Patho Ch28 pp1263
advertisement
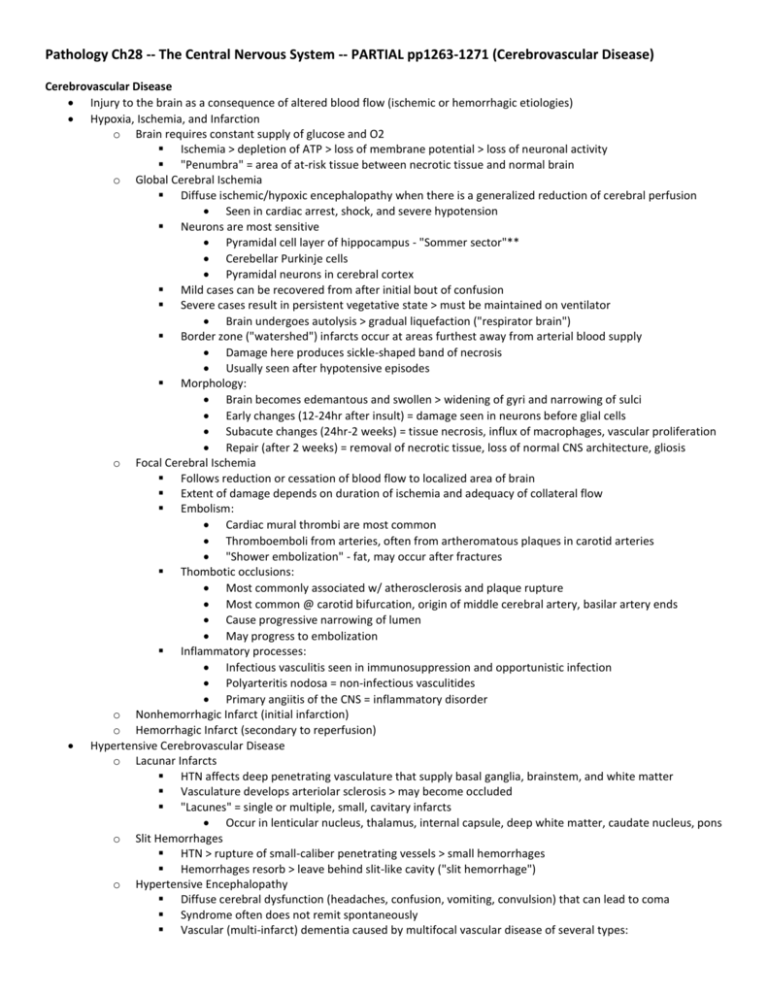
Pathology Ch28 -- The Central Nervous System -- PARTIAL pp1263-1271 (Cerebrovascular Disease) Cerebrovascular Disease Injury to the brain as a consequence of altered blood flow (ischemic or hemorrhagic etiologies) Hypoxia, Ischemia, and Infarction o Brain requires constant supply of glucose and O2 Ischemia > depletion of ATP > loss of membrane potential > loss of neuronal activity "Penumbra" = area of at-risk tissue between necrotic tissue and normal brain o Global Cerebral Ischemia Diffuse ischemic/hypoxic encephalopathy when there is a generalized reduction of cerebral perfusion Seen in cardiac arrest, shock, and severe hypotension Neurons are most sensitive Pyramidal cell layer of hippocampus - "Sommer sector"** Cerebellar Purkinje cells Pyramidal neurons in cerebral cortex Mild cases can be recovered from after initial bout of confusion Severe cases result in persistent vegetative state > must be maintained on ventilator Brain undergoes autolysis > gradual liquefaction ("respirator brain") Border zone ("watershed") infarcts occur at areas furthest away from arterial blood supply Damage here produces sickle-shaped band of necrosis Usually seen after hypotensive episodes Morphology: Brain becomes edemantous and swollen > widening of gyri and narrowing of sulci Early changes (12-24hr after insult) = damage seen in neurons before glial cells Subacute changes (24hr-2 weeks) = tissue necrosis, influx of macrophages, vascular proliferation Repair (after 2 weeks) = removal of necrotic tissue, loss of normal CNS architecture, gliosis o Focal Cerebral Ischemia Follows reduction or cessation of blood flow to localized area of brain Extent of damage depends on duration of ischemia and adequacy of collateral flow Embolism: Cardiac mural thrombi are most common Thromboemboli from arteries, often from artheromatous plaques in carotid arteries "Shower embolization" - fat, may occur after fractures Thombotic occlusions: Most commonly associated w/ atherosclerosis and plaque rupture Most common @ carotid bifurcation, origin of middle cerebral artery, basilar artery ends Cause progressive narrowing of lumen May progress to embolization Inflammatory processes: Infectious vasculitis seen in immunosuppression and opportunistic infection Polyarteritis nodosa = non-infectious vasculitides Primary angiitis of the CNS = inflammatory disorder o Nonhemorrhagic Infarct (initial infarction) o Hemorrhagic Infarct (secondary to reperfusion) Hypertensive Cerebrovascular Disease o Lacunar Infarcts HTN affects deep penetrating vasculature that supply basal ganglia, brainstem, and white matter Vasculature develops arteriolar sclerosis > may become occluded "Lacunes" = single or multiple, small, cavitary infarcts Occur in lenticular nucleus, thalamus, internal capsule, deep white matter, caudate nucleus, pons o Slit Hemorrhages HTN > rupture of small-caliber penetrating vessels > small hemorrhages Hemorrhages resorb > leave behind slit-like cavity ("slit hemorrhage") o Hypertensive Encephalopathy Diffuse cerebral dysfunction (headaches, confusion, vomiting, convulsion) that can lead to coma Syndrome often does not remit spontaneously Vascular (multi-infarct) dementia caused by multifocal vascular disease of several types: (1) Cerebral athersosclerosis (2) Vessel thrombosis or embolization from carotid vessels or from heart (3) Cerebral arteriolar sclerosis from chronic hypertension Binswanger disease = when injury preferentially involves large areas of subcortical white matter Intracranial Hemorrhage o Intraparenchymal Hemorrhage (within the brain) Rupture of small intraparenchymal vessels > hemorrhage within brain Often associated w/ sudden onset of neurologic symptoms (stroke) Ganglionic hemorrhages = within basal ganglia and thalamus (due to HTN) Chronic HTN associated w/ Charcot-Bouchard microaneurysms = site of rupture Lobar hemorrhages = within cerebral hemispheres (due to cerebral amyiloid angiopathy) Amyloidogenic peptides deposited in walls of medium and small meningeal and cortical vessels o Same peptides found in Alzheimer's disease Deposition weakens vessel wall > hemorrhage Location of hemorrhage determines the clinical manifestations o Subarachnoid Hemorrhage and Ruptured Saccular Aneurysms "The worst headache I've ever had" Most common cause is rupture of saccular ("berry") aneurysm in a cerebral artery 90% found near major arterial branch points in anterior circulation Structural abnormality of involved vessel = absence of SM and intimal elastic lamina 1.3% will rupture per year, but chances up to 50% in larger aneurysms Ruptures associated w/ acute incidence of intracranial pressure (sexing or pooping) Comes with risk of vasospasm due to vessels being bathed in extravasated blood o Vascular Malformations Classified into (1) arteriovenous, (2) cavernous, (3) capillary telangiectasis, (4) venous angiomas (1) and (2) are associated w/ risk of hemorrhage and development of symptoms Arteriovenous malformations Vessels in subarachnoid space and/or brain Arteriovenous shunting in tangled network for wormlike vascular channels Often show evidence of prior hemorrhage Results in seizure disorder, intracerebral hemorrhage, or subarachnoid hemorrhage Most common site is middle cerebral artery (esp. posterior branches) Cavernous malformations Distended, loosely organized vascular channels Usually no brain parenchyma between vessels Occur most often in cerebellum, pons, and subcortical regions "Low-flow" channels > do not participate in arteriovenous shunting Vessels often surrounded by old hemorrhage, infarction, and calfication Familial forms are common > highly penetrant autosomal dominant trait