Transplantation of the sensitized patient
advertisement

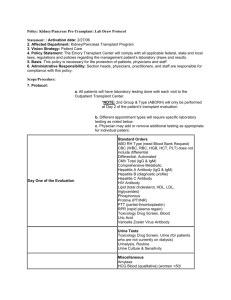
Transplantation of the Sensitized Patient Heidi Schaefer, MD Associate Professor of Medicine Vanderbilt University Case Presentation • 30-year old male with congential kidney disease who underwent LDTx from his mother in 1994 • Kidney failed in 2012 due to biopsy proven chronic allograft nephropathy • PRA class I % = 0 and class II % = 25 • Noted to have anti-HLA antibodies (DQ8, DQA1*03) against his brother • What are his transplant options? HLA Class I and II Inheritance of HLA Haplotypes • HLA genes highly polymorphic • Multiple different nucleotide sequences for each gene have evolved • Millions of possible combinations of HLA types Kidney Matching • HLA “typing” identifies the alleles carried by a person. • HLA “matching” compares donor alleles to recipient alleles. • Degree of HLA matching at the HLA-A, -B, -DR loci affects the survival of the allograft. Panel Reactive Antibody (PRA) • Anti-HLA antibodies are made following exposure to blood transfusions, pregnancy and previous tissue transplants. • Can react with HLA molecules on the endothelia of a transplanted organ’s blood vessels causing rejection and damage to the organ. • Determines if someone is “high immunologic risk or sensitized” – PRA >30% is considered “high” Crossmatch • Final pretransplant immunologic screening step. • Detects donor-directed antibodies in the sera of a potential transplant recipient. • A positive crossmatch is a relative contraindication to transplantation. Sensitization • 91,000 patients on waiting list for kidney transplant • 17% have had previous transplant • 36% are sensitized per UNOS database PRA Incidence 1-10% 4% 11-50% 10% 51-79% 6% 80-100% 16% Prevalence of HLA Sensitization in Kidney Transplant Candidates Improvement in histocompatibility techniques may account for the increase in prevalence along with the increased number patients who lost their allografts. Problems in Sensitized Recipients • Sensitized recipient may have living donor but cannot receive transplant due to +CM • Longer waiting times for deceased donor • Higher acute and chronic rejection rates • Lower graft survival PRA 5-year graft survival 0-9% 72.1% 10-79% 65.6% PRA >80% 61.8% UNOS data, based on 1997-2000 transplants Overview • Detection of anti-HLA antibodies • Agents used in desensitization • Options for the sensitized patient Pre-transplant desensitization on the waiting list Desensitization protocols with living donors Paired-kidney exchange • Treatment of antibody mediated rejection Anti-HLA Antibody Detection Techniques for Solid Organ Transplantation Anti-HLA Antibody CDC Techniques PRA Solid Phase Assay ELISA-PRA HLA Cross-match CDC Cross-match T: AHG B: Amos Flow Cross-match T and B cell (IgG) (With or without Pronase) Flow Cytometer Flow ScreeningPRA Luminex Single AntigenCPRA/DSA Strength of antibodies Strength of T and B cell Flow Cross-match: T cutoff: <50 MCS B cutoff: < 150 MCS are negative cross-match. MFI; SFI; MESF Abbreviations: HLA:human luekocyte antigen; CDC: complement-dependent-cytotoxicity; DSA: donor specific antibody; CPRA: calculated panel reactive antibody; MFI: mean fluorescence intensity; SFI: standardized fluorescence Intensity; MESF: molecular equivalent soluble fluorescence; MCS:median channel shift. Quantitating Antibody: Flow Cytometry and Luminex Single Antigen Bead Assays Flow Cytometry Positive Readout: Median Channel Shift T cell cross match >50 B cell cross match >150 Negative Luminex Single Antigen Bead Assay Readout: Mean Fluorescence Intensity Class I Channel Shift MFI Positive Class II Overview • Detection of anti-HLA antibodies • Agents used in desensitization • Options for the sensitized patient Pre-transplant desensitization on the waiting list Desensitization protocols with living donors Paired-kidney exchange • Treatment of antibody mediated rejection Basic Concepts in Desensitization • Removal of existing antibodies Plasmapharesis Immunoadsorption • Inhibition of residual antibody and complement cascade Intravenous Immunoglobulin (IVIg) Eculizumab (C5 inhibitor) • Depletion of antibody producing cells Naïve and memory B cells: rituximab Plasma cells: bortezomib • Suppression of the T cell response Induction agents Triple immunosuppression with CNI, MMF, steroids Mechanisms of IVIG Jordan SC et al. Transplantation 2009; 88:1 Eculizumab • Genetically humanized monoclonal antibody • Anti-C5 • Blocks the activation of terminal complement • FDA approved for treatment of PNH • Primarily used for AMR • Increased risk of infections with encapsulated bacteria Hillmen et al. NEJM 2006; 355:1233 Rituximab • Genetically engineered monoclonal murine/human antibody • Anti-CD20 • FDA approved for treatment of lymphoma • Used for desensitization and AMR Bortezomib • Proteasome inhibitor • Directly targets antibody production by plasma cells • FDA approved for multiple myeloma • Primarily used for AMR • Side effects include thrombocytopenia and disabling neuropathy Richardson et al. NEJM 2003; 348:2609 Overview • Detection of anti-HLA antibodies • Agents used in desensitization • Options for the sensitized patient Pre-transplant desensitization on the waiting list Desensitization protocols with living donors Paired-kidney exchange • Treatment of antibody mediated rejection • 35% of IVIG treated patients were transplanted within 2 years as compared to 17% in placebo group • Projected mean time to transplantation was 4.8 years in IVIG treated patients and 10.3 years in placebo group • Mean PRA levels were decreased to 50% from 80% at 4 months • 20 highly sensitized patients underwent desensitization with IVIG and rituximab over 4-week period • 16 (80%) received transplant • 6 deceased donor • 10 living donor • Outcomes at 12 months • Patient survival = 100% • Graft survival = 94% • Acute rejection rate = 50% • AMR = 31% • 76 highly sensitized patients underwent desensitization with IVIG and rituximab over 4-week period • 45 deceased donor • 31 living donor • Deceased donor waiting times reduced from 96 months to 4 months • Outcomes at 24 months • Patient survival = 95% • Graft survival = 84% • Acute rejection rate = 37% • AMR = 29% • Development of AMR was significantly associated with strength of DSA by SFI units Vanderbilt Experience • 27 patients • 15 treated with rituximab • Outcomes • Patient survival = 96% • Graft survival = 93% • 10 rejection episodes • 4 AMR • Rejection free graft survival improved with rituximab therapy • Received IVIG and plasmapharesis pre/post-transplant • 5 patients (28%) developed AMR * PP not viable option for those on waiting list as does not result in durable reduction in HLA antibody • 211 highly sensitized patients who underwent live donor transplant • Treated with PP/low dose IVIG • Desensitization with live donor provided significant survival benefit as compared with waiting for compatible organ Comparison of PP vs. High-Dose IVIG Desensitization Stegall et al. AJT 2006; 6: 346-351 Overview • Detection of anti-HLA antibodies • Agents used in desensitization • Options for the sensitized patient Pre-transplant desensitization on the waiting list Desensitization protocols with living donors Paired-kidney exchange • Treatment of antibody mediated rejection *Antibody mediated rejection significantly associated with development of transplant glomerulopathy. Transplant Glomerulopathy Cosio et al. AJT 2008; 8: 492-496 100% n=2 100 88% Graft Loss (%) 75 57% n=7 47% 50 35% 25 30% 0 n=8 6% 6% 0 I 24% II III Type of AMR Median SCr = 1.6 mg/dL (0.8-2.7 mg/dL) TG – transplant glomerulopathy Patient Actuarial Death- TG Survival censored GRAFT SURVIVAL No CMV Proteinuria BKV Pathologic Diagnosis of Rejection Criteria for Antibody Mediated Rejection Clinical Outcomes Per Luminex MFI Values IVIG only IVIG only IVIG/PP____ DSA MFI < 6,000 DSA MFI > 6,000 DSA MFI>6,000 (n=33) (n=17) (n=20) ___________________________________________________________________________________ Median F/U (mos) Patient survival Graft survival Living Deceased-donor Acute rejection AMR ACR Biopsy proven CAN Transplant glomerulopathy Median Cr (mg/dl) Patients with Cr < 1.4 DSA loss during F/U 30 (4-80) 100% 97% 100% 88% 0% 0% 0% 6% 6% 1.1 (0.6-3.1) 81% 77% Akalin et al. CJASN 2008; 3: 1160-1167 40 (14-53) 100% 65% 67% 64% 59% 47% 12% 36% 12% 1.2 (1.0-3.1) 73% 31% 16 (12-28) 90% 75% 88% 67% 20% 15% 5% 20% 10% 1.4 (0.8-1.9) 87% 36% No DSA identified MFI <5,000 and >0 MFI >5,000 and <10,000 MFI >10,000 Bortezomib Therapy for AMR • Directly targets antibody production by plasma cells • Side effects: thrombocytopenia and peripheral neuropathy • Bortezomib alone is not adequate therapy for AMR • Outcomes primarly in case series Eculizumab Therapy for AMR Overview • Detection of anti-HLA antibodies • Agents used in desensitization • Options for the sensitized patient Pre-transplant desensitization on the waiting list Desensitization protocols with living donors Paired-kidney exchange • Treatment of antibody mediated rejection Traditional Paired Kidney Exchange Kidney Transplant Chains non-directed altruistic donor R R D R Cluster #1 D R Cluster #2 D R D D R Cluster #3 Etc. D Paired Kidney Exchange Programs Washington Regional Voluntary Living Donor Registry New England Program for Kidney Exchange (NEPKE) Ohio Organ Transplantation Consortium Alliance for Paired Donation Johns Hopkins Medical Institutions North Central Donor Exchange Cooperative National Kidney Registry UNOS