kwicker@mhaonline.org • Pennsylvania Participants – Mary Catanzaro RN BSMT CIC – Phone 717-756-3958 – mcatanzaro@haponline.org 21