VAP DAILY GOALS SHEET 2009_Grand River Hospital
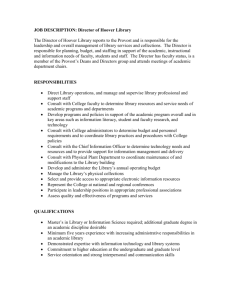
advertisement
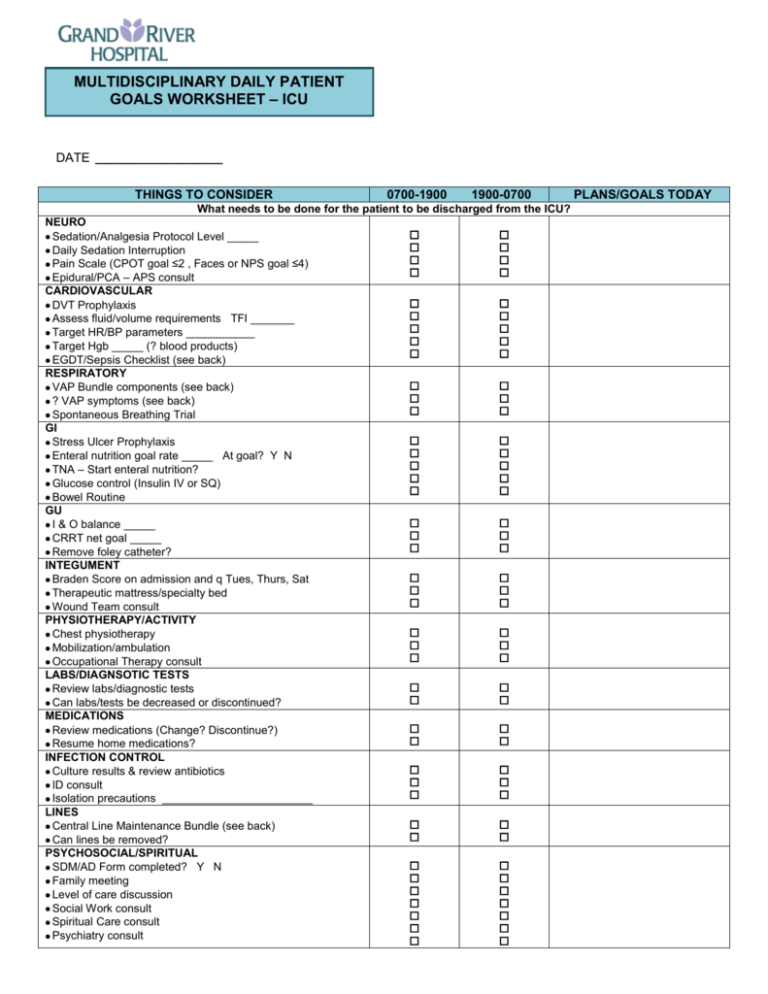
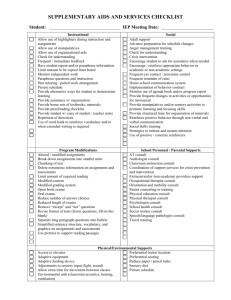
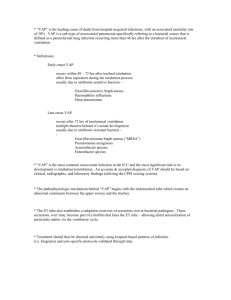
MULTIDISCIPLINARY DAILY PATIENT GOALS WORKSHEET – ICU DATE _________________ THINGS TO CONSIDER 0700-1900 1900-0700 What needs to be done for the patient to be discharged from the ICU? NEURO Sedation/Analgesia Protocol Level _____ Daily Sedation Interruption Pain Scale (CPOT goal ≤2 , Faces or NPS goal ≤4) Epidural/PCA – APS consult CARDIOVASCULAR DVT Prophylaxis Assess fluid/volume requirements TFI _______ Target HR/BP parameters ___________ Target Hgb _____ (? blood products) EGDT/Sepsis Checklist (see back) RESPIRATORY VAP Bundle components (see back) ? VAP symptoms (see back) Spontaneous Breathing Trial GI Stress Ulcer Prophylaxis Enteral nutrition goal rate _____ At goal? Y N TNA – Start enteral nutrition? Glucose control (Insulin IV or SQ) Bowel Routine GU I & O balance _____ CRRT net goal _____ Remove foley catheter? INTEGUMENT Braden Score on admission and q Tues, Thurs, Sat Therapeutic mattress/specialty bed Wound Team consult PHYSIOTHERAPY/ACTIVITY Chest physiotherapy Mobilization/ambulation Occupational Therapy consult LABS/DIAGNSOTIC TESTS Review labs/diagnostic tests Can labs/tests be decreased or discontinued? MEDICATIONS Review medications (Change? Discontinue?) Resume home medications? INFECTION CONTROL Culture results & review antibiotics ID consult Isolation precautions ________________________ LINES Central Line Maintenance Bundle (see back) Can lines be removed? PSYCHOSOCIAL/SPIRITUAL SDM/AD Form completed? Y N Family meeting Level of care discussion Social Work consult Spiritual Care consult Psychiatry consult PLANS/GOALS TODAY Ethics consult Early referral to TGLN? VAP BUNDLE COMPONENTS D N Head of bed elevated ≥ 30 degrees EVAC tube Oral versus nasal tubes Daily Sedation Interruption Assess readiness to extubate (ie. SBT) Chlorhexidine mouthwash q4h CENTRAL LINE MAINTENANCE BUNDLE D N Review of line necessity/removal Check entry site for inflammation/signs of infection Access lumens aseptically (swab with chlorhexidine) Dressing change with Tegaderm IV q7days (dated & timed) Change IV bags q24 hours (dated & timed) Change IV tubing q72 hours (dated & timed) Dedicatd lumen for TNA if applicable DOES MY PATIENT HAVE VAP? 1) Has patient been ventilated (via ETT/trach) for at least 48 hours? If yes, proceed… 2) Does the patient have ANY of the following: i) Temperature ≤36.4ºC OR ≥38.0ºC with no other recognizable cause ii) Leukopenia (WBC <4.0 x 109/L) OR leukocytosis (WBC >11.0 x 109/L) iii) If ≥70 years old, altered mental status with no other recognizable cause iv) New onset of purulent sputum, OR change in character of sputum, OR increased respiratory secretions, OR increased suctioning requirements v) Inspiratory crackles OR bronchial breath sounds on auscultation vi) Worsening gas exchange (ie. O2 desaturations OR PaO2/FiO2 <240), increased O2 requirements, OR increased minute ventilation Check if yes D N If yes to any of the above, suspect possible VAP. Consider initiation of VAP Protocol, including CPIS Score. (To be discussed with MD, NP or Pharmacist) EARLY GOAL DIRECTED THERAPY (EGDT)/SEPSIS CHECKLIST (If patient meets definition of severe sepsis or septic shock, proceed with checklist in consultation with MD) TIME INTERVENTION Check if completed 0-1 1. Consider intubation prior to overt respiratory distress. 2. Aggressive fluid resuscitation: Goals HR <100, MBP >65, or U/O >0.5 hour mL/kg/hour 3. Obtain blood, urine, sputum & patient/site-specific cultures, then initiate broad spectrum empiric antibiotics. 4. Obtain sepsis bloodwork: electrolytes, lactate, ABGs, CBC, INR/PTT, LFTs 1-8 1. Consider arterial & central IV access. hours 2. Fluid resuscitate to CVP 8-12, MBP >65, SvO2 >70% & Hct >30%. 3. Initiate vasopressor if circulatory shock persists despite adequate fluid resuscitation. 4. Initiate inotropes if SvO2 or Cardiac Index remains decreased. 5. Localize & control source of infection. 6. Consider ACTH Stimulation test &/or steroid therapy: Hydrocortisone & Fludrocortisone. 8-24 1. Consider Vasopressin if shock refractory to first-line vasopressors. hours 2. Consider PA Catheter if pressor-dependent despite achieving target CVP. 3. Consider Xigris if patient meets defined inclusion/exclusion criteria. 4. Initiate enteral feeding & intensive insulin therapy. 5. Hemodialysis therapy for patients in renal failure. 6. ARDS ventilation protocol if indicated. Multidisciplinary Care Provider Signatures: RN (0700-1900): _____________________________ Allied Health: ________________________________ RN (1900-0700): _____________________________ ________________________________ Physician: __________________________________ ________________________________ ACNP: _____________________________________ ________________________________