Principles of history taking
advertisement

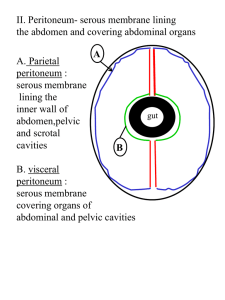
Principles of History Taking Dr Thamer Bin Traiki Prepare yourself to be a good physician History Taking A process of gathering information during patient interview as part of patient clinical assessment. Importance • Obtaining an accurate Hx is the critical 1st step in determining the etiology of a patient’s problem . • A proper history and examination will get you to your diagnosis almost 70% of the time . Set Up – Your appearance is important (wearing proper uniform, ie. Lab coats, I.D., etc.) – Your way of asking the Qs – See him walking in and not in the cubicle & allow a relative to be there if the patient wants. – Provide a safe & private environment Cont.. • Introduce yourself • Greeting patient – By name – Shake hands – Avoid unfamiliar or demeaning terms Be alert and pay him full attention The way of getting the Hx • • • • Ask open questions Listen carefully Take notes Avoid interruption except – Special situations • History should be in the following order : – – – – – – – Personal data Present complaint (c/o). History of present complaint. Systemic enquiry. Past history: surgical, medical , drug history Family history Social history Personal Data Date and Time Name & File number ( Medical record number) Age Gender Religion Marital status Occupation Residency Who gave the history? Chief Complaint • Present complaint or problems : – Symptom/Symptoms that caused patient to seek care and their duration . – In the patient’s own words – If multiple , list them in order of severity . Chief complaint may be misleading Problem may be more serious than the chief complaint History of the presenting Illness • Elaborate the symptom in medical terminology – Provides full clear, chronological details of the history of the main problem/s . • Previous similar attack/s should be included here . • What had been done for the patient if any • Elaborate the system involved. • Add any related symptoms . Systemic Review • Negative symptoms are as important as positive one. • You have to ask about them all, and keep repeating them in each patient, to memorize them well. Neuro • • • • • • • Nervousness Excitability Tremor Fainting attacks Blackout Loss of consciousness Changes of smell, Vision or hearing • • • • • • • Muscle weakness Paralysis Sensory disturbances Paraesthesiae Headaches Change of behavior Fits Cardiovascular & Resp • • • • • • • • Cough Sputum Haemoptysis Dyspnoea Hoarseness Wheezing Chest pain Paroxysmal nocturnal dyspnoea • • • • • • • Orthopnea Palpations Dizziness Ankle swelling Pain in limbs Walking distance Temperature and color of hands and feet GI • • • • • • • • Appetite Diet Abnormal Taste Dysphagia Odynophagia Regurgitation Indigestion Itching • • • • • • • • Vomiting Haematemses Abdominal pain Abdominal Distension Bowel habit Melena PR bleeding Jaundice Urogenital • Loin pain • Symptoms of uremia – – – – – – Headache Drowsiness Fits Visual disturbances Vomiting Edema of ankles, hands of face • Lower urinary tract symptoms ( LUTS) • Painful micturition • Polyuria • Color of urine • Hematuria • Male Infertility history • Sexual history Musculoskeletal • • • • • Aches or Pain in muscles, bones and joints Swelling of joints Limitation of joints movements Weakness Disturbance of gait • Constitutional symptoms: – Weight loss/gain – Fever – Night sweats Past Hx. • • • • • • • Childhood illnesses Adult illnesses Accidents and injuries Surgeries or hospitalizations Blood transfusion Drugs : Insulin, Steroids and OCP Allergy to any medications or food Family Hx • Health of immediate family – father , mother , 1st degree relatives – HTN, DM , heart disease, contagious illnesses • Potential for hereditary diseases Social Hx • • • • • • • • Detailed marital status Living accommodation Occupation Travel abroad Leisure activity Smoking Drinking Eating habits Sensitive Topics • Alcohol or drug use • Physical abuse or violence • Sexual issues Sensitive Topics Guidelines • • • • • • Respect patient privacy Be direct and firm Avoid confrontation Be nonjudgmental Use appropriate language Document carefully – Use patient’s words when possible Special Challenge • Silence • Overly talkative patients • Patients with multiple symptoms • Anxious patients • Limited intelligence • Crying • • • • Anger and hostility Intoxication Depression Confusing behavior or histories • Developmental disabilities • Language barrier Cont.. • False reassurance – May be tempting – Avoid early reassurance or “over reassurance” • Unless it can be provided with confidence Common surgical symptoms • Pain • Lump • Ulcer Pain Hx 1. Site 2. Time & mode of onset 3. Duration 4. Severity 5. Nature ( Character) 6. Progression of pain 7. The end of pain 8. Relieving factors 9. Exaggerating (Exacerbating) factors 10. Radiation 11. Cause Visceral pain • Visceral peritoneum is innervated bilaterally by the autonomic nervous system. • The bilateral innervation causes visceral pain to be midline, vague, deep, dull, and poorly localized. • Visceral pain is triggered by inflammation, ischemia, and geometric changes such as distention, traction, and pressure. ( usually the result of distention of a hollow viscus ). • Embryologic origin of the affected organ determines the location of visceral pain in the abdominal midline. – Foregut(stomach to the second portion of the duodenum, liver and biliary tract, pancreas, spleen) , present as epigastric pain. – Midgut (second portion of the duodenum to the proximal two thirds of the transverse colon) pain present as periumbilical pain. – Hindgut (distal transverse colon to the anal verge) pain present with suprapubic pain. Parietal pain • Parietal peritoneum is innervated unilaterally via the spinal somatic nerves that also supply the abdominal wall. • Unilateral innervation causes parietal pain to localize to one or more abdominal quadrants . • Sharp, severe, and well localized. • The anterior and lateral abdominal wall is innervated from vertebral segments T7 to L1, whereas the posterior abdominal wall is from L2 to L5. Parietal pain : – Triggered by : • Irritation of the parietal peritoneum by an inflammatory process (e.g., chemical or bacterial). • Mechanical stimulation, such as a surgical incision. Referred pain • Arises from a deep visceral structure but is superficial at the presenting site i.e. pain felt at a remote area from the diseased organ . • It results from central neural pathways that are common to the somatic nerves and visceral organs i.e. misinterpretation of visceral afferent impulse that cross the nerve cells to the corresponding somatic dermatome within the CNS . • Radiating pain is pain in remote area but in continuity with the diseased organ . Lump & Ulcer • • • • • • • When did u notice it ? How did u notice it? What are the associated symptoms ? Persistence ( does it ever disappear ?) Progression ( change in its size ) Any other lump currently or previously What do u think the cause ? Questions