Ventilator Care Bundle
Assignment – Critical care Nursing
OUM
Dr. S.N. Silva
(MBBS)
VENTILATOR
ASSOCIATED
PNEUMONIA
AIMS AND OBJECTIVES
To present a clinical case illustrating the
problem of ventilator-associated
pneumonia (VAP)
To discuss the diagnosis and management
of VAP, along with a review of the
evidence
To highlight controversies in dealing with
VAP
CASE PRESENTATION
BB 73 M
Presented to SMH with 10/7 history of
“laryngitis”
Cough/SOB/Fever
CASE PRESENTATION
PMHx
Prostate Ca
Bilateral TKRs for OA
Hypertension
DHx
Antihypertensives
Zoladex
NKDA
CASE PRESENTATION
Initially managed on medical ward
However, deteriorated 1/7 into admission:
Tachycardia/hypotension/tachypnoea
Transferred to ICU, deteriorated further
Intubated
Ventilated. Needing high FiO2/PEEP
Inotropic support
Broad spectrum antibiotics
Over 2/52, gradual improvement. Antibiotics stopped
CASE PRESENTATION
Improving- FiO2 now 40%, PEEP 8
Tracheostomy for weaning
Then deterioration:
FiO2 60% to maintain PO2 8
Tachypnoea
Pyrexia
???
WHAT IS VAP?
Er, noone really knows
Suggested diagnostic criteria:
New CXR changes and one of:
Fever
Leukocytosis
Increasingly purulent secretions
48 hours or longer after institution of mechanical
ventilation
Confirmation by microbiological sampling
(BAL/tracheal brushings)
WHAT IS VAP?
Wide range of organisms:
Gram positive:
Gram negative:
Staph Aureus (both MSSA and MRSA)
Streptococcus
Pseudomonas
Acinetobacter
Klebsiella
Others:
Candida/Aspergillus
Viruses (rare)
WHO GETS VAP?
People being
mechanically
ventilated (Both ETT
and tracheostomy)
Risk factors:
Host
Environment
Age
Intubation
Sex
(M>F) Length of
Underlying ventilation
disease
Tube cuff pressure
state
Reintubation
(chronic
Sedation
disease,
Body postion*
conscious
level, sepsis Use of gastric
protection*
etc)
NG feeding
Unit hygiene*
WHY IS IT IMPORTANT?
We see it all the time
(27% of ICU patients)
Mortality 27-76% (!)*
WHY IS IT IMPORTANT?
WHAT SHOULD WE DO?
Identify the at risk patient
Reduce the risks
Rapidly diagnose VAP when it occurs
Treat appropriately
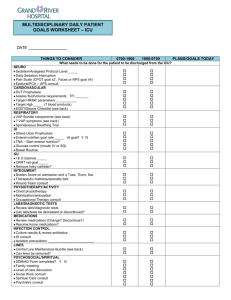
REDUCING THE RISKS
“Care bundles”
Series of intervention
grouped together as a
single one
Worked well with
central venous
catheters (“Matching
Michigan”)*
REDUCING THE RISKS
Elevation of bed 30-45 degrees*
DVT prophylaxis
Humidification
Oral hygiene/chlorhexidine mouthwash*
Gastric ulcer prophylaxis*
Appropriate ventilator tubing management
Suctioning of oropharyngeal secretions
Sedation holding/review
REDUCING THE RISKS (Extra
stuff from Europe)
Microbiological surveillance
Low nurse:patient ratio
Reduce antimicrobial prescriptions
Orotracheal tubes/orogastric tubes
Maintaining ETT cuff pressure >20cmH20
Subglottic aspiration*
Antiseptic coated ETTs*
ORAL DECONTAMINATION WITH
CHLORHEXIDINE
Simple
Cheap
Quite safe
Makes sense
SELECTIVE DIGESTIVE
DECONTAMINATION
Similar principle, but involves using oral
decontamination + NG tube antibiotics +
IV antibiotics in a variety of recipes
Same principle as above
GASTRIC ULCER PROPHYLAXIS
Reduces risk of ventilator associated
stress ulcers…
But INCREASES risk of VAP
What to do?
GASTRIC ULCER PROPHYLAXIS
“No single strategy of stress ulcer prophylaxis is
preferred when mortality is used as the outcome.
In the absence of a clinical trial demonstrating
survival benefit the individual clinician's
assumptions regarding the effect of prophylaxis
on gastrointestinal bleeding and pneumonia and
the attributable mortality of pneumonia vs.
gastrointestinal bleeding will have a significant
effect on the decision”.
RAPID DIAGNOSIS
Sensitivity 77%, specificity 42%
Other biomarkers being searched fornone yet
(Procalcitonin/CRP useful treatment
monitors, but not so useful for diagnosis)
RAPID,SPECIFIC TREATMENT
Start treatment early when suspected
Broad-spectrum antibiotic (with
antipseudomonal activity) +/aminoglycoside recommended
Assignment
Define terms
VCB – ?
VAP – OUM has done
Critically ill patient - ?
Critically
ill patient with VAP
Then…..
Discuss using VCB
Significance of using VCB
Critically Discuss VCB
Ventilator Associated Pneumonia
Multiple factors should be considered when
addressing the issues of HAP and VAP.
These factors include the following:
Whether or not to intubate the patient
The route of intubation or placement of tubes
Feeding the patient
Body positioning
Prevention of stress-related bleeding
Prevention of deep venous thrombosis
Use of antibiotics and control of colonization
http://emedicine.medscape.com/article/304836-overview
Ventilator Associated Pneumonia
Who / When/ What?
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1592694/
While critically ill patients experience a life-threatening illness, they
commonly contract ventilator-associated pneumonia. This
nosocomial infection increases morbidity and likely mortality as well
as the cost of health care. This article reviews the literature with
regard to diagnosis, treatment, and prevention. It provides
conclusions that can be implemented in practice as well as an
algorithm for the bedside clinician and also focuses on the
controversies with regard to diagnostic tools and approaches,
treatment plans, and prevention strategies.
Significance
“The application of the VAP bundle in
chronic ventilated patients resulted in a
significant reduction in the incidence of
VAP. ”
http://ccforum.com/content/12/S2/P433
Significance
“Initiation of the VAP bundle is associated
with a significantly reduced incidence of
VAP in patients in the SICU and with cost
savings.”
http://apicwv.org/docs/40.pdf
Critically?
“The ventilator bundle should be modified
and expanded to include specific
processes of care that have been
definitively demonstrated to be effective in
VAP reduction or a specific VAP bundle
created to focus on VAP prevention. ”
http://www.ncbi.nlm.nih.gov/pubmed/1927
6975
Critically ?
“Individual elements did not appear
effective; strict compliance with infection
elements was needed. Efforts to prevent VAP
may be successful in settings of high
levels of compliance with all infection-specific
elements and in settings with full-time HEs.”
http://www.cumc.columbia.edu/studies/pnice/pdf/
Pogorzelska.pdf