Brain Injury in the Term Infant Jeffrey M. Perlman, MBChB
advertisement
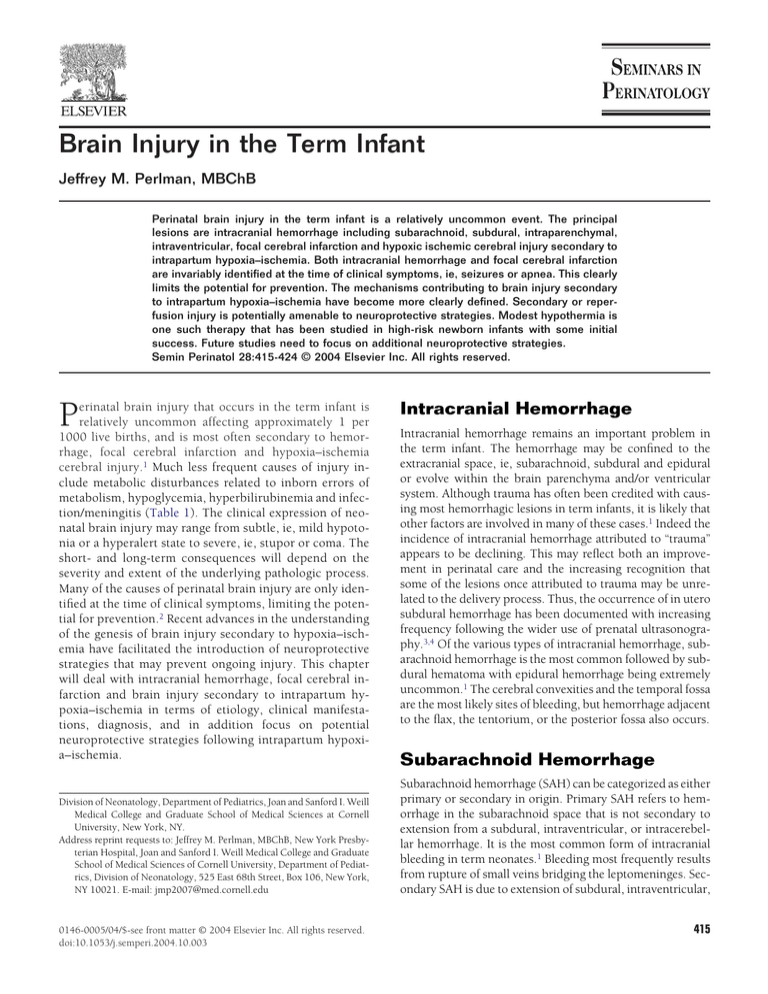
Brain Injury in the Term Infant Jeffrey M. Perlman, MBChB Perinatal brain injury in the term infant is a relatively uncommon event. The principal lesions are intracranial hemorrhage including subarachnoid, subdural, intraparenchymal, intraventricular, focal cerebral infarction and hypoxic ischemic cerebral injury secondary to intrapartum hypoxia–ischemia. Both intracranial hemorrhage and focal cerebral infarction are invariably identified at the time of clinical symptoms, ie, seizures or apnea. This clearly limits the potential for prevention. The mechanisms contributing to brain injury secondary to intrapartum hypoxia–ischemia have become more clearly defined. Secondary or reperfusion injury is potentially amenable to neuroprotective strategies. Modest hypothermia is one such therapy that has been studied in high-risk newborn infants with some initial success. Future studies need to focus on additional neuroprotective strategies. Semin Perinatol 28:415-424 © 2004 Elsevier Inc. All rights reserved. P erinatal brain injury that occurs in the term infant is relatively uncommon affecting approximately 1 per 1000 live births, and is most often secondary to hemorrhage, focal cerebral infarction and hypoxia–ischemia cerebral injury.1 Much less frequent causes of injury include metabolic disturbances related to inborn errors of metabolism, hypoglycemia, hyperbilirubinemia and infection/meningitis (Table 1). The clinical expression of neonatal brain injury may range from subtle, ie, mild hypotonia or a hyperalert state to severe, ie, stupor or coma. The short- and long-term consequences will depend on the severity and extent of the underlying pathologic process. Many of the causes of perinatal brain injury are only identified at the time of clinical symptoms, limiting the potential for prevention.2 Recent advances in the understanding of the genesis of brain injury secondary to hypoxia–ischemia have facilitated the introduction of neuroprotective strategies that may prevent ongoing injury. This chapter will deal with intracranial hemorrhage, focal cerebral infarction and brain injury secondary to intrapartum hypoxia–ischemia in terms of etiology, clinical manifestations, diagnosis, and in addition focus on potential neuroprotective strategies following intrapartum hypoxia–ischemia. Division of Neonatology, Department of Pediatrics, Joan and Sanford I. Weill Medical College and Graduate School of Medical Sciences at Cornell University, New York, NY. Address reprint requests to: Jeffrey M. Perlman, MBChB, New York Presbyterian Hospital, Joan and Sanford I. Weill Medical College and Graduate School of Medical Sciences of Cornell University, Department of Pediatrics, Division of Neonatology, 525 East 68th Street, Box 106, New York, NY 10021. E-mail: jmp2007@med.cornell.edu 0146-0005/04/$-see front matter © 2004 Elsevier Inc. All rights reserved. doi:10.1053/j.semperi.2004.10.003 Intracranial Hemorrhage Intracranial hemorrhage remains an important problem in the term infant. The hemorrhage may be confined to the extracranial space, ie, subarachnoid, subdural and epidural or evolve within the brain parenchyma and/or ventricular system. Although trauma has often been credited with causing most hemorrhagic lesions in term infants, it is likely that other factors are involved in many of these cases.1 Indeed the incidence of intracranial hemorrhage attributed to “trauma” appears to be declining. This may reflect both an improvement in perinatal care and the increasing recognition that some of the lesions once attributed to trauma may be unrelated to the delivery process. Thus, the occurrence of in utero subdural hemorrhage has been documented with increasing frequency following the wider use of prenatal ultrasonography.3,4 Of the various types of intracranial hemorrhage, subarachnoid hemorrhage is the most common followed by subdural hematoma with epidural hemorrhage being extremely uncommon.1 The cerebral convexities and the temporal fossa are the most likely sites of bleeding, but hemorrhage adjacent to the flax, the tentorium, or the posterior fossa also occurs. Subarachnoid Hemorrhage Subarachnoid hemorrhage (SAH) can be categorized as either primary or secondary in origin. Primary SAH refers to hemorrhage in the subarachnoid space that is not secondary to extension from a subdural, intraventricular, or intracerebellar hemorrhage. It is the most common form of intracranial bleeding in term neonates.1 Bleeding most frequently results from rupture of small veins bridging the leptomeninges. Secondary SAH is due to extension of subdural, intraventricular, 415 J.M. Perlman 416 Table 1 Causes of Perinatal Brain Injury in the Term Infant Intracranial Hemorrhage Primary subarachnoid hemorrhage Subdural hematoma Epidural hematoma Intracerebral hemorrhage Thalamic hemorrhage Intraparenchymal hemorrhage Intraventricular hemorrhage Germinal matrix hemorrhage Focal Cerebral Infarction Hypoxic Ischemic Cerebral Injury Vascular abnormalities Aneurysm Arteriovenous malformation Metabolic Disorders Inborn errors of metabolism (eg, hyerpammonemia) Hypoglycemia Hyperbilirubinemia Cerebral Tumors Idiopathic or intraparenchymal hemorrhages and occurs less often. While “trauma” is by far the most common etiology of SAH in term neonates, coagulation disorders and rupture of an intracranial aneurysm or arteriovenous malformation are occasionally responsible. However small SAH is probably frequent even during uncomplicated deliveries, but cause little or no problems and thus goes unrecognized. The most common clinical presentation is seizures, whose onset is on approximately on the second postnatal day. In the interictal period, the infants appear remarkable well. A second presentation is that of recurrent apnea, whose onset may be in the first 24 hours of life. Rarely, a third presentation is that of more extensive bleeding into the cerebrospinal fluid causing seizures, a bulging anterior fontanel or diminished responsiveness. Subdural Hemorrhage Subdural hematoma (SDH) can be categorized into two main groupings according to their origin and direction of spread, ie, supratentorial and infratentorial5 Significant hemorrhage may result from tears in the falx and tentorium or bridging cortical veins secondary to stretching, which is most likely to occur during labor, under circumstances when anterior–posterior compression of the head is associated with excessive vertical molding and frontal– occipital elongation of the cranium.1 Thus SDH has long been considered a traumatic lesion related to difficult parturition. However as noted previously there are several case reports documenting antenatal sudural hematoma.3,4 Moreover SDH has also been documented after spontaneous vaginal delivery.6,7 The clinical expression varies depending on the size and location of the blood. Thus small hemorrhages adjacent to the cerebrum usually cause no major difficulty.6,7 However, depending on location, in particular within the posterior fossa, even small amounts of blood, sometimes result in ob- structive hydrocephalus or striking neurological deficit. Large acute SDH are apt to produce signs of increased intracranial pressure, seizures, and focal neurological deficits. Very large SDH adjacent to the cerebral hemispheres may lead to herniation of the temporal lobe over the tentorial edge, causing ipsilateral third nerve paralysis.6,7 Additional signs with large lesions include a paucity of spontaneous movement, decreased responsiveness as well as nonspecific signs such as metabolic acidosis, hypoglycemia, anemia and hypotension.8,9 Most neonates with a catastrophic syndrome do not survive, and the few who do are usually left with severe neurological sequelae. Chronic subdurals over the convexity usually present with macrocephaly, seizures, or failure to thrive. Epidural Hemorrhage Epidural hemorrhage is a rare lesion in the neonate, accounting for approximately 2% of all cases of neonatal intracranial hemorrhage observed at autopsy.9 Bleeding is derived from branches of the middle meningeal artery or from major veins or venous sinuses. Possible explanations for the infrequent occurrence are: (1) the loose attachment of the meningeal vessels to the overlying bone, which allows the neonate to withstand more trauma to the skull without lacerating the vessel underneath; and (2) the dura which is unusually thick and largely continuous with the inner periosteum. The skull it self is more pliable in infants, and thus less likely to fracture. Progressive neurological dysfunction and death commonly result unless the epidural hemorrhage is evacuated and further bleeding stopped. Diagnosis The diagnosis of subdural, epidural, or subarachnoid hemorrhage is confirmed by computed tomography, which outlines both the location and extent of bleeding in most cases. However, magnetic resonance imaging is more effective than computed tomography in the delineation of posterior fossa hemorrhages.7 Skull radiographs may demonstrate fracture or suture separation, but are not of much help clinically since hematomas are often present without these lesions. Cranial ultrasound scanning is less useful in establishing a diagnosis due the peripheral location of convexity subdural or epidural hemorrhages that limits their visualization. Both cranial ultrasound imaging and computed tomography and more recently magnetic resonance imaging, effectively outline the hydrocephalus that sometimes accompanies intracranial bleeding. Treatment Early diagnosis of intracranial hemorrhage is imperative, since the outcome so often depends on prompt therapy. Large acute subdural and epidural hemorrhages should be surgically evacuated and any source of continued bleeding ligated. Emergency craniotomy is particularly important with tentorial tears extending into the dural sinuses. Decompres- Brain injury in the term infant sion should also be considered for larger intracerebellar hematomas. Smaller subdural or epidural lesions in a stable child will frequently resolve without surgery. No specific treatment is available for acute subarachnoid hemorrhage in neonates, though close follow-up for signs of hydrocephalus is recommended. Prognosis The prognosis following hemorrhage is variable, depending on the size and location of the lesion, the promptness of treatment, and whether underlying brain damage was coincident to the hemorrhage. Epilepsy, mental retardation, motor deficits, or other sequelae may result from intracranial hemorrhage regardless of its site or etiology. In general, the prognosis after subdural hematomas is better in infants than in older children. The outlook for convexity subdural hematoma is often favorable, while the prognosis of patients with posterior fossa subdural hemorrhage is less encouraging. Without surgery, rapid deterioration of brain stem function followed by cardio respiratory failure is typical of these posterior fossa lesions, although occasional patients do well. Isolated subarachnoid and intraventricular hemorrhage may lead to hydrocephalus long after the hemorrhage, but surviving patients otherwise tend to recover fully. Intracerebral Hemorrhage Intracerebral hemorrhage in the term infant is uncommon. Blood may be found within the germinal matrix, ventricles or brain parenchyma. The thalamus appears to be a common site of hemorrhage in the term infant and frequently includes intraventricular hemorrhage as well.10,11 Typically the hemorrhage develops later, ie, during the second week of life, but it may occur earlier. Predisposing factors include prior hypoxic–ischemic cerebral injury, sepsis, and coagulopathy or may be observed in association with subarachnoid or subdural hemorrhage.7,8 Primary intraventricular hemorrhage is rare in the term infant. Documented sources of hemorrhage in this age group include residual germinal matrix, choroids plexus and thalamus. Predisposing factors include prior hypoxia–ischemia, coagulopathies and arteriovenous malformations. The clinical presentation of intracerebral hemorrhage is characterized by sudden onset of marked neurologic abnormalities, including signs of seizures, evidence of increased intracranial pressure and downward eye deviation. A bulging fontanel or blood in the cerebrospinal fluid may be present. Hemiparesis or other focal neurological deficits are uncommon. Neuroimaging, ie, cranial ultrasound, CT or MRI readily establishes the diagnosis. The prognosis is surprisingly good with primary thalamic hemorrhage although when associated with intraventricular hemorrhage, outcome is less favorable.10,11 Cerebral Infarction Cerebral infarction in the neonate, ie, perinatal stroke is a more common than has been considered in the past with an 417 estimate of 1 in 4000 births.12,13 The infarction may arise from both embolic and thrombotic phenomena, however the etiology in most cases remains unclear.12-14 Cerebral embolism is probably the most common cause of stroke in this setting, though the site of origin for the embolism is not always apparent. Other reported causes include intrapartum “asphyxia,” deficiency of one of the systemic coagulation inhibitors (ie, protein C or protein S), primary hemorrhage with vasospasm, meningitis, polycythemia, extracorporeal membrane oxygenation, etc.15-19 The initial clinical manifestations typically consist of seizures or apnea, usually on the second postnatal day. Focal deficits are not common except with large deficits. The diagnosis may be established by cranial ultrasonography, CT or MRI.19 The outcome depends on the location and the extent of the lesion. Involvement of the thalamus is invariably associated with contralateral hemiplegia. Smaller lesions may allow a normal outcome.20 Cerebral Injury Secondary to Intrapartum Hypoxia–Ischemia Hypoxic ischemic cerebral injury that occurs during the perinatal period is one of the most commonly recognized causes of severe, long-term neurological deficits in children, often referred to as cerebral palsy (CP).1,2 The brain injury that develops is an evolving process initiated during the insult and extends into a recovery period, the latter referred to as the “reperfusion phase” of injury. It is during this phase of injury that intervention strategies maybe possible.21 In this section, the pathogenesis, early identification of high-risk infants as potential candidates for neuroprotective strategies and some future interventions following intrapartum hypoxia–ischemia will be briefly reviewed. Pathogenesis The principal pathogenetic mechanism underlying most of the neuropathology attributed to intrapartum hypoxia–ischemia is impaired cerebral blood flow (CBF). This is most likely to occur as a consequence of interruption in placental blood flow and gas exchange, often referred to as “asphyxia” or severe fetal acidemia. The latter is defined as a fetal umbilical arterial pH ⱕ 7.00.2 At the cellular level, the reduction in cerebral blood flow and oxygen delivery initiates a cascade of deleterious biochemical events. Depletion of oxygen precludes oxidative phosphorylation, and results in a switch to anaerobic metabolism. This is an energy inefficient state resulting in rapid depletion of high-energy phosphate reserves including ATP, accumulation of lactic acid and the inability to maintain cellular functions.22 Transcellular ion pump failure results in the intracellular accumulation of Na⫹, Ca2⫹ and water (cytotoxic edema). The membrane depolarization results in a release of excitatory neurotransmitters and specifically glutamate from axon terminals. Glutamate then activates specific cell surface receptors resulting in an influx of Na⫹ and Ca2⫹ into postsynaptic neurons. Within the cytoplasm, there is an accumulation of free fatty acids secondary J.M. Perlman 418 to increased membrane phospholipid turnover. The fatty acids undergo per oxidation by oxygen free radicals that arise from reductive processes within mitochondria and as byproducts in the synthesis of prostaglandins, xanthine and uric acid. Ca2⫹ ions accumulate within the cytoplasm as a consequence of increased cellular influx as well as decreased efflux across the plasma membrane combined with release from mitochondria and endoplasmic reticulum. In selected neurons, the intracellular calcium induces the production of nitric oxide, a free radical that diffuses to adjacent cells susceptible to nitric oxide toxicity. The combined effects of cellular energy failure, acidosis, glutamate release, intracellular Ca2⫹ accumulation, lipid per oxidation and nitric oxide neurotoxicity serve to disrupt essential components of the cell with its ultimate death.1,23 Many factors including the duration or severity of the insult will influence the progression of cellular injury following hypoxia–ischemia. Delayed (Secondary) Brain Injury Following resuscitation, which may occur in utero or postnatally in the delivery room, cerebral oxygenation and perfusion is restored. During this recovery phase, the concentrations of phosphorus metabolites and the intracellular pH return to baseline. However, the process of cerebral energy failure recurs from 6 to 48 hours later in a second phase of injury. This phase is characterized by a decrease in the ratio of phosphocreatine/inorganic phosphate, with an unchanged intracellular pH, stable cardio respiratory status, and contributes to further brain injury.22,24 In the human infant the severity of the second energy failure is correlated with adverse neurodevelopment outcome at 1 and 4 years.25 The mechanisms of secondary energy failure may involve mitochondrial dysfunction secondary to extended reactions from primary insults (eg, calcium influx, excitatory neurotoxicity, oxygen free radicals or nitric oxide formation). Indeed mitochondria play a key role in determining the fate of neurons following hypoxia–ischemia. Thus translocation of apoptotic triggering proteins such as cytochrome c from the mitochondria to the cytoplasm can activate a cascade of proteolytic enzymes termed caspases or cysteine proteases that eventually trigger nuclear fragmentation.23 Recent evidence also suggests that circulatory and endogenous inflammatory cells/mediators also contribute to ongoing brain injury.26 The potential role of inflammation is discussed in greater detail next. Inflammatory Mediators Inflammatory mediators appear to play a critical role in the pathogenesis of hypoxic ischemic brain injury. Thus expression of IL-1-  and TNF ␣ mRNA has been demonstrated within 1 to 4 hours following hypoxia ischemia,27 along with the induction of ␣ and  chemokines followed by neutrophil invasion of the area of infarction.28 Furthermore a low dose of bacterial endotoxin administered four hours before hypoxia– ischemia in rats, induces cerebral infarction in response to short periods of hypoxia–ischemia that usually causes little or no injury. This endotoxin-induced sensitization of the imma- ture brain occurs independent of cerebral blood flow changes and/or hyperthermia and is associated with an altered expression of CD14 mRNA.29 Inflammatory cytokines may have a direct toxic effect via increased production of inducible nitric oxide synthase, cyclo-oxygenase and free radical release, or indirectly via induction of glial cells to produce neurotoxic factors such as excitatory amino acids. The important role of cytokines in perpetuating excitotoxic injury is suggested from experimental observations in which administration of IL-1 endogenous receptor antagonists as well as neutralizing antibody are associated with a reduction in excitotoxic and ischemic injury in mice.30,31 However, cytokines that potentiate brain damage following ischemia also seem to play a beneficial neurotrophic effect. Thus TNF knockout mice were shown to have increased neuronal cell degeneration following ischemia and excitotoxic injury suggesting a critical role for endogenous TNF in regulating the cellular responses to brain injury.32 In addition administration of exogenous IL-6 following ischemia produced by middle artery occlusion also results in marked neuroprotection.33 Thus inflammatory cytokines appear to exert both beneficial and deleterious effects following ischemia. This dual effect will likely complicate the task of developing targeted interventions against the inflammatory response. Mechanisms of Neuronal Death Following Hypoxia–Ischemia The mechanism of neuronal cell death in animals and human following hypoxia–ischemia includes neuronal necrosis and apoptosis. The intensity of the initial insult may determine the mode of death with severe injury resulting in necrosis, while milder insults result in apoptosis.34 Necrosis is a passive process of cell swelling, disrupted cytoplasmic organelles, loss of membrane integrity and eventual lyses of neuronal cells and activation of an inflammatory process. By contrast, apoptosis is an active process distinguished from necrosis by the presence of cell shrinkage, nuclear pyknosis, chromatin condensation and genomic fragmentation, events that occur in the absence of an inflammatory response.35 These two processes of neuronal death can be demonstrated following hypoxia ischemia in both animals and humans.1,23,35 Since the mechanisms of neuronal necrosis versus apoptosis likely differ (see above), strategies to minimize brain damage in an affected infant following hypoxia–ischemia likely will have to include interventions that target both processes. Clinical Manifestations Clinical findings will vary depending on the timing of the intrapartum insult, the duration of the insult and fetal adaptive mechanisms.1,2 Commonly the infant will initially appear clinically depressed, ie, lethargic with central hypotonia, particularly proximally (likely related to reduced parasagittal blood flow) and with reduced deep tendon reflexes. Over the Brain injury in the term infant next several hours there is in most cases an improvement in the clinical status with an improvement in the level of responsiveness. Indeed in some infants there is an appearance of a hyperalert state. The hypotonia generally tends to persist and the reflexes are now easily elicited. In some there maybe sensory stimulus clonus. Clinical seizures if present are usually noted between 12 and 24 hours of postnatal age. The subsequent clinical course may range from a hyperalert state with rapid recovery and no seizures (the most common presentation), a state designated as Sarnat Stage 1 encephalopathy,36 to seizures with moderate encephalopathy characterized by lethargy, a state designated Sarnat Stage 2 encephalopathy, and finally with progression to severe encephalopathy characterized by stupor or coma, loss of brainstem signs, loss of deep tendon reflexes, absence of clinical ⫾ electrographic seizures a state designated Sarnat Stage 3 encephalopathy. The clinical findings usually evolve over the first 24 to 72 hours of postnatal life. There are a small number of infants who will present and maintain a severe encephalopathic state from birth. The outcome following intrapartum hypoxia–ischemia is strongly related to the severity of the clinical examination. Thus almost all infant with stage 1 encephalopathy develop normally, approximately 75 to 80% of infants with stage 2 encephalopathy develop normally, whereas no infants with stage 3 encephalopathy develops normally.1 Indeed the outcome is dismal in all cases. The extent of damage and likely outcome can be supported with an electroencephalogram (EEG) (the appearance of a burst suppression pattern is associated with a poor prognosis), and magnetic resonance imaging (see below). The recognition and importance of reperfusion injury, and the potential to implement neuroprotective strategies and thus reduce neurologic morbidity has led to an earlier identification of high risk infants with a modified Sarnat scoring system and use of a modified EEG (see subsequent section on treatment). Detection of Neuronal Injury with Magnetic Resonance (MR) Imaging MR techniques have become very important in delineating evolving structural, metabolic and functional changes following intrapartum hypoxia–ischemia.37 Thus using conventional MR, three patterns of signal abnormalities can be identified including injury to the thalami and/or posterior–lateral putamen with involvement of the subcortical white matter in the most severe cases; injury to the parasagittal gray matter and subcortical white matter, posteriorly usually more than anteriorly; and focal or multifocal injury.38 Conventional MR studies are of limited value in the early phases, ie, hours and days following the insult. More recently the use of advanced MR techniques, ie, diffusion weighted imaging (DWI) has been utilized to detect early injury.39 This technique measures the self-diffusion of water detected as an apparent diffusion coefficient (ADC).37 Thus the ADC decreases with acute injury and is reflective of reduced water diffusivity in the tissue. Studies of adult arterial infarcts have shown that 419 DWI signal changes occur within minutes of symptom onset and hours before changes become apparent on T1- or T2weighted images.40 This earlier detection of injury may facilitate intervention before irreversible injury. DWI changes may be negative if it is performed earlier than 24 hours of life or later than 8 days of life.37 Recently the development of magnetic resonance spectroscopy (MRS) has facilitated the detection of tissue metabolism and in vivo biochemistry.37,38 Thus proton MRS (1H-MRS) can identify a spectrum of metabolites including lactate, creatine, N-acetylaspartate (NAA) and glutamine to name a few. Indeed elevated lactate levels have been demonstrated following hypoxia–ischemia in 1HMRS with regional differences, ie, higher lactate/NAA ratios in basal ganglia than in occipito-parietal cortex.41 Moreover an early elevated lactate/creatine ratio with 1H-MRS coupled with a low phosphocreatine/inorganic phosphate ratio done with phosphorus MRS correlated with neurodevelopmental outcome at 1 year.42 Thus the data indicate that MRS plays an important role in the assessment of the encephalopathic infant following intrapartum hypoxia–ischemia. Management The goals of management of a newborn infant who has sustained a hypoxic–ischemic insult and is at risk for evolving injury should include: (1) early identification of the infant at highest risk for evolving injury, (2) supportive care to facilitate adequate perfusion and nutrients to the brain, and (3) consideration of interventions to ameliorate the processes of ongoing brain injury. Each of these approaches is briefly discussed next. Early Identification of High Risk Infants The initial step in management is early identification of those infants at greatest risk for evolving to the syndrome of hypoxic–ischemic encephalopathy (HIE). This is a highly relevant issue because the therapeutic window, ie, the time interval following hypoxia–ischemia during which interventions might be efficacious in reducing the severity of ultimate brain injury, is likely to be short. Based on experimental studies it is estimated to vary from 2 to 6 hours. Given this presumed short window of opportunity, infants must be identified as soon as possible following delivery to facilitate the implementation of early interventions. There are increasing data to indicate that the highest risk infant can be identified shortly after birth by a constellation of findings. These include evidence of a sentinel event during labor, ie, fetal heart rate abnormality, a severely depressed infant (low extended Apgar score), the need for resuscitation in the delivery room (ie, intubations, chest compression ⫾ epinephrine administration), evidence of severe fetal acidemia (cord umbilical artery pH ⬍ 7.00 and/or base deficit ⬎ ⫺16 mEq/L),43 followed by evidence of an early abnormal neurologic examination and/or abnormal assessment of cerebral function, ie, integrated EEG.44-46 Thus in a prospective study of 50 infants J.M. Perlman 420 Table 2 A Guide to the Supportive Management of an Infant at Risk for Hypoxic Ischemic Cerebral Injury Ventilation Maintain paCO2 within a normal range Perfusion Promptly treat hypotension Avoid hypertension Fluid status Initial fluid restriction Follow serum sodium and daily weights Blood glucose Maintain blood glucose within a normal range Avoid hypoglycemia Seizures Treat clinical seizures, particularly with an electrographic correlate Potential role of prophylactic phenobarbital Electrolyte imbalance Monitor serum electrolytes, calcium and magnesium who had evidence of intrapartum distress, Apgar score 5 at 5 minutes, or cord arterial pH 7.00 and underwent an early neurologic examination using a modified Sarnat staging system (stages 2 and 3 were regarded as abnormal) and a blinded simultaneous a-EEG measurement, predictive values were calculated for a short-term abnormal outcome defined as persistent moderate to severe encephalopathy beyond 5 days. An abnormal outcome evolved in 14 (28%) of the 50 infants. The neurologic examination was performed at 5 ⫾ 3 hours after delivery. A short-term abnormal outcome occurred in 9 (53%) of 17 infants with initial stage 2 and in both infants with initial stage 3 encephalopathy. In addition, 13 infants manifested features of both stage 1 and 2 encephalopathy and post hoc were classified (S1–2). Three of the latter infants (23%) developed an abnormal short-term outcome. The aEEG was abnormal in 15 (30%) infants, 11 (73%) of whom developed an abnormal outcome. An abnormal a-EEG was more specific (89% versus 78%), had a greater positive predictive value (73% versus 58%), and had similar sensitivity (79% versus 78%) and negative predictive value (90% versus 91%) when compared with an abnormal early neurologic examination. A combination of abnormalities had the highest specificity (94%) and positive predictive value (85%). Thus a combination of the a-EEG and the neurologic examination shortly after birth enhances the ability to identify high-risk infants and limits the number of infants who would be falsely identified compared with either evaluation alone.46 Supportive Care Supportive care should be directed toward the maintenance of adequate ventilation (avoid hyper and hypocarbia), avoidance of hypotension, judicious fluid management, avoidance of hypoglycemia and the treatment of seizures21 (Table 2). For the purposes of this review, the importance of seizures as a cause of ongoing injury and the potential role of prophylactic phenobarbital is briefly discussed next. Seizures as a Cause of Ongoing Injury Although seizures are a consequence of the underlying brain injury, ie, hypoxia–ischemia, seizures activity in itself may contribute to ongoing injury. Experimental evidence strongly suggests that repetitive seizures disturb brain growth and development as well as increase the risk for subsequent epilepsy.47,48 Despite the potential adverse effects of seizures, the question of which infants should be treated remains controversial.1,49 This is in part related to the observation that not all clinical seizures have an electrographic correlation.50 Prophylactic Phenobarbital Experimental data indicates that barbiturate pretreatment and even early post treatment in adult animals subjected to cerebral hypoxia–ischemia reduces the severity of ultimate brain damage. The prophylactic administration of “high dose” barbiturates to infants at highest risk for evolving to HIE has been evaluated in two small studies with conflicting results.51,52 In the first randomized study, the administration of Thiopental initiated within two hours and infused for 24 hours did not alter the frequency of seizures, intracranial pressure or short-term neurodevelopmental outcome at 12 months.51 Of importance was the observation that systemic hypotension occurred significantly more often in the treated group. In the second randomized study, Phenobarbital 40 mg/kg body weight administered intravenously between 1 and 6 hours to asphyxiated infants was associated with subsequent neuroprotection.52 Although there was no difference in the frequency of seizures between the two groups in the neonatal period, 73% of the pretreated infants compared with 18% of the control group (P ⬍ 0.05) revealed normal neurodevelopmental outcome at 3-year follow-up. No adverse effect of phenobarbital administration was observed in this study. Thus, the role of prophylactic barbiturates in high-risk infants remains unclear at this current time and may be worthy of further investigation. Potential Neuroprotective Strategies Aimed at Ameliorating Secondary Brain Injury Hypothermia Modest systemic or selective cooling of the brain by as little as 2-4°C has been shown to reduce the extent of tissue injury in experimental studies as well as human following events such as stroke, trauma or cardiac arrest.53-68 Potential mechanisms of neuroprotection with hypothermia include inhibition of glutamate release, reduction of cerebral metabolism which in turn preserves high energy phosphates, decrease in intracellular acidosis and lactic acid accumulation, preservation of endogenous antioxidants, reduction of nitric oxide production, prevention of protein kinase inhibition, improvement of Brain injury in the term infant protein synthesis, reduction of leukotriene production, prevention of blood brain barrier disruption and brain edema and inhibition of apoptosis.64,66 Although neuroprotection following intraischemic hypothermia is well established, the effects of postischemic hypothermia have been less certain. The latter is the typical scenario in the human newborn. Before initiating hypothermia as a therapeutic strategy in neonates, several factors had to be considered. The first relates to duration of therapy. Thus, brief postischemic hypothermia, ie, less than 6 hours results is only partial or temporary neuroprotection in most experimental animals.53,66 Prolonging postischemic hypothermia from 24 to 72 hours attenuates brain damage and improves behavioral performance.57,58,66 The second factor relates to the degree of hypothermia. Accordingly, moderate hypothermia at brain temperatures of 32 to 34°C initiated immediately or within a few hours after reperfusion and continued for 24 to 72 hours has been shown to favorably affect outcome in adult and newborn animals.57,58 The third factor relates to the delay in initiation of therapy. Clearly, the sooner hypothermia can be initiated, the more likely it is to be successful. Indeed studies indicate that if therapy is initiated beyond 6 hours following hypoxia–ischemia or following the onset of seizures, that hypothermia is not neuroprotective.59,60 The fourth factor relates to the method of achieving hypothermia. Selective head cooling is attractive because it reduces potential side effects (see below) but is associated with differential gradients within the brain.69 Total body cooling is more likely to be associated with side effects but less temperature gradient within the brain. A major concern of hypothermia in newborn infants relates to potential adverse effects including hypoglycemia, reduction of myocardial contractility and ventilation–perfusion mismatch, increased blood viscosity, acidbase and electrolyte imbalance and an increased risk of infection.65,70 To address the practicality and safety of mild or minimal hypothermia, pilot studies were conducted utilizing both selective and systemic methods to cool the brain in term neonates with moderate to severe encephalopathy.71,72 Subsequently two large randomized multicenter studies have been undertaken and completed in term infants at highest risk for evolving to moderate and/or severe encephalopathy, using either selective or systemic modest hypothermia. One of these studies utilizing selective head cooling has reported follow up results at 18 months (A. Gunn, personal communication). There was no overall protective effect of hypothermia observed with regard to the development of cerebral palsy and/or death. However for those infants who presented with moderate encephalopathy and without electrographic seizures, a significant benefit of hypothermia was noted. Conversely no effect was observed in those infants with severe encephalopathy and/or early seizures. As a consequence of these preliminary data several key questions need further delineation: (1) What is the ideal temperature for selective head cooling? (2) Which is the best mode of inducing hypothermia, ie, selective head versus total body cooling? (3) How long should hypothermia be maintained? (4) Will a multimo- 421 dal approach especially for the more severely affected infants be more effective than hypothermia alone? Oxygen Free Radical Inhibitors and Scavengers Since oxygen free radicals are considered important in the genesis of ongoing injury following hypoxia–ischemia, therapies targeted at the destruction of oxygen free radicals have been developed. Such strategies include the administration of specific antioxidant enzymes, ie, superoxide dismutase and catalase known to degrade highly reactive radicals to a nonreactive component. In newborn animals, neuroprotection has only been shown when these agents have been administered several hours before the hypoxic–ischemic insult.21,73 Specific free radical inhibition of xanthine production, ie, with allopurinol and oxypurinol (xanthine oxidase inhibitors) protects the immature rat from hypoxic–ischemic brain damage when the drugs are administered early during the recovery phase following resuscitation.21 In a recent clinical study, allopurinol administered to asphyxiated infants reduced blood concentrations of oxygen free radicals when compared with control infants.74 A third approach of free radical inhibition has targeted the formation of free radicals specifically hydroxyl radical from free iron during reperfusion.26 Thus, desferoxamine, a chelating agent, prevents the formation of free radical from iron, reduces the severity of brain injury and improves cerebral metabolism in animal models of hypoxia–ischemia when given during reperfusion.26,75 Excitatory Amino Acid Antagonists Given the important role of excessive stimulation of neuronal surface receptors by glutamate in promoting a cascade of events leading to cellular death,1,23 it has been logical to identify pharmacological agents that would either inhibit glutamate release or block its postsynaptic action. Glutamate receptor antagonists (ie, NMDA, AMPA subtypes) have been extensively investigated in experimental animals. Noncompetitive antagonists provided a reduction in brain damage in adult animals even when administered up to 24 hours after the insult. Available NMDA antagonists include dizocilpine (MK-801), magnesium, phencyclidine (PCP), dextrometrophan and ketamine.21 Relevant to the neonate, magnesium is an NMDA antagonist blocking neuronal influx of Ca2⫹ within the ion channel. Magnesium sulfate is an attractive agent because of its frequent use in the United States. It is often administered to mothers for tocolysis or to prevent seizures in mothers with pregnancy-induced hypertension. In developing brain, the potential effect of magnesium appears to be dependent on the maturation of the glutamate receptor system. Thus, in mice, excitotoxic neuronal death was limited by magnesium which was effective only after development of several aspects of the excitotoxic cascade, including the coupling of the calcium influx following NMDA over stimulation, and the presence of magnesium-dependent calcium channels.76 Additional experimental studies have revealed conflicting data. Thus, when administered shortly following J.M. Perlman 422 an intracerebral injection of NMDA, magnesium sulfate reduced brain injury in newborn rats. By contrast in a piglet model of asphyxia, magnesium sulfate administered 1 hour following resuscitation failed to decrease the severity of delayed energy failure. In addition, in a near-term fetal lamb model, magnesium sulfate administered before and during umbilical cord occlusion did not influence the electrophysiological responses or neuronal loss.21,77,78 Preliminary retrospective observations in premature infants note a reduced incidence of CP at 3 years in those exposed to antenatal magnesium sulfate79 A small randomized clinical study showed some subtle benefits, ie, on CT imaging and clinically as indicated by improved feeding at 14 days from magnesium infusion.80 Clearly, future research is necessary to determine the potential neuroprotective role of magnesium. Prevention of Nitric Oxide Formation The experimental effects of NOS inhibitors vary and are animal species specific and influenced by the pharmacological agent used, the dose and timing of therapy. Thus, in adult experiments, the severity of neuronal loss can be reduced by the prior administration of inhibitors of NOS activity. Although a similar protective effect has been observed in the immature rat, in fetal sheep, neuronal injury appears to be accentuated following hypoxia–ischemia.21 Calcium Channel Blockers The elevation of cytosolic calcium during and following hypoxic–ischemic injury makes the reduction of intracellular accumulation a highly desirable therapy. The use of calcium channel blockers, eg, flunarizine, has been studied in fetal and newborn animals and the neuroprotective effect has only been demonstrated when given before but not following hypoxic–ischemia.21 In a pilot study, nicardipine was tested in four severely asphyxiated infants but the positive effect was counteracted by the adverse effects of significant hemodynamic disturbance.81 Indeed, current calcium channel blocks are in general contraindicated in the neonate and young infant in the United States because of significant adverse cardiovascular effects. Other Potential Neuroprotective Avenues Other avenues of potential neuroprotection include platelet-activating factor antagonists,82 adenosinergic agents,83 monosialoganglioside GM1,84 growth factors, eg, nerve growth factor (NGF),85 insulin growth factor-186 and blocking the apoptotic pathways, ie, minocycline,87 erythropoeitin, etc.88,89 Summary Much progress has been made toward understanding the mechanisms contributing to ongoing brain injury following hypoxia–ischemia. This should facilitate more specific pharmacologic intervention strategies that might provide neuroprotection during the reperfusion phase of injury. Early identification of infants at highest risk for brain injury is critical if such interventions are to be successful. Conclusions Perinatal brain injury resulting in long-term neurodevelopmental deficits occurs most often as a consequence of intrapartum hypoxia–ischemia. Advances in the understanding of ongoing injury have facilitated the introduction of targeted neuroprotective strategies that may improve long-term outcome. Brain injury secondary to intracranial hemorrhage and/or focal cerebral infarction continues to be identified only at the time of symptoms greatly limiting attempts at prevention. Future studies need to focus on identifying highrisk infants that incorporate antepartum, intrapartum and postpartum strategies. References 1. Volpe JJ: Hypoxic–ischemic encephalopathy, in Volpe JJ (ed): Neurology of the Newborn. Philadelphia, PA, WB Saunders Company, 2001 2. Perlman JM: Intrapartum hypoxic-ischemic cerebral injury and subsequent cerebral palsy: Medico-legal issues. Pediatrics 99:851-859, 1997 3. Hannigan WC, Magbool BA, Cusack TJ, et al: Diagnosis of subdural hemorrhage in utero. Case Report J Neurosurg 63:977-979, 1985 4. Gunn TR, Mok PM, Becroft DMO: Subdural hemorrhage in utero. Pediatrics 76:605-610, 1985 5. Towbin A: Central nervous system damage in the human fetus and newborn infant. Mechanical and hypoxic injury incurred in the fetal– neonatal period. Am J Dis Child 199:529-542, 1970 6. Hayashi T, Hashimoto T, Fukuda S, et al: Neonatal subdural hematoma secondary to birth injury: Clinical analysis of 48 survivors. Child Nerv Syst 3:23-29, 1987 7. Chamnanvanakij S, Rollins N, Perlman JM: Subdural hematoma in term infants. Pediatr Neurol 26:301-304, 2002 8. Steinbok P, Haw CS, Cochrane DD, et al: Acute subdural hematoma associated with cerebral infarction in the full term neonate. Pediatr Neurosurg 23:206-215, 1995 9. Perlman JM: Neonatal cerebrovascular disorders, in Roach ES, Riela AR (eds): Pediatric Cerbrovascular Disorders. Armonk, NY, Futura Publishing Company, 1995, pp 267-290 10. Trounce JQ, Dodd KL, Fawer CL, et al: Primary thalamic hemorrhage in the newborn. A new clinical entity. Lancet 1:190-192, 1985 11. Roland EH, Flodmark O, Hill A: Thalamic hemorrhage with intraventricular hemorrhage in the full term neonate. Pediatrics 85:737-742, 1990 12. Lynch JK, Hirtz DG, DeVeber G, et al: Report of the National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. Pediatrics 109:116-123, 2002 13. Estan J, Hope P: Unilateral neonatal cerebral infarction in full term infants. Arch Dis Child Fetal Neonatal Ed 76:F88-F96, 1997 14. Perlman JM, Rollins NK, Evans D: Neonatal stroke: Clinical characteristics and cerebral blood flow velocity measurements. Pediatr Neurol 11:81-84, 1994 15. Ment CR, Duncan C, Erenkrantz RA: Perinatal cerebral infarction. Ann Neurol 16:559-568, 1984 16. Barmada MA, Mousby J, Shuman RM: Cerebral infarcts with arterial occlusion in neonates. Ann Neurol 6:495-502, 1979 17. Kraus FT, Acheen VI: Fetal thrombotic vasculopathy in the placenta: Cerebral thrombi and infarcts, coagulopathies, and cerebral palsy. Hum Pathol 30:759-769, 1999 18. Thorarensen O, Ryan S, Hunter J, et al: Factor V Leiden mutation: An Brain injury in the term infant 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. unrecognized cause of hemiplegic cerebral palsy, neonatal stroke, and placental thrombosis Ann Neurol 42:372-375, 1997 Mercuri E, Cowan F, Gupte G, et al: Prothrombotic disorders and abnormal neurodevelopmental outcome in infants with neonatal cerebral infarction. Pediatrics 107:1400-1414, 2001 Trauner DA, Mannino FL: Neurodevelopmental outcome after neonatal cerebrovascular accidents. J Pediatr 108:458-461, 1986 Vannucci RC, Perlman JM: Interventions for perinatal hypoxic-ischemic encephalopathy. Pediatrics 100:1004-1014, 1997 Wyatt JS, Edwards AD, Azzopardi D, et al: Magnetic resonance and near infrared spectroscopy for investigation of perinatal hypoxic-ischemic brain injury. Arch Dis Child 64:953-963, 1989 Grow J, Barks DE: Pathogenesis of hypoxic-ischemic cerebral injury in the term infant: Current concepts. Clin Perinatol 29:585-602, 2002 Lorek A, Takei Y, Cady EB, et al: Delayed (“secondary”) cerebral energy failure after acute hypoxia- ischemia in the newborn piglet: Continuous 48-hour studies by phosphorus magnetic resonance spectroscopy. Pediatr Res 36:699-706, 1994 Roth SC, Baudin J, Cady E, et al: Relation of deranged neonatal cerebral oxidative metabolism with neurodevelopmental outcome and head circumference at four years. Dev Med Child Neurol 39:718-725, 1997 Palmer C: Hypoxic-ischemic encephalopathy. Therapeutic approaches against microvascular injury, and role of neutrophils, PAF, and free radicals. Clin Perinatol 22:481-517, 1995 Hagberg H, Gilliaud E, Bona E: Enhanced expression of IL1 and IL6 m-RNA and bioactive proteins after hypoxia ischemia in neonatal rats. Pediatr Res 40:603-609, 1996 Bona E, Anderson AL: Chemokines and inflammatory cell response to hypoxia ischemia in immature rats. Pediatr Res 45:500-509, 1999 Eklind S, Mallard C, Leverin AL: Bacterial endotoxin sensitizes the immature brain to hypoxic ischemic injury. Eur J Neurosci 13:11011106, 2001 Hagan P, Barks GDE, Yabut M, et al: Adenovirus mediated over expression of IL1 receptor antagonist reduces susceptibility to excitotoxic brain injury in perinatal rats. Neuroscience 75:1033-1045, 1996 Yanasaki Y, Shoozurhara H, Onodera H, et al: Blocking of IL-1 activity is a beneficial approach to ischemia and brain edema formation. Acta Neurochir 60:S300-S302, 1995 Bruce AJ, Boling W, Kindy S: Altered neuronal and microglial responses to excitotoxic and ischemic brain injury in mice lacking TNF receptors. Nat Med 2:788-794, 1996 Loddick SA, Turnbill AV, Rothwell NJ: Cerebral interleukin 1 is neuroprotective against permanent focal ischemia in the rat. J Cereb Blood Flow Metab 18:176-179, 1998 Bonfold E, Krainc D, Ankarcrona M, et al: Apoptosis and necrosis: Two distinct events, induced respectively by mild and intense insults with N methyl-dospartate or nitric oxide/superoxide in cortical cell cultures. Proc Natl Acad Sci U S A 92:7162-7166, 1995 Edwards AD, Mehmet H: Apoptosis in perinatal hypoxic-ischemic cerebral damage. Neuropathol Appl Neurobiol 22:494-498, 1996 Sarnat HB, Sarnat MS: Neonatal encephalopathy following fetal distress. Arch Neurol 33:696-705, 1976 Huppi PS: Advances in postnatal neuroimaging: Relevance to pathogenesis and treatment of brain injury. Clin Perinatol 29:827-856, 2002 Ment LR, Bada HS, Barnes P, et al: Practice parameter: Neuroimaging of the neonate: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 58:1726-1738, 2002 Cowan FM, Pennock JM, Hanrahan JD, et al: Early detection of cerebral infarction and hypoxic ischemic encephalopathy in neonates using diffusion-weighted magnetic resonance imaging. Neuropediatrics 25: 172-175, 1994 Albers GW, Lansberg MG, Norbash AM, et al: Yield of diffusionweighted MRI for detection of potentially relevant findings in stroke patients. Neurology 54:1562-1567, 2000 Groenendaal F, Veenhoven RH, van der Grond J, et al: Cerebral lactate and N-acetyl-aspartate/choline ratios in asphyxiated full-term neonates demonstrated in vivo using proton magnetic resonance spectroscopy. Pediatr Res 34:148-151, 1994 423 42. Hanrahan JD, Cox IJ, Edwards AD, et al: Persistent increases in cerebral lactate concentration after birth asphyxia. Pediatr Res 44:308-311, 1998 43. Perlman JM, Risser R: Can asphyxiated infants at risk for neonatal seizures be rapidly identified by current high-risk markers? Pediatrics 97:456-462, 1996 44. Hellstrom-Westas L, Rosen I, Svenningsen NW: Predictive value of early continuous amplitude integrated EEG recordings on outcome after severe birth asphyxia in full term infants. Arch Dis Child 72:F34F38, 1995 45. al Naqeeb N, Edwards AD, Cowan FM, et al: Assessment of neonatal encephalopathy by amplitude-integrated electroencephalography. Pediatrics 103:1263-1269, 1999 46. Shalak L, Corbett R, Laptook AR, et al: Amplitude-integrated electroencephalography coupled with an early neurologic examination enhances prediction of term infants at risk for persistent encephalopathy. Pediatrics 111:351-357, 2003 47. Dzhala V, Ben-Ari Y, Khazipov R: Seizures accelerate anoxia-induced neuronal death in the neonatal rat hippocampus. Ann Neurol 48:632640, 2000 48. Holmes GL, Gairsa JL, Chevassus-Au-Louis N, Ben-Ari Y: Consequences of neonatal seizures in the rat: Morphological and behavioral effects. Ann Neurol 44:845-857, 1998 49. Mizrahi EM: Consensus and controversy in the clinical management of neonatal seizures. Clin Perinatol 16:485-500, 1989 50. Scher MS, Aso K, Beggerly ME, et al: Electrographic seizures in preterm and full term infant’s neonates: Clinical correlates associated brain lesions and risk for neurologic sequelae. Pediatrics 91:128-134, 1993 51. Goldberg RN, Moscoso P, Bauer CR, et al: Use of barbiturate therapy in severe perinatal asphyxia: A randomized controlled trial. J Pediatr 109: 851-856, 1986 52. Hall RT, Hall FK, Daily DK: High-dose phenobarbital therapy in term newborn infants with severe perinatal asphyxia: A randomized prospective study with three-year follow-up. J Pediatr 132:345-348, 1998 53. Minamisawa H, Smith ML, Siesjo BK: The effects of mild hyperthermia and hypothermia on brain damage following 5, 10, and 15 minutes of forebrain ischemia. Ann Neurol 28:26-33, 1990 54. Yager J, Towfighi, Vannucci RC: Influence of mild hypothermia on hypoxic-ischemic brain damage in the immature rat. Pediatr Res 35: 525-529, 1993 55. Laptook AR, Corbett RJT, Sterett R, et al: Modest hypothermia provides partial neuroprotection for ischemic neonatal brain. Pediatr Res 35: 436-442, 1994 56. Thorensen M, Bagenholm R, Loberg EM, et al: Posthypoxic cooling of neonatal rats provides protection against brain injury. Arch Dis Child 74:F3-F9, 1996 57. Gunn AJ, Gunn TR, de Haan HH, et al: Dramatic neuronal rescue with prolonged selective head cooling after ischemia in fetal lambs. J Clin Invest 99:248-256, 1997 58. Gunn AJ, Gunn TR, Gunning MI: Neuroprotection with prolonged head cooling started before postischemic seizures in fetal sheep. Pediatrics 102:1098-1106, 1998 59. Gunn AJ, Bennet L, Gunning MI, et al: Cerebral hypothermia is not neuroprotective when started after post ischemic seizures in fetal sheep. Pediatr Res 46:274-280, 1999 60. Gunn AJ: Cerebral hypothermia for prevention of brain injury following perinatal asphyxia. Curr Opin Pediatr 12:111-115, 2000 61. Colbourne F, Sutherland G, Corbett D: Postischemic hypothermia: A critical appraisal with implications for clinical treatment. Mol Neurobiol 14:171-201, 1997 62. Edwards AD, Wyatt JS, Thoresen M: Treatment of hypoxic-ischemic brain damage by moderate hypothermia. Arch Dis Child Fetal Neonatal Ed 78:F85-F91, 1998 63. Laptook AR, Corbett RJT: Therapeutic hypothermia: A potential neuroprotective and resuscitative strategy for neonatal hypoxia-ischemia. Prenat Neonat Med 1:199-212, 1996 64. Towfighi J, Housman C, Heitjan DF, et al: The effect of focal cerebral cooling on perinatal hypoxic-ischemic brain damage. Acta Neuropathol 87:598-604, 1994 424 65. Laptook AR, Corbett RJT: The effects of temperature on hypoxic-ischemic brain injury. Clin Perinat. 29:623-629, 2002 66. Marion DW, Penrod LE, Kelsey SF, et al: Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med 336:540-546, 1997 67. Bernard SA, Gray TW, Buist MD, et al: Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 346:557-563, 2002 68. Hypothermia after cardiac arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 346:549-556, 2002 69. Laptook AR, Shalak L, Corbett RJT: Differences in brain temperature and cerebral blood flow during selective head versus whole-body cooling Pediatrics 108:1103-1110, 2001 70. Thoresen M, Whitelaw A: Cardiovascular changes during mild therapeutic hypothermia and rewarming in infants with hypoxic-ischemic encephalopathy. Pediatrics 106:92-99, 2000 71. Gunn AJ, Gluckman PD, Gunn TR: Selective head cooling in newborn infants after perinatal asphyxia. A safety study. Pediatrics 102:885-892, 1998 72. Azzopardi D, Robertson NJ, Cowan FM, et al: Pilot study of treatment with whole body hypothermia for neonatal encephalopathy. Pediatrics 106:684-694, 2000 73. Shimizu K, Rajapakse N, Horiguchi T, et al: Neuroprotection against hypoxia-ischemia in neonatal rat brain by novel superoxide dismutase mimetics. Neurosci Lett 346:41-44, 2003 74. Van Bel F, Shadid M, Moison RM, et al: Effect of allopurinol on postasphyxial free radical formation, cerebral hemodynamics and electrical brain activity. Pediatrics 101:185-193, 1998 75. Peeters-Scholte C, Braun K, Koster J, et al: Effects of allopurinol and desferoxamine on reperfusion injury of the brain in newborn piglets after neonatal hypoxia-ischemia. Pediatr Res 54:516-522, 2003 76. Marret S, Gressens P, Gadisseux JF, et al: Prevention by magnesium of excitotoxic neuronal death in the developing brain: An animal model of clinical intervention studies. Dev Med Child Neurol 37:473-484, 1995 77. Penrice J, Amess PN, Punwani S, et al: Magnesium sulfate after transient hypoxia-ischemia fails to prevent delayed cerebral energy failure in the newborn piglet. Pediatr Res 41:443-447, 1997 J.M. Perlman 78. de Haan HH, Gunn AJ, Williams CE, et al: Magnesium sulfate therapy during asphyxia in near-term fetal lambs does not compromise the fetus but does not reduce cerebral injury. Am J Obstet Gynecol 176: 18-27, 1997 79. Nelson KB, Grether JK: Can magnesium sulfate reduce the risk of cerebral palsy in very low birth weight infants? Pediatrics 95:263-269, 1995 80. Ischiba H: Randomized controlled trial of magnesium sulfate infusion for severe birth asphyxia Pediatr Int 44:505-509, 2002 81. Levene MI, Gibson NA, Fenton AC, et al: The use of a calcium-channel blocker, nicardipine, for severely asphyxiated newborn infants. Dev Med Child Neurol 32:567-574, 1990 82. Liu XH, Eun BL, Silverstein FS, et al: The platelet-activating factor antagonist BN 52021 attenuates hypoxic-ischemic brain injury in the immature rat. Pediatr Res 40:797-803, 1996 83. Halle JN, Kasper CE, Gidday JM, et al: Enhancing adenosine A1 receptor binding reduces hypoxic-ischemic brain injury in newborn rats. Brain Res 759:309-312, 1997 84. Tan WK, Williams CE, Mallard CE, et al: Monosialoganglioside GM1 treatment after a hypoxic-ischemic episode reduces the vulnerability of the fetal sheep brain to subsequent injuries. Am J Obstet Gynecol 170:663-669, 1994 85. Holtzman DM, Sheldon RA, Jaffe W, et al: Nerve growth factor protects the neonatal brain against hypoxic-ischemic injury. Ann Neurol 39: 114-122, 1996 86. Johnston BM, Mallard EC, Williams CE, et al: Insulin-like growth factor-1 is a potent neuronal rescue agent after hypoxic-ischemic injury in fetal lambs. J Clin Invest 97:300-308, 1996 87. Arvin K, Han BH, Du Y, et al: Minocycline markedly protects the neonatal brain against hypoxic-ischemic injury. Ann Neurol 52:54-61, 2002 88. Aydin A, Genc K, Akhisaroglu M, et al: Erythropoietin exerts neuroprotective effect in neonatal rat model of hypoxic-ischemic brain injury Brain Dev 25:494-498, 2003 89. Kumral A, Ozer E, Yilmaz O, et al: Neuroprotective effect of erythropoietin o/ hypoxic-ischemic brain injury in neonatal rats. Biol Neonate 83:224-228, 2003